The vein of Galen aneurysmal malformation (VGAM) is an extremely rare arterio-venous malformation. The VGAM clinical manifestations vary depending on the magnitude of vascular compromise and the age at initial presentation. Neonates typically present with severe congestive heart failure. Here we present a case in which a systolic heart murmur was the first manifestation of high output heart failure due to a VGAM.
Las malformaciones de la vena cerebral de Galeno (MVG) son extremadamente raras. Sus manifestaciones clínicas varían dependiendo de la magnitud del compromiso vascular y la edad inicial de presentación. En neonatos, típicamente se presenta con una insuficiencia cardiaca congestiva grave. Se presenta un caso en el cual un soplo sistólico cardiaco fue la primera manifestación de una insuficiencia cardíaca de gasto alto secundaria a una malformación aneurismática de la vena de Galeno.
The vein of Galen (VG) is a small, thin-walled blood vessel (1cm path length) considered a deep/internal cerebral vein. The internal cerebral veins are anatomically formed by the union of the thalamostriate vein and the choroid vein at the interventricular foramen. Along its extention, the VG flexes upwards from the splenium of corpus callosum, continues into the anterior extremity of the sinus rectus, and receives the basal occipital, basal internal and superior callous veins.1
The vein of Galen aneurysmal malformation (VGAM) was initially described by Jaeger et al. in 1937.1 VGAM accounts for < 1% of intracranial arteriovenous malformations and approximately 30% of vascular intracranial anomalies in pediatric patients.2,3 VGAM results from the persistence of the embryonic proencephalic vein of Markowski, which normally regresses between the 6th and 11th weeks of development.4 VGAM generates an arteriovenous shunt that can lead to heart failure, pulmonary hypertension, intraventricular hemorrhage and hydrocephaly, depending on the magnitude of vascular compromise.3
In recent years the evaluation for VGAM has steadily advanced, allowing for prenatal detection in most cases. However, some cases, like the one presented here, present atypically, and are a challenge to diagnose.
Case reportOur patient is the product of a 39-week gestation born to a 21-year old woman. Her past relevant medical history included only a previous vaginal delivery. She was evaluated regularly during this pregnancy and had no symptoms. Screens for syphilis and HIV were negative and two obstetric ultrasounds were normal. She developed pregnancy-induced hypertension in the final three weeks of the pregnancy, with no other complications.
Vaginal delivery was without complications. The newborn was a 39-week old male with a good Apgar score (8/10 one minute and 9/10 five minutes after birth). However, 12hours after birth the newborn showed perioral cyanosis, exacerbated with crying and suctioning. He needed oxygen administration (1 L/min) to improve his oxygen saturation (from 80% to 98%). On examination at that time, the newborn weighed 3440g, with 51cm height, 34cm cephalic circumference, 29cm abdominal circumference, and 31cm thoracic perimeter. He was noted to have a systolic murmur (III/VI-grade) with highest intensity at the left upper sternal border. No other anomalies were found.
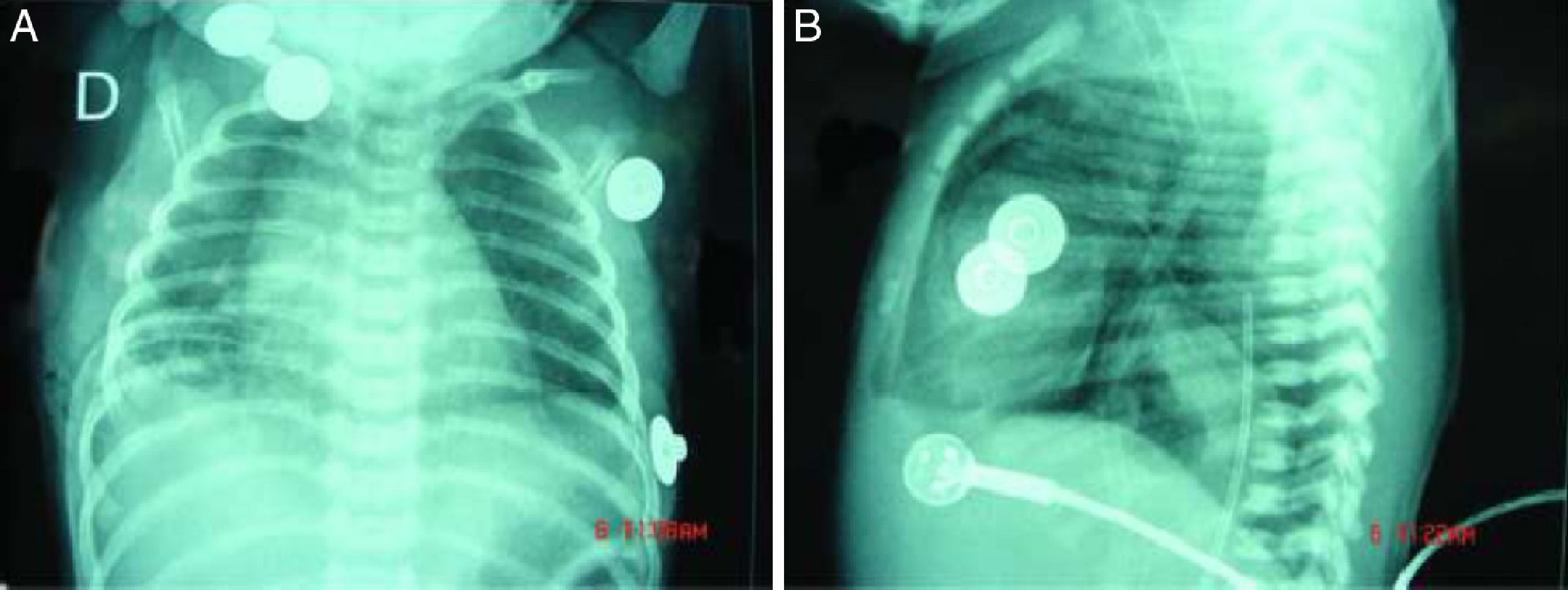
Radiography of the chest demonstrated a cardiothoracic index of 3.9 (Fig. 1). Echocardiogram revealed a dilated right ventricle with moderate functional tricuspid, pulmonary hypertension (80% systemic), a small patent foramen ovale and ductus arteriosus, and bi-directional shunting with predominant left to right flow.
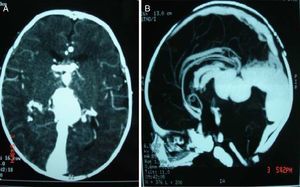
The newborn was admitted to the intensive care unit, but rapidly deteriorated becoming hypoactive and hypotonic, with poor suction, incomplete Moro and grasp reflexes and intolerance to oral feeding. Thoracoabdominal computed tomography (CT) scan showed right predominance cardiomegaly, augmented pulmonary artery size, and persistent ductus arteriosus. Transfontanellar ultrasonography and CT scans showed a rounded cystic dilated structure in the back of the third ventricle and above the cerebellum with high vascular flow; this is compatible with VGAM that has dilated neighboring vascular structures (internal cerebral veins). Multiple vascular structures were found communicating not only with the VGA, but also with the anterior cerebral arteries, pericallosal artery, as well as a branch of the posterior cerebral artery. There was also prominence of the circle of Willis, cerebral arteries, and basilar artery, resulting from VGAM (Fig. 2). No other anomalies were found.
The VGAM was embolized with microparticles through an endovascular procedure by transvenous route.
Under general anesthesia, a 0.018-inch guidewire was placed via an umbilical approach, within a 4Fr guiding catheter. A 0.014-inch Transend® Ex Floppy microguide wire was then navigated through a 1.7Fr Excelsior® SL-10 microcatheter to the branches from the bilateral anterior choroidal arteries. After the malformation was embolized using N-butyl cyanoacrylate (NBCA), the flow through the fistula was significantly reduced, allowing the infant to regain normal hemodynamic parameters. The patient experienced progressive resolution of his symptoms and within 2-weeks no longer required oxygen or other supportive measures. He currently is asymptomatic, with age-appropriate development, at 10 months after treatment.
DiscussionVGAM are divided into two groups: aneurysmatic dilations and malformations.4 VGAMs have direct communication between the choroidal or mural arteries and the VG. Choroidal malformations lead to mild to severe cardiac failure, cerebral atrophy, convulsions, or hepatomegaly in neonates.5The clinical manifestations of VGAM vary depending on age at clinical debut and other factors. In neonates, like our case, the most common clinical presentations related to heart failure are cyanosis, tachycardia and bounding carotid pulses.6–8
The heart failure developed as a result of VGAM can exhibit different grades, and its clinical manifestations depend on its severity. Some cases, such as this one, have a moderate compromise resulting in overlooked clinical manifestations. Therefore a thorough clinical examination can be the cornerstone in the diagnosis of this rare anomaly.
The medical confirmation of this congenital anomaly is through ultrasound studies or magnetic resonance imaging, in many cases allowing prenatal detection. In some studies, a mid-cerebral-line cystic lesion is visible,7,9 but in some cases, as presented here, this malformation could be unseen. However, VGAM can go undetected despite appropriate prenatal screening, and early detection and treatment after birth can prevent complications. In this case, the first manifestation was a (III/VI-grade) systolic murmur, a simple clinical sign that can encourage evaluation for evidence of heart failure, which may otherwise be unexplained. This can lead to earlier diagnosis, rapid treatment, and prevention of brain damage and other complications such as intracranial hemorrhage and hydrocephaly.7
Vascular embolization is the therapy that has so far shown to be the most effective. It consists of percutaneous arterial and venous embolization guided by micro-catheters, mostly via the umbilical artery. Once the morphologic anomaly is detected, N-butyl-cyanoacrylate (NBCA) injection or other embolic agents are administered by means of radio-opaque agents.10–12 These endovascular advancements have markedly improved the prognosis of VGAM in the past few years. In 1964, Gold et al. reported a 100% mortality among neonates with VGAM.13 By 2003, Fullerton et al. reported a mortality rate of only 15% due to new options in the treatment for this condition.14
In conclusion, we report a difficult case in which an appropriate clinical approach allowed rapid treatment, consequently resulting in reversal of severe heart failure and a favorable outcome for the patient.
FundingThis manuscript was supported with personal funding.
Conflict of interestThere are no conflicts of interest to disclose.
Authors would like to thank Dr. Michael Y. Choi for data preparation.