Training in surgical specialties has declined during the COVID-19 pandemic. A study was carried out to further analyze the impact of the COVID-19 pandemic on specific aspects of clinical, training, and research activities performed by the otolaryngology residents in Spain.
MethodsA cross-sectional qualitative study was conducted during the last two weeks of February 2021. The study consisted of an online survey taken by otolaryngology residents who had undertaken one-year continuing training from February 15, 2020, to February 15, 2021, and consisted of 26 questions exploring the impact of the COVID-19 on the health of the ENT residents and training activities. Categorical variables were reported as frequency and percentage. When indicated, Pearson’s Chi-square test (χ2) with Yates’s correction and Pearson's correlation coefficient (r) were used.
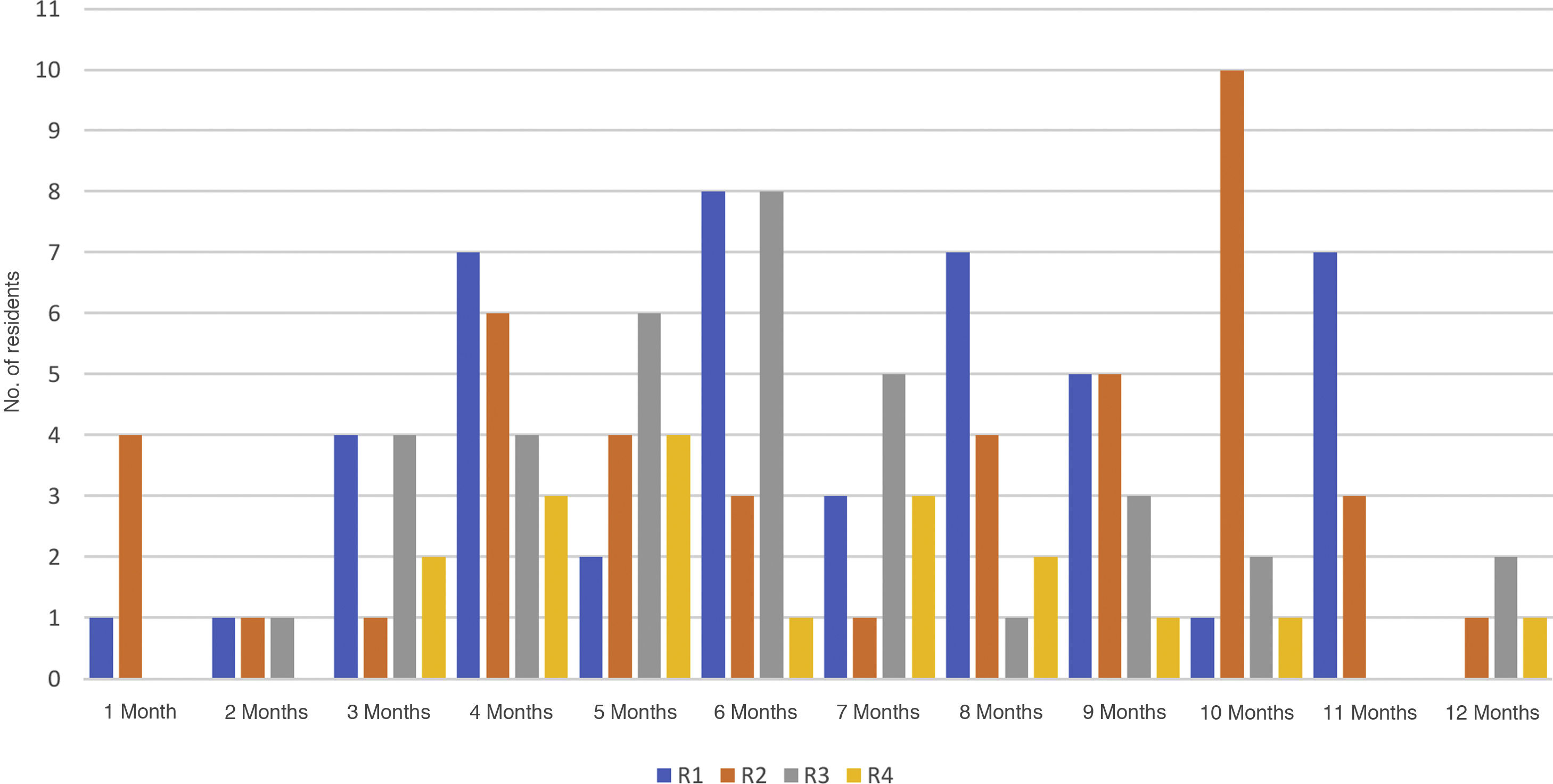
Results143 completed surveys were received from 264 Residents (54.17%). 36 residents (25.2%) have suffered from the disease due to SARS-CoV-2. Most of them only developed mild symptoms (86.1%), with 3 requiring hospitalisation (8.3%). The origin of infection was unknown in all reported cases and the need for confinement was principally due to either attending an asymptomatic patient in 9 cases (6.3%) or to being supposedly in close contact with an asymptomatic person in 22 (15.4%). 60.1% of the residents surveyed reported having lost more than 6 months of their training period, and in 18.8% of cases, it was as high as 10 and 12 months. There has been a reduction of more than 75% of what was planned in surgical training (p<0.05) of tympanoplasty, mastoidectomy, stapedectomy, cochlear implants, endoscopic sinonasal and anterior skull base surgery, septoplasty and turbinoplasty.
ConclusionsThe decline in ENT activity and residents having to assist in other COVID-19 units during the most critical moments of the pandemic, has caused the main reduction in their training capacity. Contagion mainly occurred through contact with asymptomatic carriers during patient care and through supposedly close contact with asymptomatic carriers. Virtual activities have been widely accepted, but they have not completely replaced all residents’ training needs. Measures should be implemented to recover lost training, especially surgical practical learning in otology and rhinology.
La pandemia COVID-19ha alterado todas las actividades sanitarias, entre ellas la formación especializada de los residentes. Se llevó a cabo un estudio para analizar en profundidad el impacto de la pandemia COVID-19 en aspectos específicos de las actividades clínicas, formativas e investigadoras que realizan los residentes de Otorrinolaringología (ORL) en España durante un año completo de formación.
Material y métodosSe realizó un estudio cualitativo transversal durante las últimas dos semanas de febrero de 2021. El estudio consistió en una encuesta en línea realizada por residentes de ORL que habían realizado un año continuado de formación desde el 15 de febrero de 2020al 15 de febrero de 2021 y consistió en 26 preguntas que exploraban el impacto del COVID-19 en la salud de los residentes de ORL, en su dedicación laboral y en las actividades de formación. Las variables categóricas se informaron como frecuencia y porcentaje. Cuando se indicó, se utilizó la prueba Chi-cuadrado de Pearson con la corrección de Yates y el coeficiente de correlación de Pearson (r).
ResultadosSe recibieron 143 encuestas cumplimentadas de 264 residentes (54,17%). 36 residentes (25,2%) habían padecido la enfermedad por SARS-CoV-2. La mayoría de ellos solo desarrolló síntomas leves (86,1%) y 3 requirieron hospitalización (8,3%). Los residentes encuestados que resultaron positivos para el SARS-CoV-2 no fueron capaces de identificar la fuente de su contagio y la necesidad de confinamiento se debió principalmente a la atención de un paciente asintomático en 9 casos (6,3%) o al contacto estrecho con un asintomático en situaciones no identificadas distintas de la atención sanitaria en 22 (15,4%). El 60,1% de los residentes encuestados reportó haber perdido más de 6 meses de su período de formación, y en el 18,8% de los casos llegó a 10 y 12 meses. Se ha producido una reducción de más del 75% de lo previsto en formación quirúrgica (p<0,05) de timpanoplastia, mastoidectomía, estapedectomía, implantes cocleares, cirugía endoscópica nasosinusal y de base de cráneo anterior, septoplastia y turbinoplastia.
ConclusionesEl descenso de la actividad ORL y la necesidad de prestar asistencia en otros servicios y unidades durante los momentos más críticos de la pandemia han causado la principal reducción de su capacidad de formación. El contagio fundamentalmente ocurrió por el contacto con portadores asintomáticos durante la atención a pacientes y por contacto estrecho con portadores asintomáticos. Las actividades virtuales han sido ampliamente aceptadas, pero no han reemplazado por completo las necesidades de formación de todos los residentes. Se deberán implementar medidas para recuperar la formación perdida, especialmente el aprendizaje práctico quirúrgico en otología y rinología.
Specialised training has been significantly impacted by the COVID-19 pandemic, caused by the SARS-CoV-21,2 virus. A high volume of day-to-day healthcare was cancelled and many professionals had to provide support to hospital services overwhelmed by the speed and intensity of the pandemic. Many ear, nose and throat (ENT) services resorted to alternatively segregating part of their residents by assigning them to face-to-face activities, while others were protected from possible infection by isolating them at home.3 The need to reduce uncertainties about the mechanisms of infection and to make up for the shortfall in protective materials and equipment became a top priority at the onset of the pandemic. Care processes and hospital structures were redesigned to care for COVID-19 patients, relegating care to non-COVID-194 patients. Many centres were forced to cancel non-emergency surgery due to a lack of hospital beds and even the temporary use of operating theatres and post-anaesthesia recovery rooms as intensive care unit (ICU) beds. The volume of patients attending ENT services for any pathology was reduced, due to population restrictions on non-essential travel and limitations on citizens’ access to primary care centres.5
ENT services acted quickly to implement training models adapted to the restrictions arising from the pandemic, to mitigate training deficiencies due to the cancellation of on-site training activities6–8 and the need to follow the recommendations on protection issued by healthcare and scientific institutions and organisations.9–11 Multiple web-based virtual communication solutions were implemented and simulation alternatives were promoted to compensate for the reduction in surgical procedures.12,13
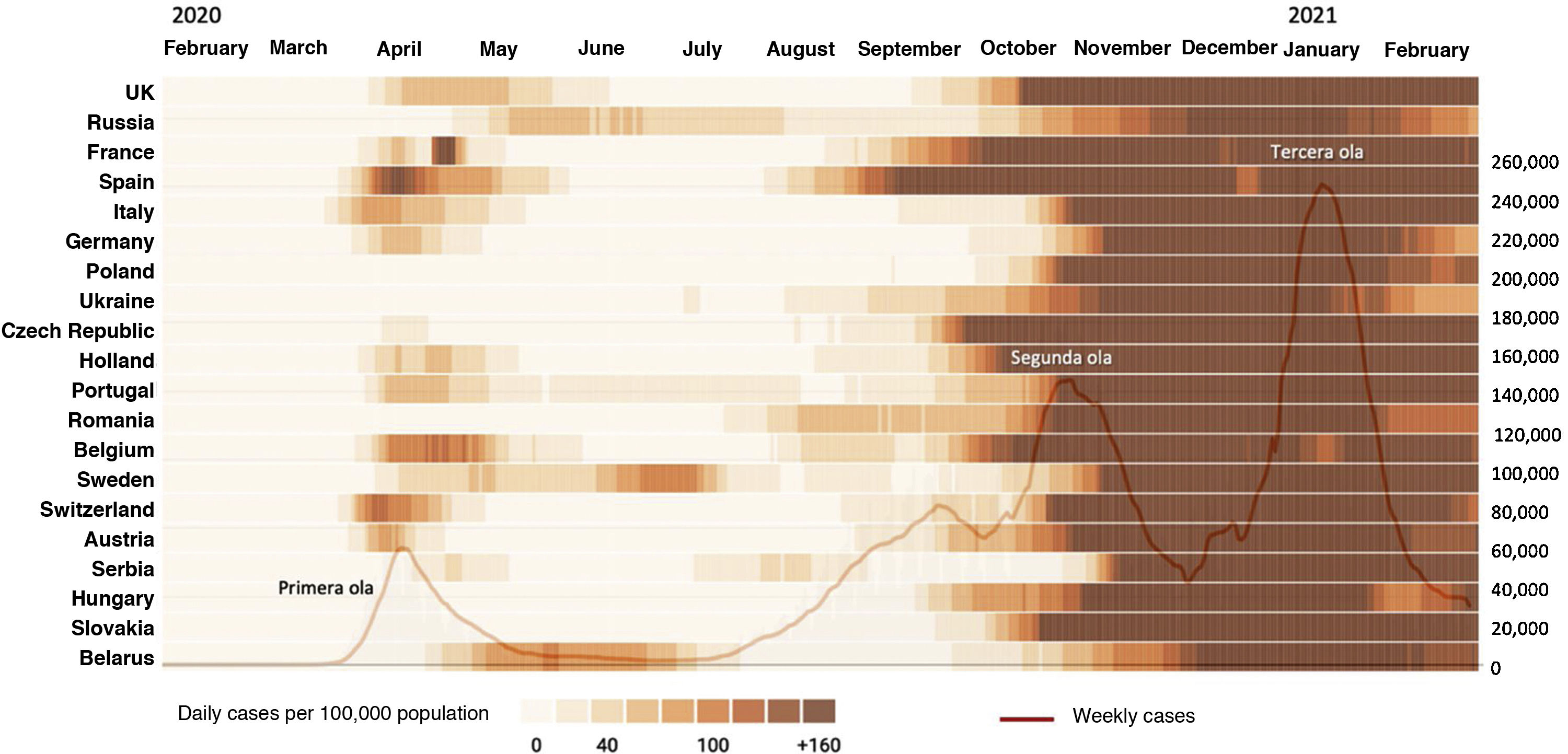
By late spring 2020, the perception of disease control was widespread and the results of the impact of the pandemic on the training of ENT residents began to be available.14–16 However, the lack of knowledge of the behaviour of this new disease and the strong social, political and economic interference aimed to de-escalate the restrictive measures imposed to prevent the infection of the population more quickly than desirable, revealed that the outbreak of Spring 2020 had only been a first wave. A second wave appeared, more intense but slower to set in and decline than the first, and then a third, much more intense than the previous two, without ever reaching a state of normality. The incidence of each of these three waves lasted longer in Spain than in other European countries, although with wide geographical variability and time sequence within Spain itself (Fig. 1).17
The first publications on the impact of the COVID-19 pandemic on ENT training solely reported the effect of the first wave in the spring of 2020. One year after the onset of the pandemic, it is possible to assess the impact it has had on the training of Spanish ENT residents over a period of time equivalent to one year of their training time. This knowledge acquires great relevance in Spain, where the training time for a surgical speciality such as ENT is 4years.
The aim of this study was to gain detailed knowledge of the impact of the COVID-19 pandemic on specific aspects of the different areas of the care, training and research work undertaken by ENT residents in Spain, as well as the solutions adopted to adapt to the shortcomings and their acceptance of virtual training modes.
Material and methodsStudy designSA qualitative cross-sectional study was run by online survey during the second half of February 2021 on ENT residents in Spanish teaching units who had completed their training over a continuous year between 15th February 2020 and 15th February 2021.
The COVID-19 pandemic occurred in Spain in the format of increasingly frequent periods of incidence, known as "waves", defined as the periods between the increase and decrease in SARS-CoV-2 positive cases, as diagnosed by polymerase chain reaction (PCR), where cases were over 10% of prevalent cases in the preceding 14days. Thus, the first wave is considered to be between 10th March and 10th May 2020, the second wave between 1st September and 16th November 2020, and the third wave between 11th December 2020 and 15th February 2021.
PopulationThe study population consisted of ENT residents (R) who had obtained their place for the 2017, 2018, 2019 and 2020 courses (R4, R3, R2 and R1, respectively) at one of the 77 accredited ENT teaching units in Spain, all of these within the public health system, except one in the private health sector. All hospitals attended to both COVID-19 positive patients and non-COVID-19 patients. Residents from the 2016 course were excluded as they were impacted by the pandemic only during the period between 10th March and 20th May 2020, which was the period of completion of their residency course.
Survey designThe survey was conducted using Google Forms and consisted of 26 questions spread across 8 sections: 1) geographical location of the hospital by region and locality; 2) impact of the SARS-CoV-2 disease on the health of ENT residents and diagnostic tests they had undergone; 3) impact on the healthcare work at the centre; 4) impact on the overall changes in theoretical training activities, and specifically by areas of the speciality, including the new virtual training models; 5) impact on the overall changes in practical training activities, specifically by areas of the speciality; 6) impact on internal and external rotations, courses, conferences, stays, etc.; 7) Impact on research activities; and 8) Overall impact on the acquisition of skills and know-how as an ENT specialist.
Distribution of the questionnaire and data collectionAn email was sent in two waves to all ENT residents in Spain informing them of the aim and scope of the study, requesting their participation. They were informed of all aspects of the research and their consent was obtained for the study; this being approved by the Andalusian Biomedical Research Ethics Committee.
Validation of the questionnaireThe variables on the impact of the COVID-19 pandemic on the activities of the residency courses formed the basis of the research questionnaire. These were measured using a 5 point Likert scale which was subjected to a validity test using Pearson’s correlation method (ρ), establishing that all items were valid at a 95% confidence level.
The reliability of the survey was determined by obtaining a score of α=0.790 with Cronbach's alpha test for 5 items. The items used to measure the impact of the COVID-19 pandemic on residency courses were thus consistent and would produce the same results if used more than once.
Statistical analysisA statistical analysis was run with the Statistical Package for Social Sciences, version 26 (SPSS, Chicago, IL, USA). Categorical variables were summarised as frequency and percentage. Comparison between levels of impairment in residents' training and the impact of the COVID-19 pandemic on their training was undertaken using Pearson's chi-square test with correction for Yates' continuity. A p-value cut-off point of 0.05 with a 95% confidence interval was used to determine statistical significance.
ResultsA total of 143 completed surveys were received from a total of 264 residents sent out, with a response rate of 54.17% (62.8% female) and a margin of error of 5.56% for a 95% confidence interval. Surveys came from 59 ENT departments out of 77 accredited for specialised ENT training (76.6%) from 15 out of the 17 autonomous communities (88.2%). Respondents were 18 out of 81 R4 (22.2%), 36 out of 69 R3 (52.2%), 43 out of 63 R2 (68.2%) and 46 out of 51 R1 (90.2%).
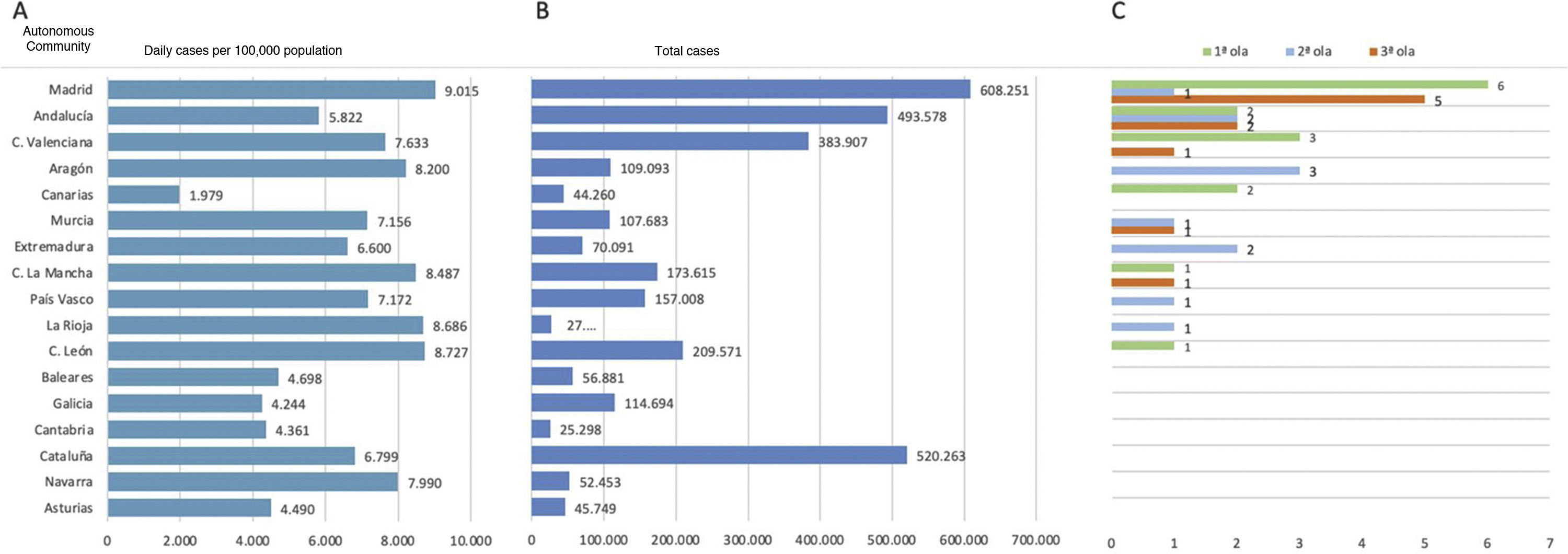
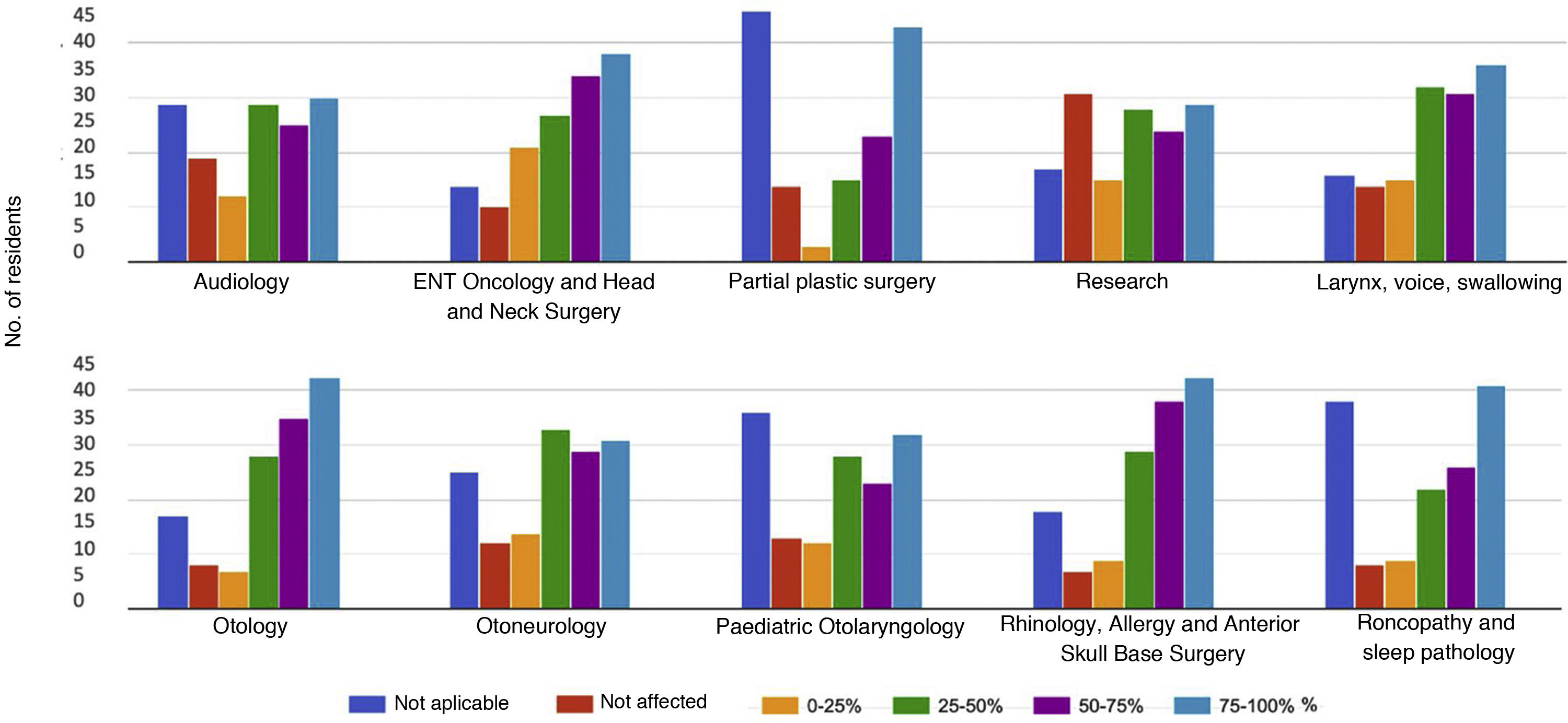
Thirty-six ENT residents (25.2%) became ill with SARS-CoV-2: 14 in the first wave (38.9%), 12 in the second wave (33.3%) and 10 in the third wave (27.7%). The Autonomous Communities of residents who fell ill were Madrid (n=12, 33.3%) Andalusia (6, 16.6%), Valencia (n=4, 11.1%), Aragon (n=3, 8.3%), Canary Islands (n=2, 5, 6%), Castilla-La Mancha (n=2, 5.6%), Extremadura (n=2, 5.6%), Murcia (n=2, 5.6%), Castilla y León (n=1, 2.8%), La Rioja (n=1, 2.8%) and the Basque Country (n=1, 2.8%); Fig. 2 shows the relationship between the number of residents with SARS-CoV-2 disease over the three waves, according to their geographical location and the incidence in the regions. Of these cases, 31 had only mild symptoms and did not require medical attention (86.1%), 3 were hospitalised with severe symptoms (8.3%) and 2 had moderate symptoms requiring medical attention without hospitalisation (5.6%). No resident was admitted to an ICU. The intensity of involvement meant that 14 were absent from work between 0 and 14days, 19 were absent between 15 and 30days and 3 were absent between 31 and 60days. The impact of COVID-19 on residents' health and absence from work is shown in Table 1. Fig. 3 shows the overall impact of each sub-area of the speciality, while the specific impact on the surgical work in the most relevant procedures for specialised training is shown in Table 2. Of the 15 procedures, 10 showed a statistically significant difference as regards the decrease in surgical training in the year of residency, except for the increase experienced globally between R1 and R2. Table 3 shows the impact on face-to-face training activities and research.
Impact of SARS-CoV-2 on residents' health, absence from work and time devoted to the speciality of ENT.
| Residents who had the disease | 36 (25.2%) |
| Mild | 31 (86.1%) |
| Moderate (with medical treatment) | 2 (5.6%) |
| Serious (with hospitalisation) | 3 (8.3%) |
| Absence of disease | 107 (74.8%) |
| Diagnostic tests receivediagnostic tests received | |
| Used on sick residents for the diagnosis of SARS-CoV-2 | |
| PCR test | 26 (72.2%) |
| Antibodies* | 10 (27.8%) |
| Used on sick residents to determine the cure for SARS-CoV-2 | 32 (94.1%) |
| Used on healthy residents suspected of infection by SARS-CoV-2 | |
| Minimum of 1 PCR test | 102 (97.1%) |
| More than 1 PCR test | 98 (85.8%) |
| Minimum of 1 antigen test or antibody test | 107 (100%) |
| Absence of a job | |
| Non absence | 49 (34.3%) |
| Caused by contracting the disease | |
| 0−14 days | 14 (9.8%) |
| 15−30 days | 19 (13.3%) |
| 30−60 days | 3 (2.1%) |
| Caused by confinement** | |
| 0−14 days | 35 (24.5%) |
| 15−30 days*** | 14 (9.8%) |
| 30−60 days*** | 3 (2.1%) |
| 60−90 days*** | 4 (2.8%) |
| Confinement additional to those who had been ill** | 10 (7%) |
| Time devoted by residents to their ENT unit during the pandemic | |
| Complete, continuous dedicación | 69 (48.3%) |
| Partial dedication to emergency services | 33 (23.1%) |
| Partial dedication to the internal medicine services | 18 (12.6%) |
| Partial dedication to other front-line services directed at COVID-19 | 19 (13.3%) |
| Partial dedication to the intensive care unit | 1 (0.7%) |
| Compliance with ENT activities planned before the pandemic | |
| Complete compliance | 41 (28.7%) |
| 80−99% compliance | 49 (34.3%) |
| 60−79% compliance | 29 (20.3%) |
| 40−59% compliance | 16 (11.2%) |
| 20−39% compliance | 6 (4.2%) |
| <20% compliance | 1 (0.7%) |
Not all residents were tested for antibodies, so it is possible that some of them were asymptomatic positive and acted as a source of infection.
Number of residents affected by the reduction or increase in the volume of surgical activity during the COVID-19 pandemic for the main procedures relative to the average number of procedures overall.
| Procedures | n | Mean*** | R1 (n=46) | R2 (n=43) | R3 (n=36) | R4 (n=18) | p (Yates correction) | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Reduction | Inc. | Reduction | Inc. | Reduction | Inc. | Reduction | Inc. | ||||||||||||||||||||
| N.A. | 0 | 1 | 2 | 3 | N.A. | 0 | 1 | 2 | 3 | N.A. | 0 | 1 | 2 | 3 | N.A. | 0 | 1 | 2 | 3 | ||||||||
| Adeno-tonsillectomy* | 40 | 218 | 3 | 4 | 4 | 15 | 18 | 2 | 6 | 10 | 3 | 7 | 17 | 0 | 13 | 8 | 3 | 3 | 9 | 0 | 4 | 6 | 4 | 2 | 2 | 0 | 0.003 |
| Ventilation tubes* | 20 | 128 | 5 | 3 | 3 | 10 | 22 | 3 | 6 | 7 | 5 | 6 | 19 | 0 | 13 | 8 | 3 | 4 | 8 | 0 | 4 | 8 | 2 | 2 | 2 | 0 | 0.003 |
| Turbinoplasty | N.A. | 86 | 8 | 2 | 5 | 13 | 16 | 2 | 6 | 5 | 4 | 10 | 18 | 0 | 7 | 9 | 6 | 4 | 10 | 0 | 5 | 2 | 6 | 3 | 2 | 0 | 0.045 |
| Septoplasty* | 15 | 116 | 12 | 1 | 2 | 14 | 15 | 2 | 2 | 4 | 5 | 9 | 21 | 2 | 2 | 5 | 6 | 11 | 12 | 0 | 1 | 3 | 7 | 2 | 5 | 0 | 0.030 |
| Endoscopic endonasal surgery* | 10 | 57 | 12 | 2 | 2 | 11 | 17 | 2 | 6 | 2 | 4 | 10 | 18 | 3 | 1 | 2 | 7 | 9 | 16 | 1 | 2 | 2 | 4 | 8 | 2 | 0 | 0.119 |
| Tympanoplasty (all types)* | 15 | 106 | 16 | 2 | 3 | 9 | 14 | 2 | 10 | 3 | 5 | 6 | 19 | 0 | 3 | 0 | 4 | 9 | 18 | 2 | 1 | 1 | 5 | 3 | 7 | 1 | 0.105 |
| Mastoidectomy | N.A. | 31 | 19 | 1 | 4 | 4 | 17 | 1 | 12 | 4 | 4 | 6 | 17 | 0 | 3 | 1 | 5 | 8 | 16 | 3 | 1 | 2 | 5 | 2 | 7 | 1 | 0,027 |
| Stapedectomy | N.A. | 27 | 20 | 0 | 3 | 4 | 16 | 3 | 13 | 2 | 4 | 6 | 18 | 0 | 3 | 0 | 4 | 8 | 17 | 4 | 2 | 0 | 4 | 3 | 8 | 1 | 0,060 |
| Audiological implants** | N.A. | 23 | 27 | 2 | 1 | 3 | 11 | 2 | 21 | 3 | 4 | 4 | 11 | 0 | 5 | 3 | 3 | 4 | 19 | 2 | 3 | 2 | 5 | 3 | 4 | 1 | 0.003 |
| Micro-laryngoscopy* | 30 | 162 | 7 | 4 | 8 | 13 | 12 | 2 | 0 | 11 | 9 | 9 | 13 | 1 | 3 | 7 | 9 | 4 | 13 | 0 | 2 | 4 | 8 | 3 | 1 | 0 | 0.067 |
| Transoral laser surgery* | 10 | 34 | 13 | 7 | 2 | 6 | 16 | 2 | 11 | 11 | 5 | 4 | 10 | 2 | 3 | 7 | 6 | 6 | 13 | 1 | 3 | 2 | 3 | 7 | 2 | 1 | 0.134 |
| Open head and neck surgery* | 6 | 43 | 10 | 4 | 10 | 8 | 12 | 2 | 3 | 11 | 7 | 11 | 8 | 3 | 0 | 10 | 8 | 6 | 10 | 2 | 1 | 4 | 0 | 12 | 1 | 0 | 0.001 |
| Partial laryngectomy | N.A. | 19 | 17 | 5 | 2 | 6 | 15 | 1 | 13 | 7 | 6 | 7 | 9 | 1 | 2 | 12 | 4 | 5 | 11 | 2 | 1 | 3 | 4 | 9 | 1 | 0 | 0.001 |
| Laryngectomy total* | 10 | 24 | 16 | 7 | 4 | 5 | 13 | 1 | 11 | 8 | 7 | 6 | 9 | 2 | 2 | 12 | 7 | 5 | 8 | 2 | 1 | 3 | 4 | 9 | 1 | 0 | 0.004 |
| Tracheotomy* | 20 | 55 | 1 | 11 | 0 | 7 | 11 | 16 | 3 | 11 | 3 | 4 | 10 | 12 | 3 | 11 | 6 | 7 | 2 | 7 | 1 | 2 | 4 | 4 | 0 | 7 | 0.044 |
Inc: increase; N.A.: not applicable (not scheduled in the year of residency); R1: first-year resident; R2: second-year resident; R3: third-year resident; R4: fourth-year resident.
0: <25%; 1: 25−50%; 2: 50−75%; 3: 75−100%.
Statistical significance: p<0.05.
Impact of COVID-19 on face-to-face training activities and research.
| Planned training activities | |
| Maintenance of all programmed activities | 16 (11,2%) |
| Reduction in programmed activities | 127 (88,8%) |
| Cancellation of internal rotations | 98 (68,5%) |
| Cancellation of courses and visits to other centres | 127 (88,8%) |
| Impact on clinical sessions | |
| Cancellation between 75−100% | 47 (32.8%) |
| Cancellation between 50−75% | 37 (25.9%) |
| Cancellation between 25−50% | 31 (21.7%) |
| Cancellation de Less than 25% | 28 (19.6%) |
| Impact on bibliographical sessions | |
| Cancellation between 75−100% | 56 (39,1%) |
| Cancellation between 50−75% | 33 (23,1%) |
| Cancellation between 25−50% | 24 (16,8%) |
| Cancellation less than 25% | 30 (20,9%) |
| Impact on theory course sessions | |
| Cancellation between 75−100% | 57 (39,8%) |
| Cancellation between 50−75% | 36 (25,2%) |
| Cancellation between 25−50% | 18 (12,6%) |
| Cancellation de Less than 25% | 32 (22,4%) |
| Implementation of virtual training activities prior to the pandemic | |
| Never | 100 (69,9%) |
| Between 50−75% | 11 (7,7%) |
| Between 25−50% | 8 (5,6%) |
| Less than 25% | 24 (16,8%) |
| Virtual clinical sessions held since the outbreak of the pandemic | |
| None | 27 (18,9%) |
| Between 75−100% | 25 (17,5%) |
| Between 50–75% | 22 (15,4%) |
| Between 25–50% | 22 (15,4%) |
| Less than 25% | 47 (32,8%) |
| Virtual bibliography sessions held since the outbreak of the pandemic | |
| None | 40 (27,9%) |
| Between 75–100% | 26 (18,2%) |
| Between 50–75% | 18 (12,6%) |
| Between 25–50% | 16 (11,2%) |
| Less than 25% | 43 (3.0.1%) |
| Virtual theory sessions held since the outbreak of the pandemic | |
| None | 50 (35%) |
| Between 75–100% | 23 (16,1%) |
| Between 50–75% | 15 (10,5%) |
| Between 25–50% | 17 (11,9%) |
| Less than 25% | 38 (26,5%) |
| Acceptance of the format to be followed in future residency training sessions | |
| 100% should be on-site | |
| 100% should be virtual | 7 (4,9%) |
| Some should be virtual | 112 (78,3%) |
| 100% should be face-to-face | 24 (16,8%) |
| Virtual surgery should be done | 16 (11,2%) |
| Research activities | |
| No research projects affected | 60 (41,9%) |
| Delay in research projects | 53 (37,1%) |
| Cancellation of research projects | 13 (9,1%) |
| Maintenance of the number of oral communications and posters for congresses | 71 (4,9%) |
| Reduction in the number of oral and poster communications for conferences | 53 (37,1%) |
| Cancellation of oral communications and posters for conferences | 7 (4,9%) |
| Residents who took advantage of the pandemic period to increase the number of occasions where they participated in conferences (all conferences have been virtual) | 10 (7%) |
Of all the residents, 100% considered that their training had been reduced as a consequence of the pandemic. Twenty-three (16%) felt that they had suffered a maximum impact, 73 (51%) a very high impact, 40 (27.9%) an average impact and 7 (4.9%) a low impact. Fig. 4 illustrates the residents' perception of this impact, expressed in terms of the amount of training time they felt they had lost. The 7 residents (4.9%) who had not seen their training substantially affected proposed not introducing any legal or regulatory modifications in the training course, while 54 (37.7%) raised the need to extend the residency for a further year; 22 (15.3%) were in favour of extending training for 6months and 19 (13.2%) for 3months, but 41 (28.6%) considered that the residency should be extended depending on the deficiencies and needs of each individual.
DiscussionThe response rate of 54.17% is sufficiently representative of the population and provides broad geographical coverage and of years of training for each group of residents surveyed. The reasons for the lower response to the survey among R4s are not known, but it is possible that the proximity of the end of their training period created uncertainty about the advantages and disadvantages of working over the following months as residents or as qualified specialists in areas such as accountability, labour relations, remuneration, job opportunities and jobs.
Spain was the fourth highest European country for incidence of confirmed SARS-CoV-2 cases until 8th March 2021, after Russia, the United Kingdom and France, with 3,149,012 people infected and an infection rate of 6.65%.17 Spain was also among the countries in the world with the highest number of health professionals in all categories infected until that date, with a total of 125,6912. By the start of the third wave, 16.5% of ENT specialists had been infected,18 which was 2.48 times the rate of the general population, however the 25.2% of ENT residents infected were 3.79 times the rate of the general population and 1.53 times that of ENT specialists, with the bias that the publication by Martin-Villares et al.18 did not include the incidence of the third wave. The autonomous communities of Madrid, Andalusia and Valencia had the highest incidence of infected ENT residents. These were the highest rates of population infection, but these regions also had the highest densities of residents, although Andalusia had a lower incidence rate than the other two. Surprisingly, no sick residents were recorded in Catalonia (15 respondents, 10.5% of the sample), a region that met the same incidence criteria as the previous regions. It is possible that this is a response bias, or that the high incidence in Catalonia instilled in the residents a greater sense of protection inside and outside the hospital. All respondents reported having undergone the appropriate diagnostic tests for SARS-CoV-2 at any given time and as often as they needed, so there was no deficiency in this regard.
Lack of protective materials and lack of knowledge of the disease may account for 38.9% of the residents infected in the first wave, however it cannot alone explain the 33.3% of those infected during the second wave and 27.7% of those infected during the third wave. Residents who became infected were not able to identify their source, but in no case did the residents surveyed link this to having cared for a SARS-CoV-2 positive patient, suggesting that knowledge of the illness led to sufficient alarm among residents to protect themselves adequately during their care.19 However, not all residents rigorously adopted self-protection measures in all cases where they cared for asymptomatic carriers. Of the total, 9 residents (6.3%) maintained preventive confinement as a result of being in close contact with patients whose positivity became known after their care by the resident. The main circumstance for preventive containment, however, was close contact with an asymptomatic carrier in unidentified situations other than health care in 22 cases (15.4%). In those cases, the infection rate was similar to that of the general population, with the second and third waves affecting young people to a greater extent than in the first wave (Fig. 2).
Sixty-nine residents worked at all times only in their ENT department (48.3%) and 53 did not miss a single day of work (37%), so the main loss of training was due to the reduction in overall care work and the need to work in other departments at critical times of the pandemic. Training losses due to sickness absence lasted between 1 and 2 months in the case of only 6 residents (4.2%), between 2 and 3 months in 3 (2.1%), and more than 3 months in only one (0.7%). The remaining 80 residents (56%) were absent from work for less than one month. Absences due to sickness and confinement, added to the performance outside ENT, and the reduction in ENT work itself, meant that the residents considered that they had lost a varying number of months of their training year, depending on the local incidence of the pandemic. It is very relevant that 60.1% of the residents considered that they had lost more than 6 months of their training time and that 18.8% had lost between 10 and 12 months. This is especially serious in a speciality that consists of only 4 years of training, with a high proportion of learning time devoted to surgical training.
Restrictions on geographical mobility and the imposition of social distancing among the population cancelled more than two thirds of the internal rotations and scheduled courses and visits in other centres. The lack of acquisition of deficient skill areas in the centres where residents undertook their training further limited the breadth of skills obtained by the resident at the end of their training period.
The reduction in face-to-face training activities of a theoretical nature was not totally replaced by their conversion into virtual sessions. This new format was well received and accepted by the trainees and will be included among the daily activities to be run in the future. It is also clear that face-to-face relational contact is a favourable factor when running theoretical training sessions. The acceptance and interest shown by 11.1% of the residents in furthering virtual surgery as a training methodology is a point to highlight. The conversion of ENT conferences into virtual formats has facilitated an increase in the participation of many residents at these conferences, compared to previous face-to-face situations, enabling them to produce more oral communications, posters and videos. Although the production of scientific articles has increased, most of the research activities requiring face-to-face tasks with patients or the laboratory have been delayed (48%) and for 4.9% of the residents, these were cancelled.
The training losses most highlighted by the residents were due to the decrease in surgical care work (Table 1 and Fig. 3), without affecting exploratory and diagnostic procedures to such an extent. The cancellation or postponement of elective interventions was one of the first and most widespread recommendations in guidelines and by scientific societies, and these procedures constitute the bulk of ENT residents' surgical training. ORL.20,21 Sixty-four percent of residents did not intervene as first or independent surgeon in more than 75% of the procedures planned by their residency course. This occurred in all major procedures for each year of residency, with greater relevance in the case of second and third-year residents, as they had less time to make up for unacquired skills than they should have gained. The procedures with the least recouping capacity were all otological procedures (myringoplasty, tympanoplasty with mastoidectomy, stapedectomy, cochlear implants) and rhinology procedures (endoscopic nasosinusal and anterior skull base surgery, septoplasty and turbinoplasty), which were also those most affected by the in theoretical training activities. These procedures constitute the key body of procedures for the training of ENT residents. ORL22 To this must be added the practical disappearance of cadaver simulation training, one of the foundations of ENT resident learning.23 In contrast, 43% of residents have been able to increase by more than 75% of usual rates their hands-on learning in performing tracheostomies, despite initial recommendations stating that this was not suitable for residents.24
Oncology surgery has been reduced in the last few years and has systematically fallen in all centres, mainly due to restrictions on access to primary care centres and travel between towns. This has mainly affected R3s and R4s, who have lost most of their training as they were able to perform a large number of these procedures as principal surgeons. There has been a greater presence of R1s and R2s in the operating theatres than would have been the case without the pandemic, so this activity is offset by the reduction in other health care work. The recommendations of health institutions to perform PCR tests for the detection of asymptomatic carriers between 24−72h before elective surgery and the increase in outpatient surgery theoretically increased the surgical capacity of many ENT services, however this possibility was restricted by the real limitation in the use of operating theatres and hospital beds, massively occupied during long periods of the pandemic by COVID-19 positive patients.
Except for the few cases of residents who have not seen their scheduled training substantially affected by working in centres less affected by the pandemic, more than half were in favour of extending their residency for at least 6months, (53%), up to 37.7% considered it necessary to extend training for a full year. The pandemic has affected residents in varying ways, depending on the geographical location of their training centre. Nevertheless, these figures are sufficiently convincing to prompt the health authorities to implement measures to remedy these training deficiencies.
The need has become clear to modify the methodology for monitoring the implementation of ENT training courses in Spain, currently delegated exclusively to the teaching committees at each hospital. It appears necessary to design national planning that ensures effective fairness in the training of all residents, regardless of the c. between where they undertake their training course, and to coordinate at national level the introduction of teaching methods, virtual and simulation techniques that could make up for the local shortcomings of ENT services that show deficits.7,25
ConclusionsInfected ENT residents have suffered mild disease in most cases and few have required hospital admission, having been infected presumably by contact with asymptomatic carriers during patient care, as well as by close contact with asymptomatic carriers in unidentified situations other than health care. Nonetheless, the vast majority of ENT residents have had their training capacity reduced due to the lower amount of care work undertaken in their ENT unit and also due to having practised in other hospital services during the most critical periods of the pandemic. During the pandemic, residents must apply the recommended protective measures against SARS-CoV-2 to all patients, especially those without symptoms suggestive of COVID-19, who are at the highest risk of real infection if protective measures are not adopted.
The conversion of face-to-face training activities into virtual ones has been widely accepted by ENT residents, however it has not been able to supply the totality of training activities required. The 6–12months lost by most residents represent a very relevant impact on the acquisition of competencies, especially in surgical training, which would require the extension of residency courses from 6months to a full year to recoup lost learning, especially in the most affected subareas of otology and rhinology, where there has been a reduction of more than 75% of planned training in myringoplasty, tympanoplasty with mastoidectomy, stapedectomy, cochlear implants, endoscopic nasosinusal and anterior skull base surgery, septoplasty and turbinoplasty.
Design of an operational training plan at national level is needed to ensure effective fairness in the training of all residents at national level in order to make up for the shortcomings of ENT services with deficits.
Conflict of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Sánchez-Gómez S, Maza-Solano JM, López Flórez L, Parente Arias P, Lobo Duro D, Palacios-García JM. Impacto de la pandemia COVID-19 en la formación de los residentes deotorrinolaringología. Acta Otorrinolaringol Esp. 2022;73:235–245.