The coconut (Cocos nucifera) is a monocotyledon plant belonging to the Aracaceae family. Although potentially severe, there are few allergic processes described that arise from ingestion of its fruit, although the majority of cases described to date have been anaphylactic reactions.1–7,10 The endosperm is the edible part of the fruit, and it is composed of 25% albumins and 75% globulins, the latter of which contains the proteins which have been implicated in allergic reactions, such as Coc n2, 7S globulin, and Coc n4, 11S globulin (known as cocosin). Under native conditions, molecular masses of the 7S and 11S globulins are 156kDa and 326kDa respectively, and the 7S globulin is composed of three protein subunits of 24kDa, 22kDa, and 16kDa while the 11S globulin is composed of 55kDa, 34kDa, and 24kDa subunits.8
Cross reactivity between coconuts, walnuts, hazelnuts and lentils has been described, and this is due to 7S and/or 11S globulins.1,4,6,7 Similarly, cases of monosensitization to coconut have been described.2,3,5
Here we describe the case of a 12 and a half-year-old child with asthma and rhinitis caused by allergies which are being controlled with immunotherapy. The child is sensitized to Dermatophagoides farinae and Dermatophagoides pteronyssinus, Alternaria and dog and cat epitheliums, and has presented anaphylaxis from ingestion of crustaceans. At 12 years old, 10min after ingesting a piece of coconut for the first time, the child presented an allergic reaction which lasted for an hour and consisted of spasmodic coughing, sneezing outbursts, rhinorrhea, vomiting, and difficulty in breathing with thoracic oppression and wheezing.
To investigate this coconut allergy, skin prick tests were performed with commercial extracts and the following mean wheal diameters were found: coconut, 14mm, walnut and hazelnut, 5mm, sesame, 6mm and date, 3mm with erythema. The histamine dihydrochloride (10mg/ml) value detected was 7mm.
Protein extracts, fresh coconut and coconut milk were prepared by homogenization in phosphate-buffered saline, dialization, and lyophilization. Serum specific immunoglobulin (Ig) E levels were measured using the enzyme allergosorbent technique (Specific IgE EIA kit HYTEC HYCOR Biomedical Ltd). Determination of serum specific IgE revealed the following values: fresh coconut, 0.6kUA/L, and coconut milk, 1kUA/L. Values detected against extracts from sesame, walnut and peanut were between 0.35 and 0kUA/L. Specific IgE against date extract was <0.35kUA/L.
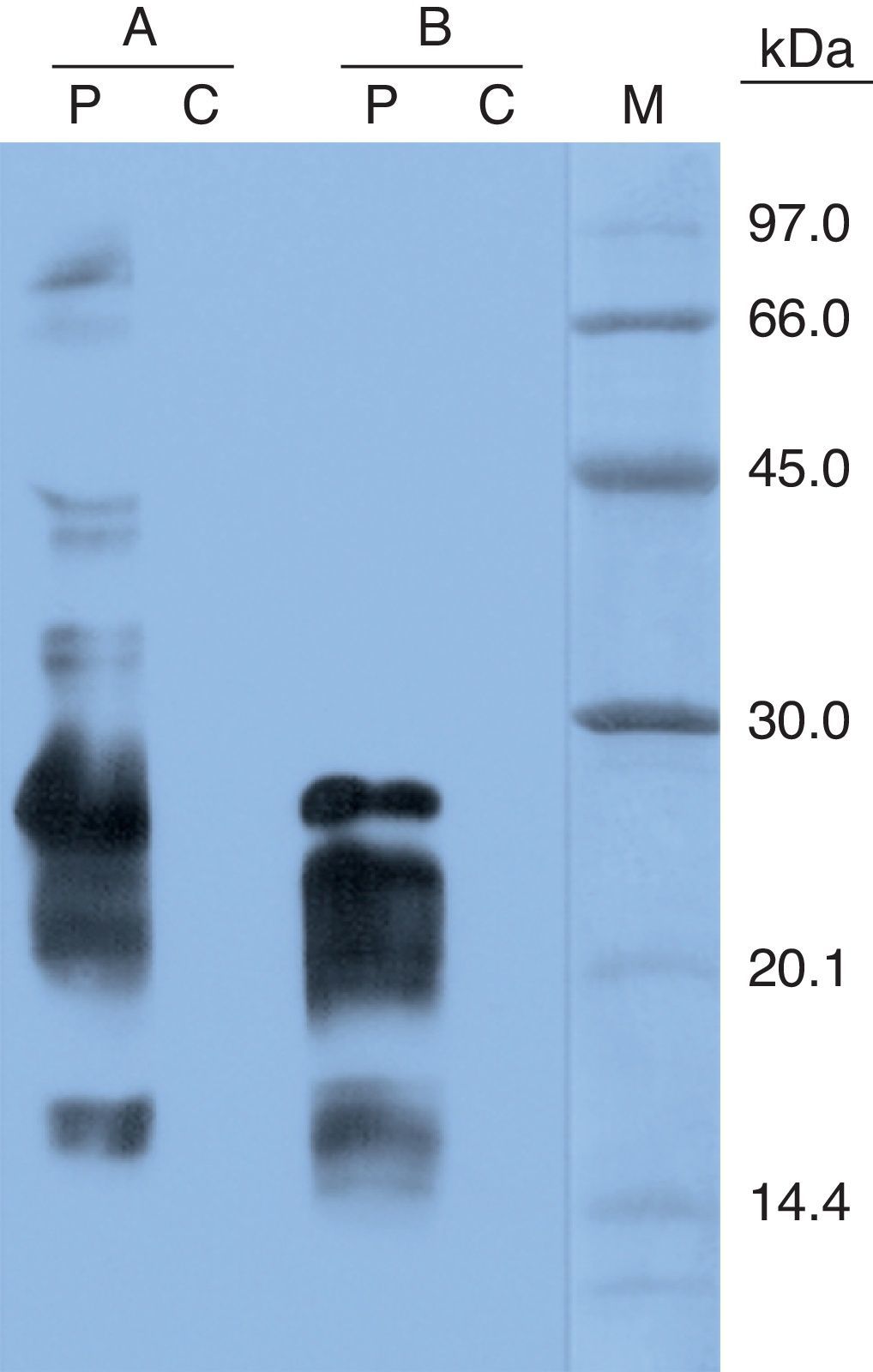
Sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE) IgE immunoblotting revealed intense IgE binding bands at 27kDa, 16kDa, and a broad one between 20 and 25kDa in both coconut extracts; some other faint bands were only detected in the fresh coconut extract at 80kDa, 66kDa, 39kDa and 32/33kDa (Fig. 1).
Finally, an open oral provocation test9 against walnut, hazelnut, sesame and date (foods whose tolerance were not known and to which sensitization was demonstrated in skin tests) was performed, and the result was negative. A provocation test against coconut was not performed as there was the danger of an anaphylactic reaction and the family denied authorization to perform the test.
Nine cases of coconut allergy have been reported, all of which produce anaphylactic reactions,1–7,10 and four of which were in children.3,4,6,7 In four of the cases, the 11S globulin was identified as the principal agent responsible for the allergic process,1,2,4 in two of the cases it was the 7S globulin,6 and in one of the cases both proteins were implicated in the allergic reaction.7
The molecular masses of the most intense bands detected in this study coincide with the molecular masses described for the 7S globulin protein subunits, and this suggests that this protein is involved in the allergic process of this patient. A less intense band of approximately 80kDa was also detected, and one with a similar molecular mass has been described in some cases of monosensitization to coconut.2,6
In this case it was verified that the patient could tolerate ingestion of tree nuts (walnuts and hazelnuts), sesame seeds and dates, all of which had produced sensitization, and thus this is the second case described where there is an allergic reaction (anaphylactic) caused exclusively by ingestion of coconut in a child. The first case was of a 3-year-old child.3 The provocation results obtained, as well as low IgE specific values detected against walnut, sesame and date extracts lead us to believe that sensitization to these foods is due to cross reactive phenomena with coconut proteins, as has been shown in other cases.1,4,6,7
In the last few years, the presence of molecules derived from coconuts has increased significantly in the food industry due to the use of coconut oil. Similarly, oil from oil palm, Elaeis guineensis, is also used in industry and the 7S globulin from the oil palm fruit is homologous to the 7S globulin from coconuts.8 Oils from both are also widely used in the cosmetic industry, where these oils can be found in 44–76% of skin products (protective creams, soaps, body lotions, shampoos, etc.).11
It has been suggested that sensitization to proteins from certain foods such as coconuts could be due to topical exposure through the skin. Whether it is through this route or the oral route by ingestion of foods containing products derived from coconuts, it is very probable that exposure to coconut proteins is now occurring from very early ages and thus the risk of sensitization to this fruit could facilitate an increase in allergic reactions to coconuts in the coming years.
In summary, we present a case of anaphylaxis in a child due to ingestion of coconut, and it is very probable that 7S globulin is the principal protein implicated in this allergic process.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this article.
Data confidentialityThe authors declare that no patient details appear in this article.
Privacy rights and informed consentThe authors declare that no patient details appear in this article.
Conflicts of interestWe declare that we do not have any financial or personal relationship with regard to the submitted publication.