Journal Information
Vol. 72. Issue 4.
Pages 262-264 (July - August 2021)
Share
Download PDF
More article options
Vol. 72. Issue 4.
Pages 262-264 (July - August 2021)
Case study
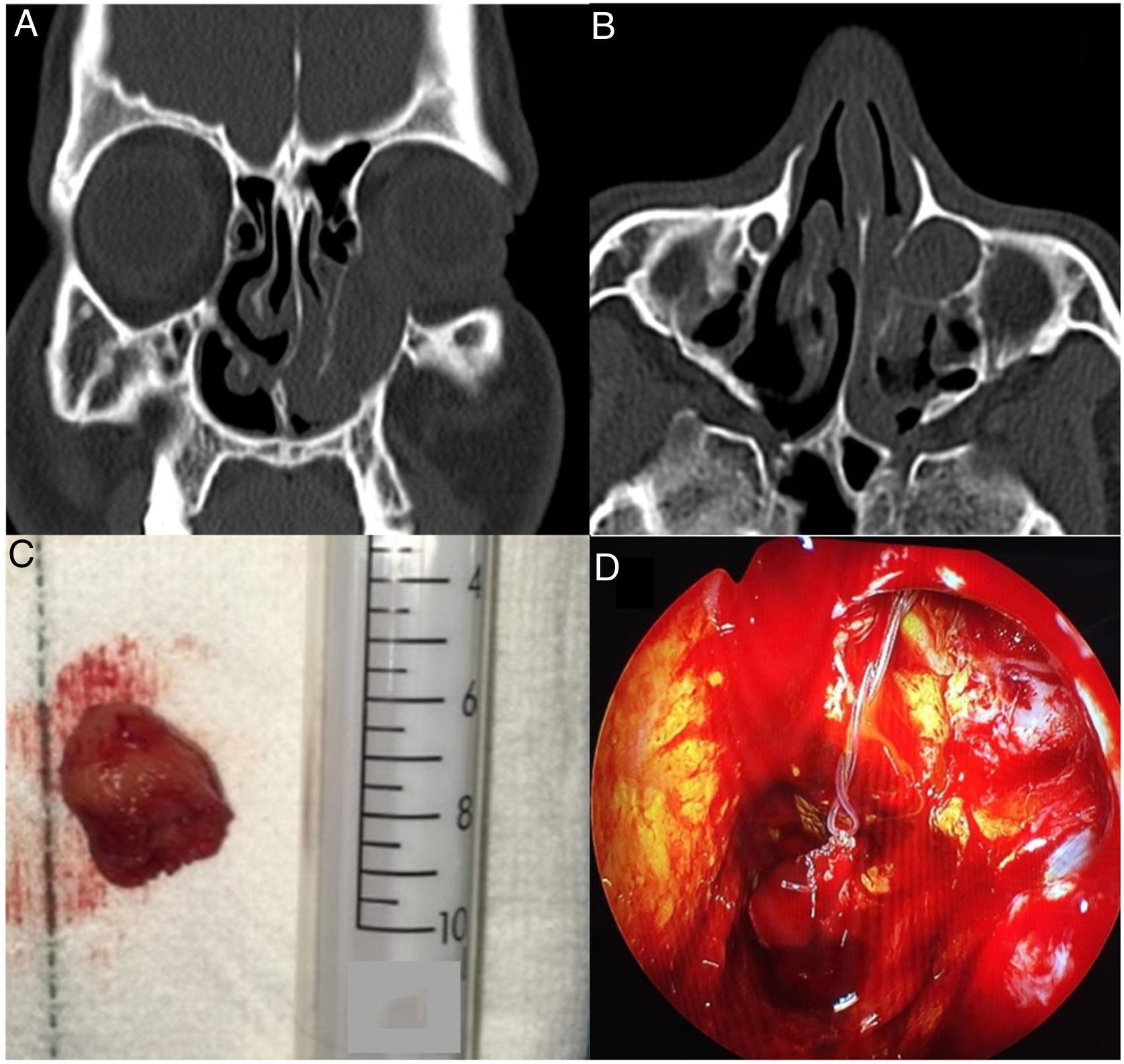
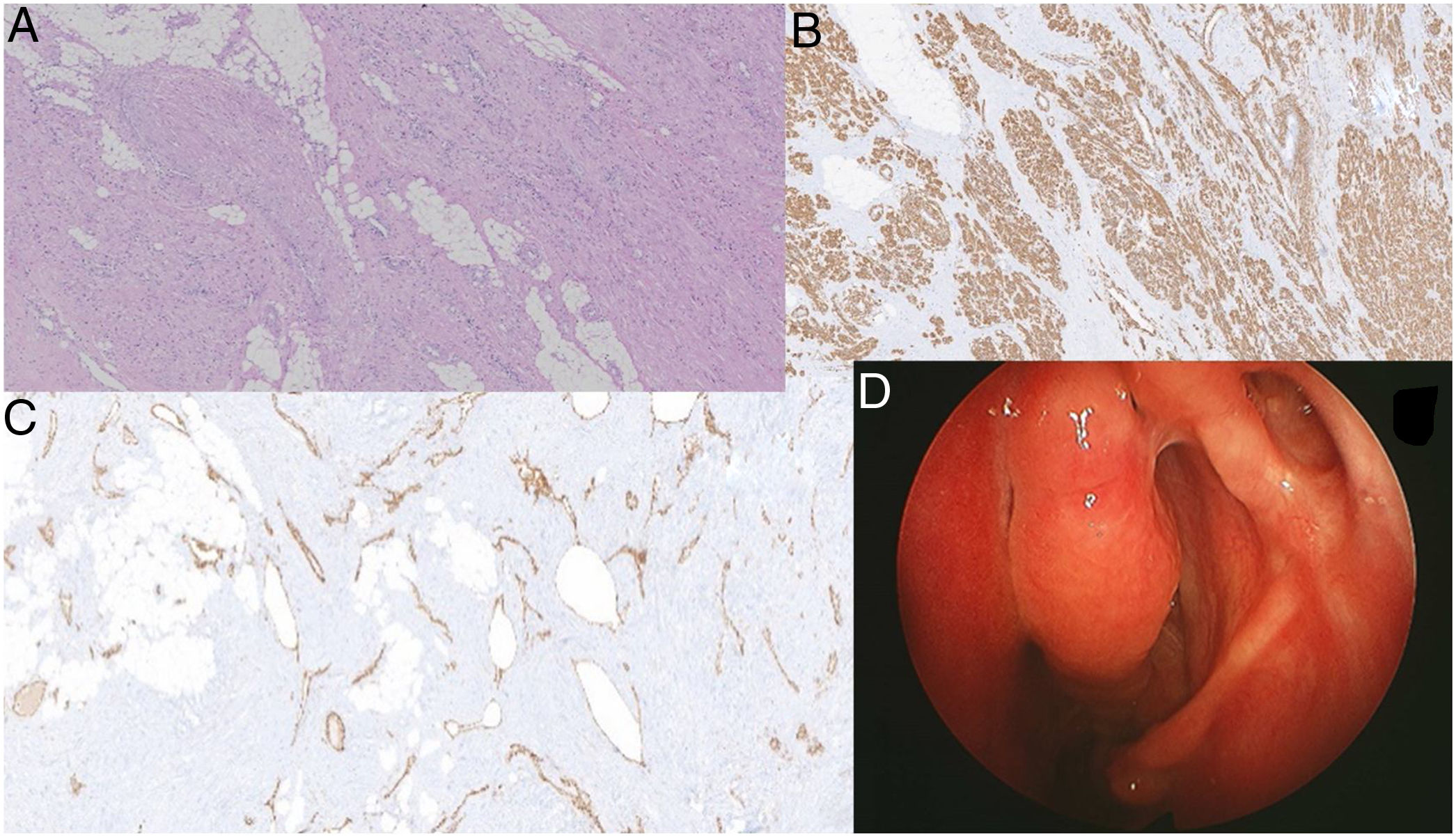
Lacrimonasal duct angioleiomyoma. A rare cause of obstruction of the lagrimal drainage system
Angioleiomioma del conducto lagrimonasal. Una rara causa de obstrucción de la vía lagrimal
Visits
5
Yolanda Escamilla Carpinteroa,
, María Teresa Sellares Fabresb, Carmen Blázquez Mañac, Mario Prenafeta Morenod
Corresponding author
a Servicio de ORL, Hospital Universitario Parc Taulí, Sabadell, Spain
b Servicio de Oftalmología, Hospital Universitario Parc Taulí, Sabadell, Spain
c Servicio de Patología, Hospital Universitario Parc Taulí, Sabadell, Spain
d Servicio de Radiodiagnóstico, UDIAT, Hospital Universitario Parc Taulí, Sabadell, Spain
This item has received
Article information
These are the options to access the full texts of the publication Acta Otorrinolaringológica Española
Subscriber
Subscribe
Purchase
Contact
Phone for subscriptions and reporting of errors
From Monday to Friday from 9 a.m. to 6 p.m. (GMT + 1) except for the months of July and August which will be from 9 a.m. to 3 p.m.
Calls from Spain
932 415 960
Calls from outside Spain
+34 932 415 960
E-mail