Mesenteric venous thrombosis is a rare cause of acute abdomen, representing only 5%–15% of cases of acute mesenteric ischemia.1 Its diagnosis is difficult if not accompanied by clinical suspicion.
Factor V (proaccelerin) is a co-enzyme that acts on factor X of the blood coagulation cascade, enabling it to activate thrombin, which interacts with fibrinogen to convert it into fibrin, a main component involved in blood clotting. Under normal conditions, activated C protein inhibits the action of factor V. Leiden mutation is a variation of factor V that makes it insensitive to activated C protein, producing a state of hypercoagulability.2 Factor V Leiden mutation is the most frequent cause of thrombophilia in Caucasians, and its prevalence without a history of thrombosis is 2%–7%, which increases to 20%–50% in patients with venous thrombosis.
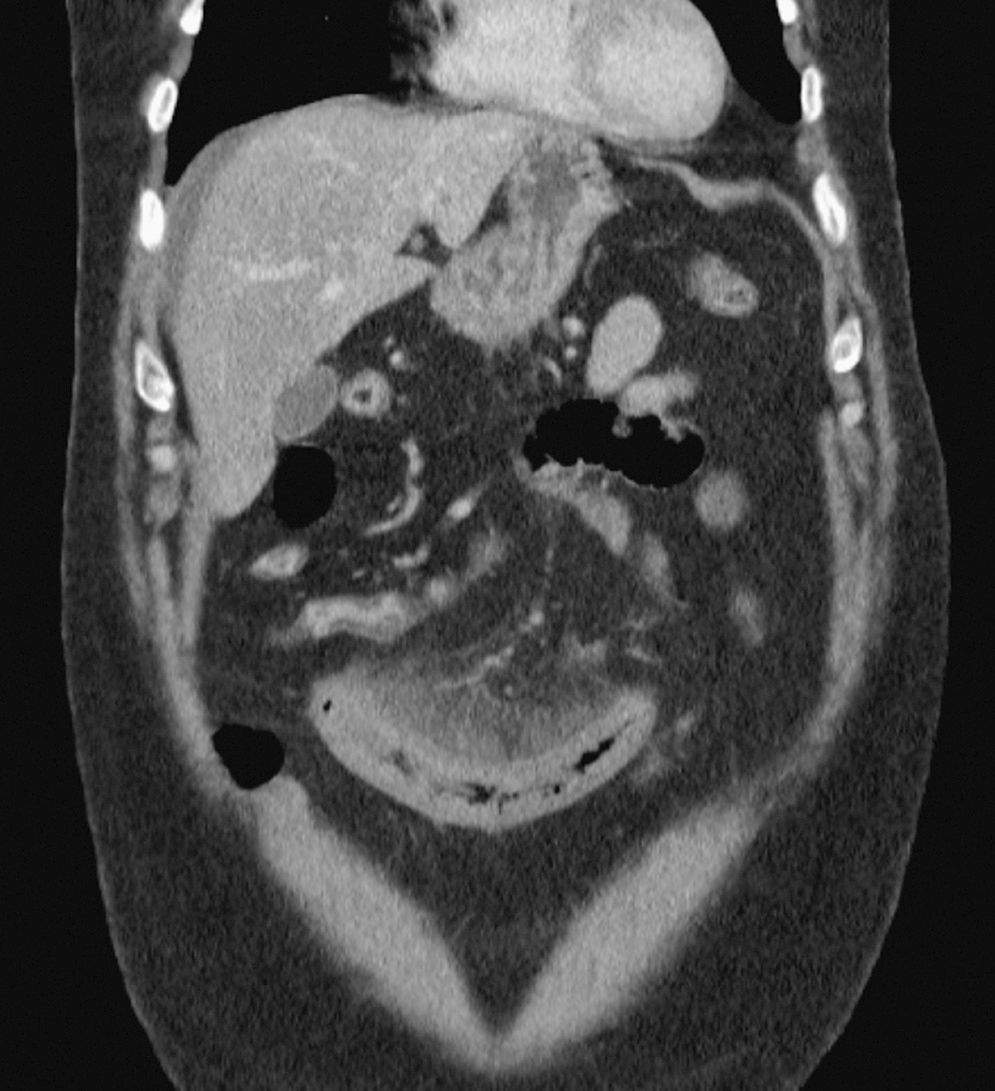
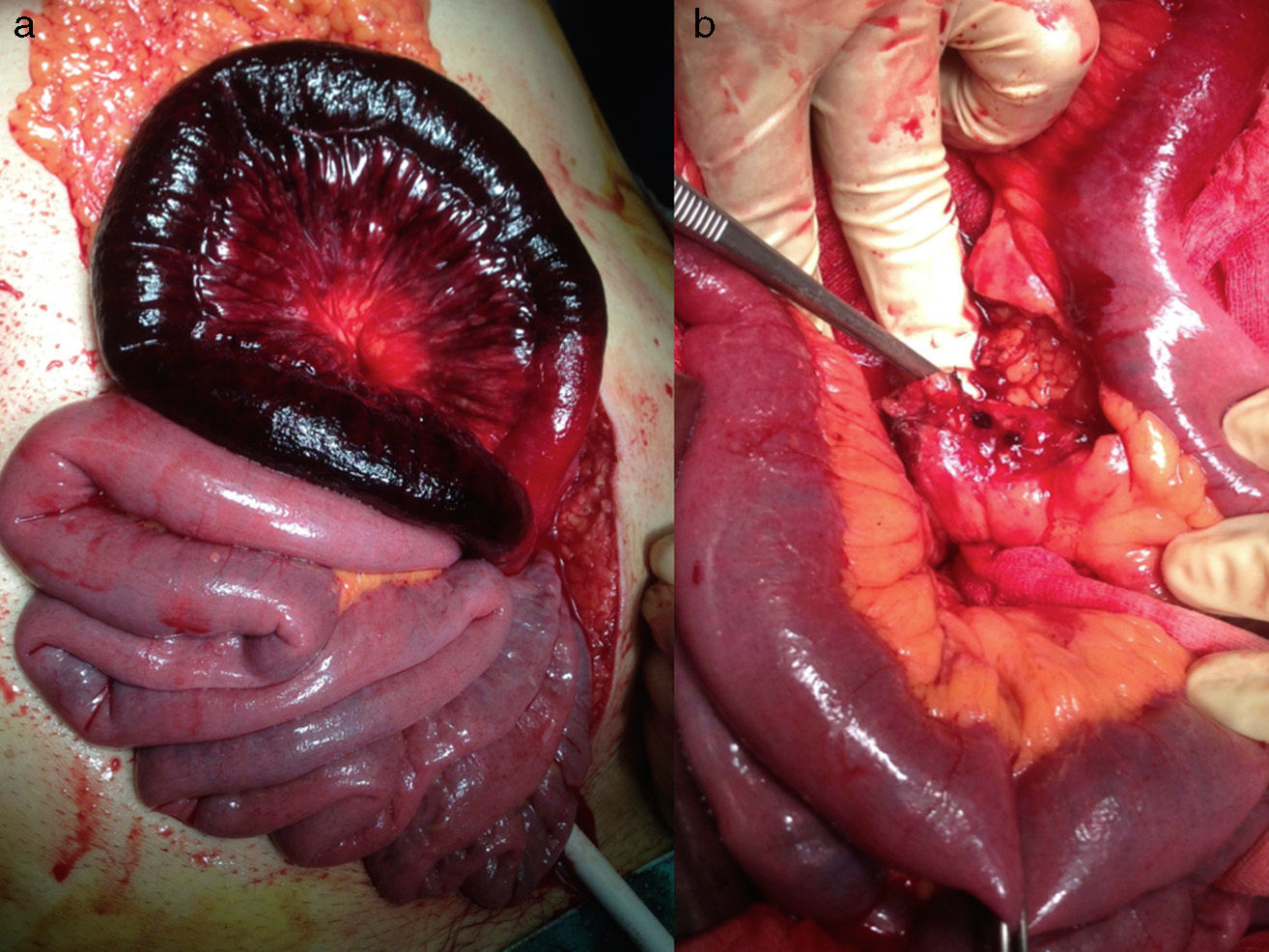
We present the case of a 55-year-old male patient with a history of obesity (body mass index 30.6kg/m2), deep vein thrombosis of the lower extremities and heterozygous for factor V Leiden, who came to the emergency room due to vomiting and sudden-onset diffuse abdominal pain for one week that was associated with diarrhea but no bleeding. He had been on a diet during the previous 6 weeks and had lost 6kg. Upon physical examination, the patient had no fever and was haemodynamically stable, although he was pale and perspiring, with diffuse abdominal pain and distension, absence of peristalsis and guarding upon palpation. His workup showed leukocytosis with neutrophilia (92%), hemoglobin 13.9g/dL, glucose 181mg/dL, creatinine 1.1mg/dL, CK 56U/L, amylase 70U/L and CRP 7.9mg/dL. Simple radiographs of the chest and abdomen were normal. An emergency computed tomography (CT) scan revealed thrombosis of the superior mesenteric vein and branches, along with congestive small bowel loops with wall thickening, rarefaction of the fat at the mesenteric root, and free fluid. The spleno-portal axis was permeable, and no pneumatosis or pneumoperitoneum were observed (Fig. 1). Emergency surgery revealed ischemia of a 60cm section of the jejunum (Fig. 2a), which was resected and reconstructed with manual end-to-end anastomosis. After division of the mesojejunum, we observed thrombosis of the mesenteric vessels (Fig. 2b). During the immediate postoperative period, the patient received anticoagulation therapy with heparin at a daily dose of 6000IU according to the patient's weight; he was monitored by the hematology unit until his discharge 6 days later.
Intestinal ischemia secondary to venous thrombosis is more difficult to diagnose and treat than arterial thrombosis, which usually has an insidious course and nonspecific clinical signs.3 The altered venous return causes edema of the intestinal wall, affected microvascular perfusion, loop distension and, finally, infarction of the affected bowel. Mesenteric venous thrombosis is frequently secondary to other processes like neoplasms, hypercoagulability syndromes, pancreatitis, abdominal trauma, severe dehydration or polycythaemia vera.4
In our case, the main risk factor was factor V Leiden mutation, which increases the risk for thrombosis between 7 and 80 times depending on whether it is heterozygous (50% altered factor V) or homozygous (100%), and obesity was an additional risk. Other influential circumstances are oestrogens (contraception, pregnancy), antiphospholipid antibody or smoking.5
The diagnosis of mesenteric venous thrombosis is often delayed and based on clinical suspicion and CT studies with intravenous contrast in arterial and venous phases, whose findings correlate with the severity of the process.6 Frequent findings include the vascular thrombosis itself, or indirect signs of intestinal complications, such as segmental thickening of the bowel wall, intestinal pneumatosis, portal venous gas, free fluid or increased uptake of the mesenteric fat.
The therapeutic objective, in addition to support measures and antibiotic therapy, is to re-establish the venous blood flow. The treatment of choice is early anticoagulation with unfractionated heparin,7 and surgery is indicated in patients with peritoneal irritation or suspicion of intestinal ischemia. Heparinisation can be stopped or reverted with protamine if reoperation is necessary. In our case, anticoagulation was initiated in the immediate postoperative period and continued after discharge.
In the cases with Leiden mutation, anticoagulation is not recommended for life unless there have been 2 episodes of thrombosis or other associated risk factors. The most important prognostic factor in mesenteric venous thrombosis is the duration of the symptoms before diagnosis. In the study by Alvi et al.,1 patients with more than 3 days of symptoms presented a higher need for laparotomy (83 vs 20%; P=.018) and higher mortality (50 vs 7%; P=.06).
In conclusion, mesenteric venous thrombosis is a disease to consider in the differential diagnosis of acute abdomen in patients that present states of hypercoagulability. CT scan is the test of choice for early diagnosis, and the main treatment is anticoagulation, although surgery is indicated if there is peritonism or signs of ischemia.
Conflict of InterestsThe authors declare having no conflict of interests.
Please cite this article as: Sánchez Corral J, Martínez Casas I, Huertas Riquelme JL, David Alvarado J, Camacho Lozano J. Isquemia mesentérica aguda por trombosis venosa en paciente portador de mutación Leiden del factor V. Cir Esp. 2015;93:672–674.