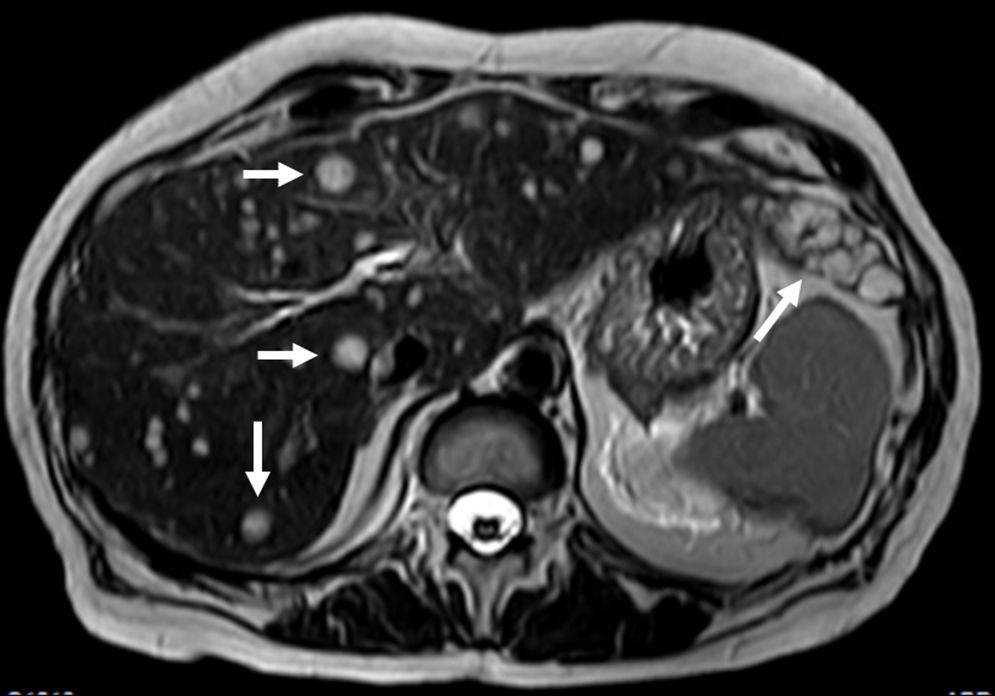
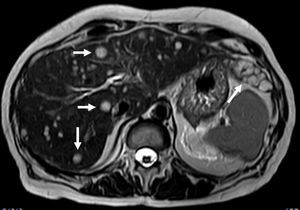
A 60-year-old woman with past medical history of chronic pancreatitis and bilioenteric anastomosis was referred to our institution for routine unenhanced pancreatic MR evaluation. Besides the expected findings of uncomplicated chronic pancreatitis, the study revealed several focal lesions distributed through the liver, suggestive of metastases. They were hypointense in T1 imaging and remarkably hyperintense in T2-weighted images (Fig. 1). Blood tests where mostly unexceptional, only revealing elevated gamma-glutamyl transferase [88U/L (normal: 5–36U/L)].
A liver biopsy was performed and, despite the obtention of only a small amount of diagnostic material, it was still possible to exclude carcinomatous, neuroendocrine and hepatocytary origin and to detect positivity for CD34, a marker present in tumors of hematopoietic or endothelial lineage.1
PET-CT was also realized for staging, demonstrating multiple slightly hypermetabolic liver lesions and significant hypermetabolism centered in the left aryepiglottic fold. After biopsy the neck lesion was diagnosed as squamous-cell carcinoma, non-related to the liver lesions. Neck MRI staging revealed invasion of the ipsilateral piriform sinus and the presence of an ipsilateral level IV necrotic lymph node (TNM: T2,N1,M0).
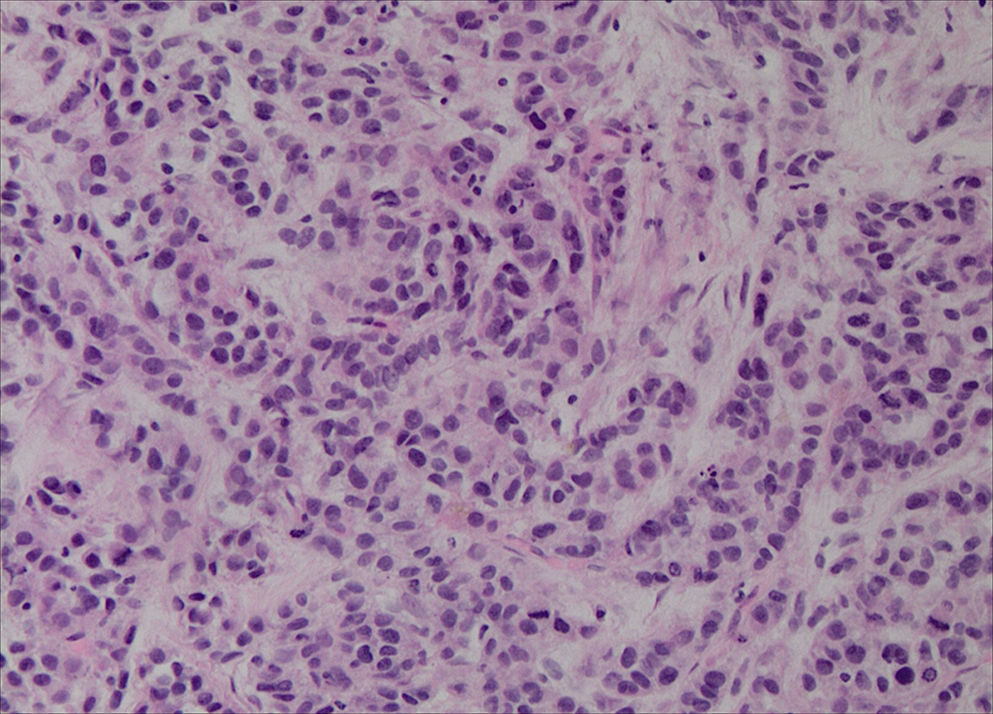
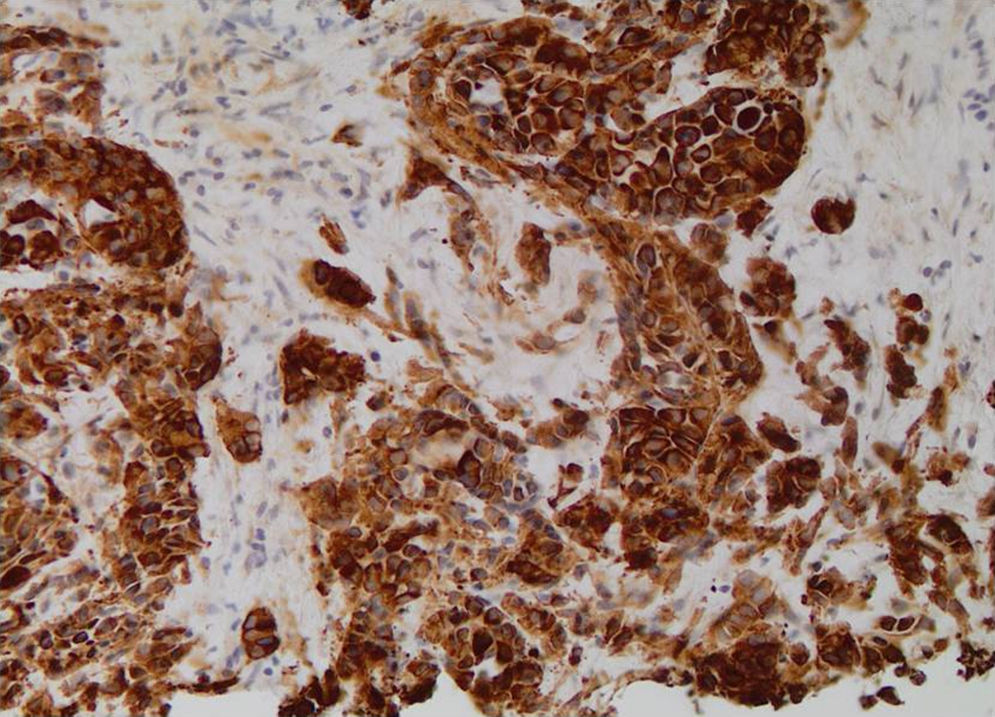
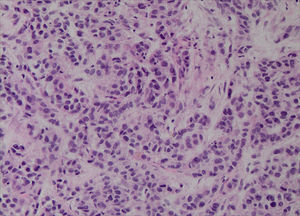
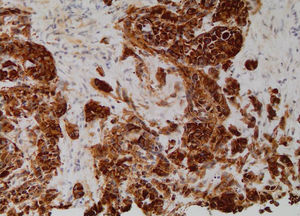
With these results the possibility of a primary, multifocal, vascular liver malignancy started to gain strength and another liver biopsy was taken. The samples were representative and histological analysis revealed the presence of nests of epithelioid cells (Fig. 2); the immunohistochemical tests detected positivity for anti-cytokeratin marker (CK OSKAR®), again suggesting the epithelial nature of the lesion (Fig. 3). Altogether, the findings of both biopsies were highly suggestive of hepatic epithelioid hemangioendothelioma (EHE).
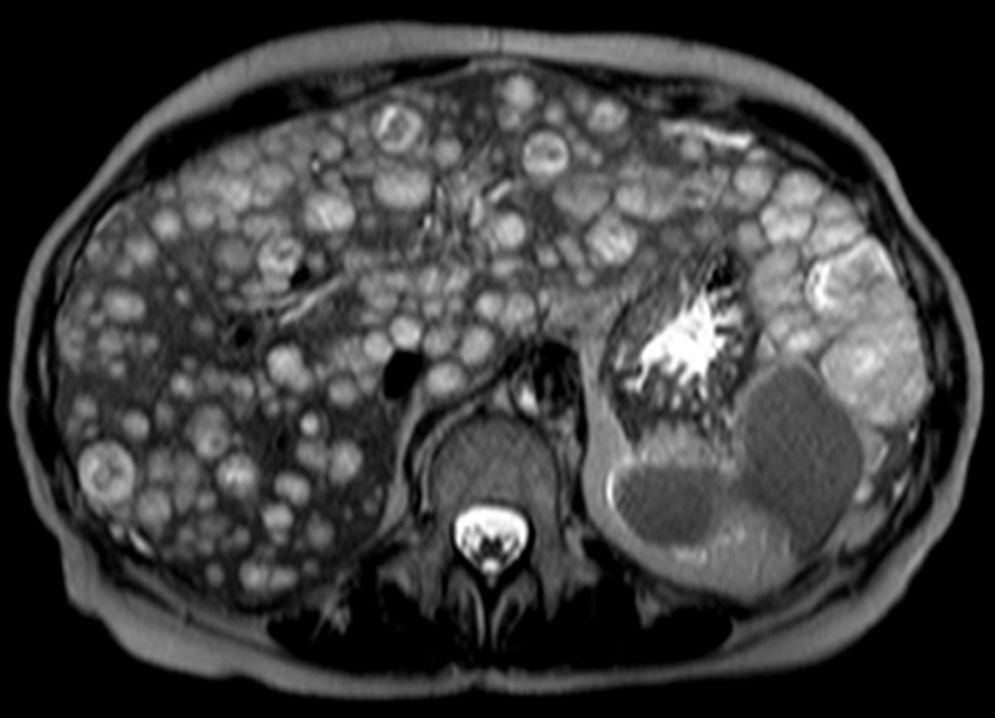
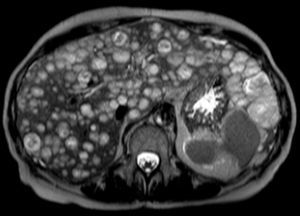
A final contrast-enhanced abdominal MRI (Fig. 4) was taken just before treatment was initialized (4 weeks after the first MRI). The liver parenchyma was now almost completely substituted by hemangioendothelioma lesions that reveal progressive contrast enhancement in the portal and delayed imaging phases.
Due to massive hepatic involvement, liver transplantation would be the best therapeutic option.2 However, the synchronous laryngeal tumor precluded this alternative and the patient started a regime of IV bevacizumab, an angiogenesis inhibitor. After 2 months of clinical and tumoral stability (MRI proven), patient's clinical condition worsened and a new MRI revealed progression of liver disease and ascites. The patient finally died from respiratory infectious complication.
HEH is a very uncommon primary tumor of liver vasculature, usually defined as intermediate-grade malignancy and considered one of the less aggressive hepatic malignancies. Nevertheless, there are aggressive cases with progressive tumor growth leading to hepatic failure, extra-hepatic metastases and death.3
Three forms of the tumor are recognized: single nodular, multifocal and diffuse type. The majority of tumors correspond to the multifocal-type. Characteristic MR features of multifocal HEH include multiple hepatic nodules usually centered in the periphery of the liver, coalescent, hypointense in T1-weighted imaging, heterogeneously hyperintense in T2-weighted imaging with progressive, delayed contrast-enhancement.3
When feasible, the most effective treatment is liver transplantation with 1-year and 5-year patient survival rates of 96% and 54.5%.4 Evidence suggests that even patients with limited extra-hepatic disease can be considered for transplantation. Other therapeutic strategies, as the use of angiogenesis inhibitors, can be considered when transplantation is not an option.5
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study
Confidentiality of dataThe authors declare that no patient data appear in this article
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors are most grateful to Professor Pieter Demetter (Department of Pathology, Hôpital Erasme, Brussels, Belgium) for his important contribution to the accomplishment of this work. The pathological findings were crucial for the final diagnosis, particularly due to the lack of specificity of the imaging findings. The diagnostic and therapeutic decisions were taken together, in group, by different members of the Departments of Gastroenterology and Hepato-Pancreatology, Medical Oncology and Digestive Surgery of the Hôpital Erasme, to whom we also would like to thank.