Among the symptoms presented by patients with SARS-Cov-2 infection, we can find various otorhinolaryngological alterations. Dysphonia appears in up to 79% of infected patients during the acute phase. Dysphonia can also occur as a sequelae, often underestimated, possibly due to its appearance along with other symptoms, also in patients after prolonged intubation or tracheostomy. We present a systematic review of the literature with a bibliographic search in PubMed, Cochrane and Google Scholar, with MESH terms including studies in English and Spanish. The results of the studies found and the vocal manifestations in patients during COVID-19 disease and the consequences produced are analysed. Dysphonia is an acute manifestation of COVID-19 with alterations in aerodynamic and acoustic analysis and in fibrolaryngoscopy. Post-COVID dysphonia can be a persistent symptom that is often underestimated, requiring multidisciplinary management and speech therapy intervention. Laryngeal sequelae are common in post-intubation or post-tracheostomy patients and are related to intubation time, tube number, pronation and respiratory sequelae.
Entre los síntomas que presentan los pacientes con infección por SARS-Cov-2 podemos encontrar diversas alteraciones otorrinolaringológicas. La disfonía aparece en hasta un 79% de los pacientes infectados durante la fase aguda. La disfonía también puede presentarse como secuela, en muchas ocasiones infraestimada, posiblemente debido a su aparición junto con otros síntomas, también en pacientes tras intubación prolongada o traqueostomía. Presentamos una revisión sistemática de la literatura con búsqueda bibliográfica en PubMed, Cochrane y Google Scholar, con términos MESH incluyendo estudios en inglés y en español. Se analizan los resultados de los estudios encontrados y de las manifestaciones vocales en pacientes durante la enfermedad por COVID-19 y las secuelas producidas. La disfonía es una manifestación aguda del COVID-19 con alteraciones en análisis aerodinámico y acústico y en la fibrolaringoscopia. La disfonía post-COVID puede ser un síntoma persistente que es a menudo infraestimado, requiriendo manejo multidisciplinar e intervención logopédica. Las secuelas laríngeas son frecuentes en pacientes post-intubación o post-traqueostomía y se relacionan con el tiempo de intubación, el número de tubo, la pronación y las secuelas respiratorias.
The COVID-19 pandemic has posed a challenge in terms of diagnosis and management of affected patients, due to both their complexity and clinical variation and severity, as well as to the challenges associated with isolation and infection control. Amongst the most frequent manifestations of COVID-19 disease are fever, cough, dyspnoea and general malaise,1 however the disease can present in varying degrees of severity and the range of symptoms during the acute phase also includes digestive, neurological and otolaryngological symptoms. The great variability of patient types, comorbidities, age, and differences in management and treatment make both acute manifestations and sequelae derived from the disease or management during hospitalisation difficult to analyse.2
According to some studies,3 the typical presentation of the disease at the beginning of the pandemic is fever, constitutional symptoms and cough.4 Some studies published on European patients show some difference in terms of clinical presentation, and in these studies the prevalence of otolaryngological symptoms is higher than in the articles published during 2020.5 Among the otolaryngological symptoms of COVID-19 disease are cough, anosmia, odynophagia, ageusia and nasal congestion,6 these being the most prevalent ones. Among hospitalised patients, the most common otolaryngological symptoms are cough, hyposmia/anosmia, dysgeusia/ageusia, and odynophagia.1
Vocal manifestations of COVID-19 can go unnoticed for a number of reasons. According to some studies, this is explained by the fact that the subjective perception of patients with multiple sequelae after COVID-19 disease is underestimated, possibly because concern about other symptoms such as persistent dyspnoea or fatigue makes dysphonia less subjectively evident.7 In addition, the prevalence of dysphonia varies in different studies; in non-hospitalised and hospitalised patients8; and in patients who have required prolonged intubation or tracheostomy,9 depending on the time since diagnosis, etc.10 The study of all manifestations related to voice is essential when it comes to correctly diagnosing these patients and establishing which factors will affect clinical evolution and prognosis, in order to adjust the treatment to each case.
The objectives of this article are to establish which are the most frequent vocal manifestations among these patients, in both the acute phase of COVID-19 and in the sequelae phase or post-COVID-19 syndrome; secondly, to detail the subjective perception regarding voice changes in these patients; and thirdly, to study the causes derived from the disease itself, or from the treatments required to alleviate it, that have caused these vocal manifestations, as well as analysing the therapeutic options described in these patients.
Material and methodsA systematic review of the literature has been undertaken, including articles published in indexed journals between 2020 and 2022, in both English and Spanish.
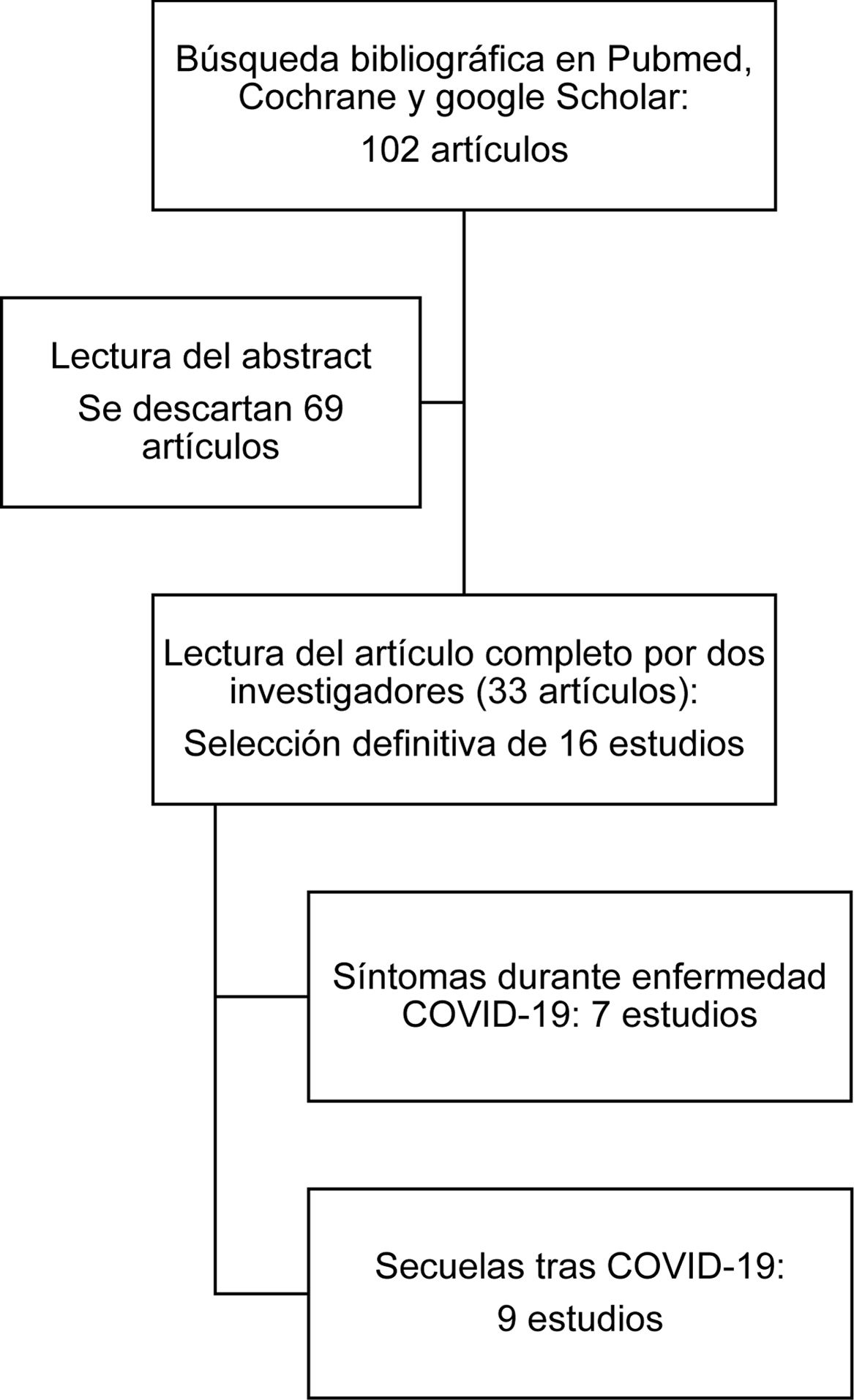
An extensive literature search was conducted in the PubMed, Google Scholar and Cochrane databases and 102 articles were selected. This study complies fully with the points detailed in the PRISMA 2020 declaration.11 Exclusion criteria included patients under 18 years of age, single-case studies, studies with fewer than 10 patients, or literature reviews and studies with data on dysphonia collected on the basis of a “yes” or “no” question only.
The terms that were included in the search criteria were the following: “dysphonia”, “voice disorders”, “infection”, “COVID-19”, “Sars-cov-2”, and 102 (56+46) articles published between 2020 and 2022 were obtained. The date of the literature search was 1st April 2023.
After a first reading of the abstracts of the selected articles, a total of 33 articles were selected. A reading of the full text of the articles obtained by two different researchers was then conducted independently, and finally a total of 16 articles were selected that met the criteria laid down in the second paragraph of this section.
Once the 16 studies had been identified, they were divided into 2 groups to facilitate data collection and synthesis. On the one hand, studies on the acute phase of the disease were grouped together, and on the other, studies analysing the sequelae after COVID-19 disease and long COVID (Fig. 1).
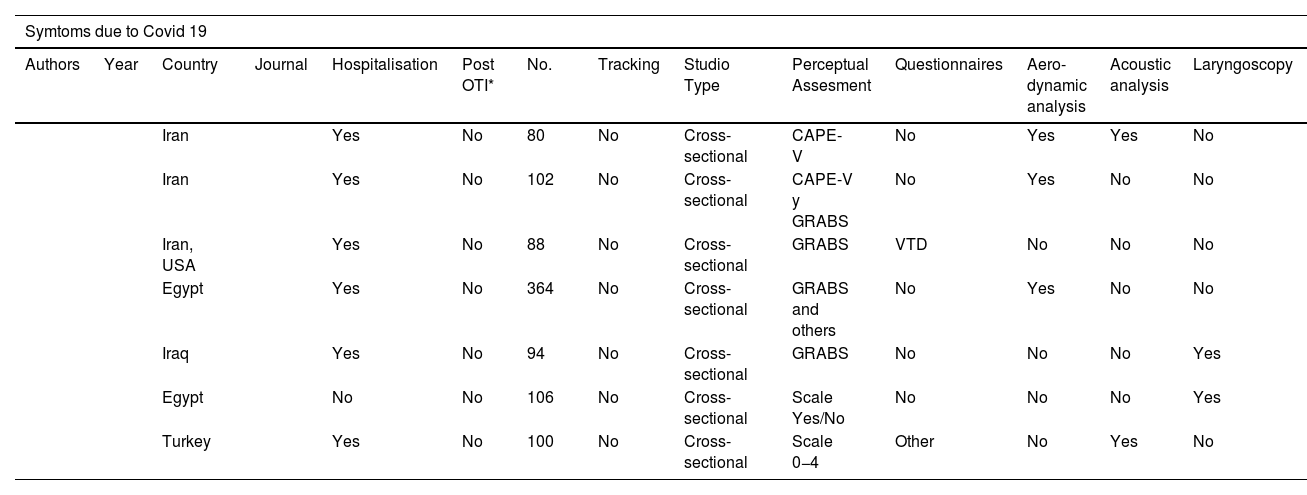
ResultsHigh-pitched vocal manifestationsSeven articles analysed acute dysphonia associated with COVID-19 (Table 1). Regarding the prevalence of dysphonia, results ranged from 68%,12 79%,13 or 22.3% in hospitalised patients.14 In two of the articles, dysphonia was more frequent in women than in men.12,14 Regarding the perceptual analysis of the voice, in the studies quantified using the CAPE-V, GRABS or other scales, the differences were significant when comparing COVID-19 patients with healthy ones.15–18 Both the aerodynamic analysis or maximum phonation time (MPT) and the acoustic analysis showed statistically significant differences in the various different studies.15,16,18
Studies included in the systematic review, dysphonia subgroup in the acute phase of COVID-19 disease.
| Symtoms due to Covid 19 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Authors | Year | Country | Journal | Hospitalisation | Post OTI* | No. | Tracking | Studio Type | Perceptual Assesment | Questionnaires | Aero-dynamic analysis | Acoustic analysis | Laryngoscopy |
| Iran | Yes | No | 80 | No | Cross-sectional | CAPE-V | No | Yes | Yes | No | |||
| Iran | Yes | No | 102 | No | Cross-sectional | CAPE-V y GRABS | No | Yes | No | No | |||
| Iran, USA | Yes | No | 88 | No | Cross-sectional | GRABS | VTD | No | No | No | |||
| Egypt | Yes | No | 364 | No | Cross-sectional | GRABS and others | No | Yes | No | No | |||
| Iraq | Yes | No | 94 | No | Cross-sectional | GRABS | No | No | No | Yes | |||
| Egypt | No | No | 106 | No | Cross-sectional | Scale Yes/No | No | No | No | Yes | |||
| Turkey | Yes | No | 100 | No | Cross-sectional | Scale 0−4 | Other | No | Yes | No | |||
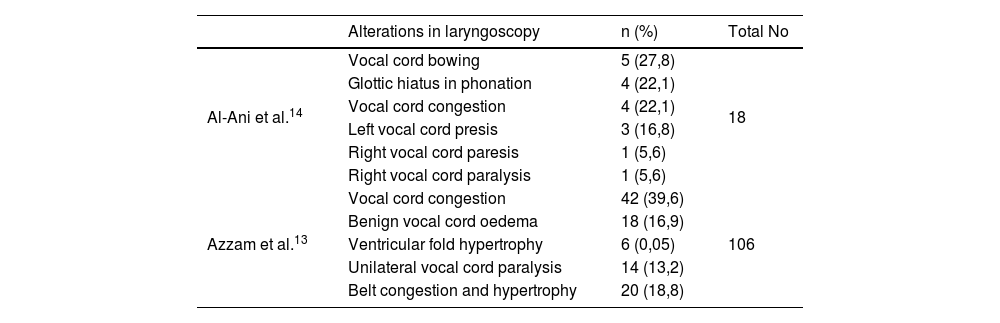
The most frequent findings on laryngoscopy were bowing of the vocal cord, glottic hiatus in phonation, congestion of both vocal cords, paresis or unilateral paralysis,14 benign vocal cord oedema, and ventricular fold hypertrophy13 (Table 2).
Results from laryngoscopy findings during the acute phase of COVID-19 symptoms.
| Alterations in laryngoscopy | n (%) | Total No | |
|---|---|---|---|
| Al-Ani et al.14 | Vocal cord bowing | 5 (27,8) | 18 |
| Glottic hiatus in phonation | 4 (22,1) | ||
| Vocal cord congestion | 4 (22,1) | ||
| Left vocal cord presis | 3 (16,8) | ||
| Right vocal cord paresis | 1 (5,6) | ||
| Right vocal cord paralysis | 1 (5,6) | ||
| Azzam et al.13 | Vocal cord congestion | 42 (39,6) | 106 |
| Benign vocal cord oedema | 18 (16,9) | ||
| Ventricular fold hypertrophy | 6 (0,05) | ||
| Unilateral vocal cord paralysis | 14 (13,2) | ||
| Belt congestion and hypertrophy | 20 (18,8) |
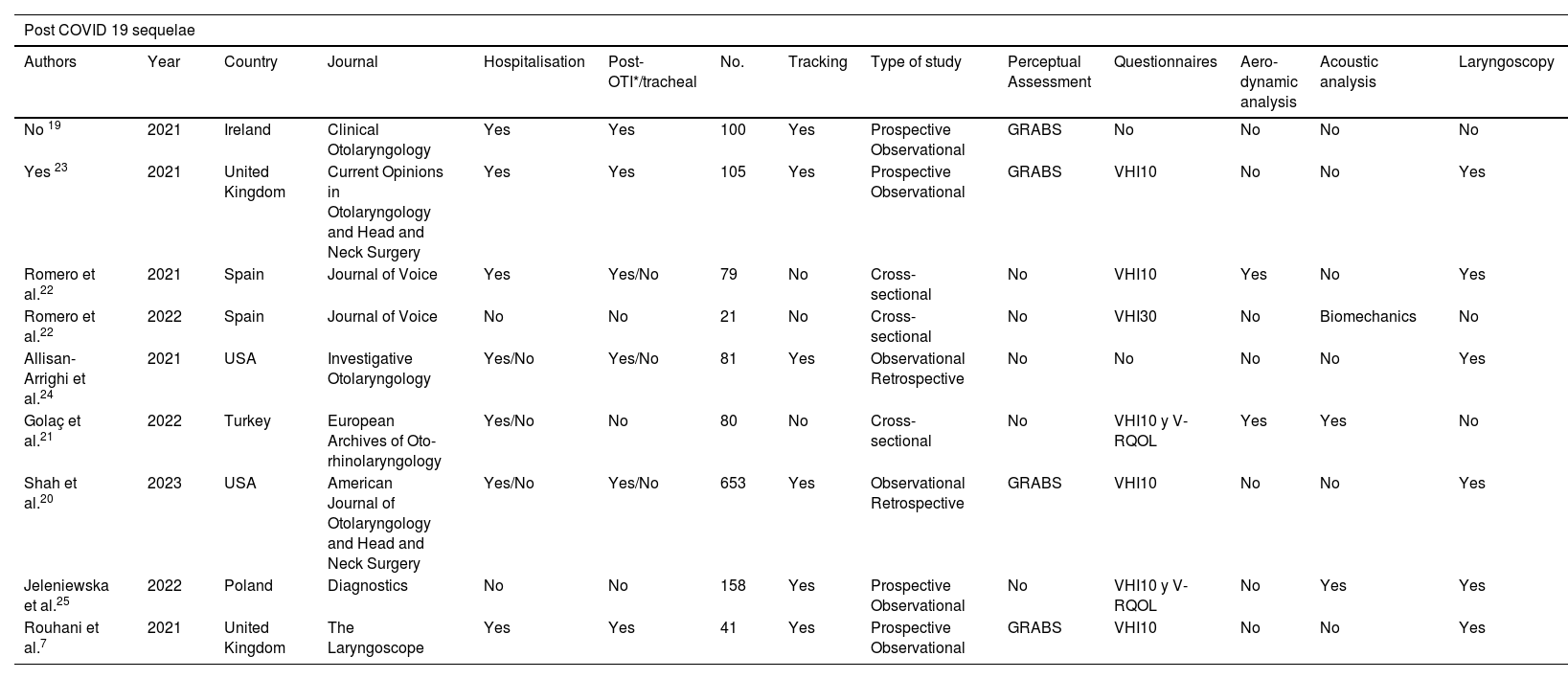
Nine studies refer to voice-related sequelae in patients who had tested positive for Sars-Cov-2 infection (Table 3).
Studies included in the systematic review, subgroup of dysphonia as a sequela of COVID-19 disease or as a post-COVID-19 syndrome.
| Post COVID 19 sequelae | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Authors | Year | Country | Journal | Hospitalisation | Post-OTI*/tracheal | No. | Tracking | Type of study | Perceptual Assessment | Questionnaires | Aero-dynamic analysis | Acoustic analysis | Laryngoscopy |
| No 19 | 2021 | Ireland | Clinical Otolaryngology | Yes | Yes | 100 | Yes | Prospective Observational | GRABS | No | No | No | No |
| Yes 23 | 2021 | United Kingdom | Current Opinions in Otolaryngology and Head and Neck Surgery | Yes | Yes | 105 | Yes | Prospective Observational | GRABS | VHI10 | No | No | Yes |
| Romero et al.22 | 2021 | Spain | Journal of Voice | Yes | Yes/No | 79 | No | Cross-sectional | No | VHI10 | Yes | No | Yes |
| Romero et al.22 | 2022 | Spain | Journal of Voice | No | No | 21 | No | Cross-sectional | No | VHI30 | No | Biomechanics | No |
| Allisan- Arrighi et al.24 | 2021 | USA | Investigative Otolaryngology | Yes/No | Yes/No | 81 | Yes | Observational Retrospective | No | No | No | No | Yes |
| Golaç et al.21 | 2022 | Turkey | European Archives of Oto-rhinolaryngology | Yes/No | No | 80 | No | Cross-sectional | No | VHI10 y V-RQOL | Yes | Yes | No |
| Shah et al.20 | 2023 | USA | American Journal of Otolaryngology and Head and Neck Surgery | Yes/No | Yes/No | 653 | Yes | Observational Retrospective | GRABS | VHI10 | No | No | Yes |
| Jeleniewska et al.25 | 2022 | Poland | Diagnostics | No | No | 158 | Yes | Prospective Observational | No | VHI10 y V-RQOL | No | Yes | Yes |
| Rouhani et al.7 | 2021 | United Kingdom | The Laryngoscope | Yes | Yes | 41 | Yes | Prospective Observational | GRABS | VHI10 | No | No | Yes |
Three of the articles included analyse the evolution of the voice in patients after prolonged intubation or tracheostomy. The subjective perception of dysphonia according to VHI-10 was less severe than the findings of the laryngoscopic examination and the perceptual assessment taking the GRABS scale.7 Predictors of dysphonia severity were injuries during intubation and a personal history of respiratory pathology.19 Patients with a stay in the ICU had persistent dysphonia 3 months after hospital discharge were at a higher percentage than those hospitalised on the ward (25% vs. 10.3%) and this was correlated with persistent dysphagia.8
Also, in this group of patients, MPT appeared to have a relationship with the vocal sequelae of COVID-19,8,21 while acoustic analysis sometimes showed no significant differences. In the study published by Romero et al.,22 a biomechanical analysis was run, showing that the patterns of analysis were similar to those found in other patients with laryngitis of other aetiologies.
The most frequent endoscopic findings in intubated patients were granulomas, subglottic abscesses, and scars in the glottic posterior commissure or glottic synechiae.23 The study published by Allisan-Arrighi et al.24 showed that a history of intubation was significantly correlated with the endoscopic finding of granuloma, while non-intubation correlated with muscle tension dysphonia.
Several studies analyse the evolution of the voice after surgery or speech therapy and describe a significant improvement after the intervention in patients who underwent surgery,23 while in patients who underwent speech therapy, the result was clinical improvement or resolution of symptoms.20
The study by Shah et al. describes a diagnostic entity termed “COVID-19 related laryngeal hypersensitivity”, which was present in 36.4% of patients with no previous history of intubation. Laryngotracheal stenosis was statistically more frequent in post-intubation patients, all of whom underwent surgery and all of them improved clinically.20
It is worth highlighting the data published by Jeleniewska et al., which analyses patients without a history of intubation or tracheostomy, who presented dysphonia as the only symptom of post-COVID-19 syndrome. The most frequent findings were erythema and mucosal dryness of the vocal cords, with the presence of mucous over the glottis, showing improvement in both acoustic analysis and at laryngoscopic examination after medical and speech therapy treatment.25
DiscussionAcute dysphonia due to COVID-19 could be due to laryngeal inflammation and oedema produced by the inflammatory process in the airways. Regarding the aetiology of this inflammation, several studies have shown that there is a high expression of angiotensin-converting enzyme 2 (ACE2),26,27 the receptor for COVID-19, in the vocal cords. ACE2 is a target of the Sars-Cov-2 virus and is also present in the epithelium of the lung, small intestine, vascular endothelium and oral cavity.27 This inflammation would partly account for the fibrolaryngoscopic findings, such as congestion of both vocal cords, benign vocal cord oedema and ventricular fold hypertrophy, vocal cord bowing, glottic hiatus in phonation, and unilateral vocal cord paresis or paralysis.13,14
Regarding the aerodynamic analysis, MPT decreased in several studies,15,16,18 which these authors justify by a decrease in respiratory support, as well as inflammation at the glottic level and phonorespiratory discoordination.15,17
According to some studies, the number of complications after intubation in COVID-19 patients is higher than in other pathologies, due to a combination of circumstances such as the prone position, the prothrombotic state in these patients, and the treatment with corticosteroids that produces mucous membrane atrophy, etc.28,29 It should also be noted that the first guidelines for the management of COVID-19 patients considered avoiding early tracheostomy in intubated patients. For this reason, these patients had been intubated for more days when they underwent tracheostomy,29 a circumstance which has been shown in different studies to be associated with more complications.30
Regarding the type of laryngeal sequelae, the most frequent were granuloma, subglottic stenosis, vocal cord paralysis, and posterior glottic synechia,9,30,31 and are common findings in patients intubated for other causes.30,32 These lesions depend on the time of intubation, the number of tubes used, and the patient's pronation, and these findings are compatible with laryngeal sequelae in patients intubated for other causes.32
Dysphonia as a post-intubation and post-tracheostomy sequela is related to the onset of dysphagia.33 These patients require joint treatment of both pathologies, with speech therapy rehabilitation and multidisciplinary management.34,35
Finally, regarding the persistence of dysphonia in patients with post-COVID-19 syndrome,7 the subjective perception of dysphonia was less severe than the findings of laryngoscopic examination and perceptual assessment. According to the authors, this may be due to the fact that, in the context of multiple post-tracheostomy and post-COVID-19 sequelae, patients attach little importance to vocal evolution.
The articles included in this systematic review have constraints associated with the isolation of these patients, and only two of them include endoscopic examination in the acute phase13,14 due to the risk of disease transmission. Some authors also point out possible confounding factors for dysphonia in these patients, including gastroesophageal reflux. Other confounding factors could be the use of oxygen therapy and corticosteroids, which dry out the vocal tract,37 as well as the stress present in these patients.36
ConclusionsDysphonia is an acute manifestation of COVID-19 with a variable prevalence in different studies: changes were observed in aerodynamic and acoustic analysis and in fibrolaryngoscopy. Post-COVID dysphonia can be a persistent symptom that is often underestimated and can last up to 5–6 months after the acute phase, requiring multidisciplinary management and speech therapy intervention. Laryngeal sequelae are common in post-intubation or post-tracheostomy patients and are related to intubation time, tube number, pronation, and respiratory sequelae.
Conflict of interest and fundingThe authors have no conflict of interest and have not received any funding.