To analyze the current state of women in urology in Spain.
Material and methodsDescriptive study based on the results of an online survey sent between February and April 2020 through the database of the Residents and Young Urologists group (RAEU) of the Spanish Association of Urology (AEU). Characteristics of the survey and its results were analyzed.
ResultsIn total, 257 responses were obtained from 210 women (81.71%) and 47 men (18.29%) belonging to 111 hospitals. Statistically significant differences were observed (p < 0.001) with a higher proportion of men in all categories except for the group of young female and male attendings (29−39 years, p = 0.789), and the group of female residents against male residents (p = 0.814). The number of men was higher in hospitals with subspecialty units except for the Pelvic Floor Unit, where no statistically significant difference was observed (p = 0.06). Regarding positions of responsibility, only 7 out of 111 hospitals had female Department Chiefs.
ConclusionsWomen's representation in urology is increasing, mainly due to the younger generations. However, the access of these women to relevant positions is anecdotal.
Analizar la situación actual de las mujeres en la Urología en España.
Material y métodosEstudio descriptivo a partir de los resultados de una encuesta electrónica remitida entre febrero y abril de 2020 a través de la base de datos del grupo de Residentes y Jóvenes Urólogos (RAEU) de la Asociación Española de Urología (AEU). Se analizaron las características demográficas de la encuesta y los resultados de la misma.
ResultadosSe obtuvieron 257 respuestas, de 210 mujeres (81,71%) y 47 hombres (18,29%) procedentes de 111 hospitales en total. Se obtuvieron diferencias estadísticamente significativas (p < 0,001) con una mayor proporción de hombres en todas las categorías excepto en el grupo de adjuntas y adjuntos jóvenes (29−39 años, p = 0,789) y en el de residentes mujeres frente a residentes hombres (p = 0,814). En los hospitales con unidades subespecializadas, se encontraron mayor número de hombres en todas, excepto en la Unidad de Suelo Pélvico, en la que no se observó una diferencia estadísticamente significativa (p = 0,06). Respecto a cargos de responsabilidad, en sólo 7 de 111 hospitales había Jefas de Servicio.
ConclusionesLa presencia de las mujeres en la especialidad de Urología es cada vez mayor, debido mayoritariamente a las generaciones más jóvenes. Sin embargo, el acceso de estas mujeres a puestos de relevancia es anecdótica.
In recent decades, the incorporation of women into the world of work and qualified studies has been on the rise. In medical schools, the number of female students has increased notably, reaching 50% in countries such as the U.S. and Canada.1 In Spain, this tendency has been even more significant, with nearly 74% of female medical students.2 Despite this, there are specialties with a smaller female presence, mainly surgical specialties such as Urology.3
This "feminization of medicine" has generated worldwide interest in the role of women in different medical areas; for example, female representation in scientific manuscripts, meetings4, or awards.5 However, there have been few analyses performed on the actual number of women in the physician workforce in different fields.
For these reasons, the aim of this article is to evaluate the state of female urologists in Spain with a descriptive analysis carried out through a nationwide survey.
Material and methodsData collectionUsing the database of the Residents and Young Urologists Group (RAEU) of the Spanish Urology Association (AEU), 452 invitations were sent to physicians aged under 35 years and Urology residents between February and April 2020. Three reminders were sent during these months. Survey responses were anonymous. Google Forms was used to generate the survey.
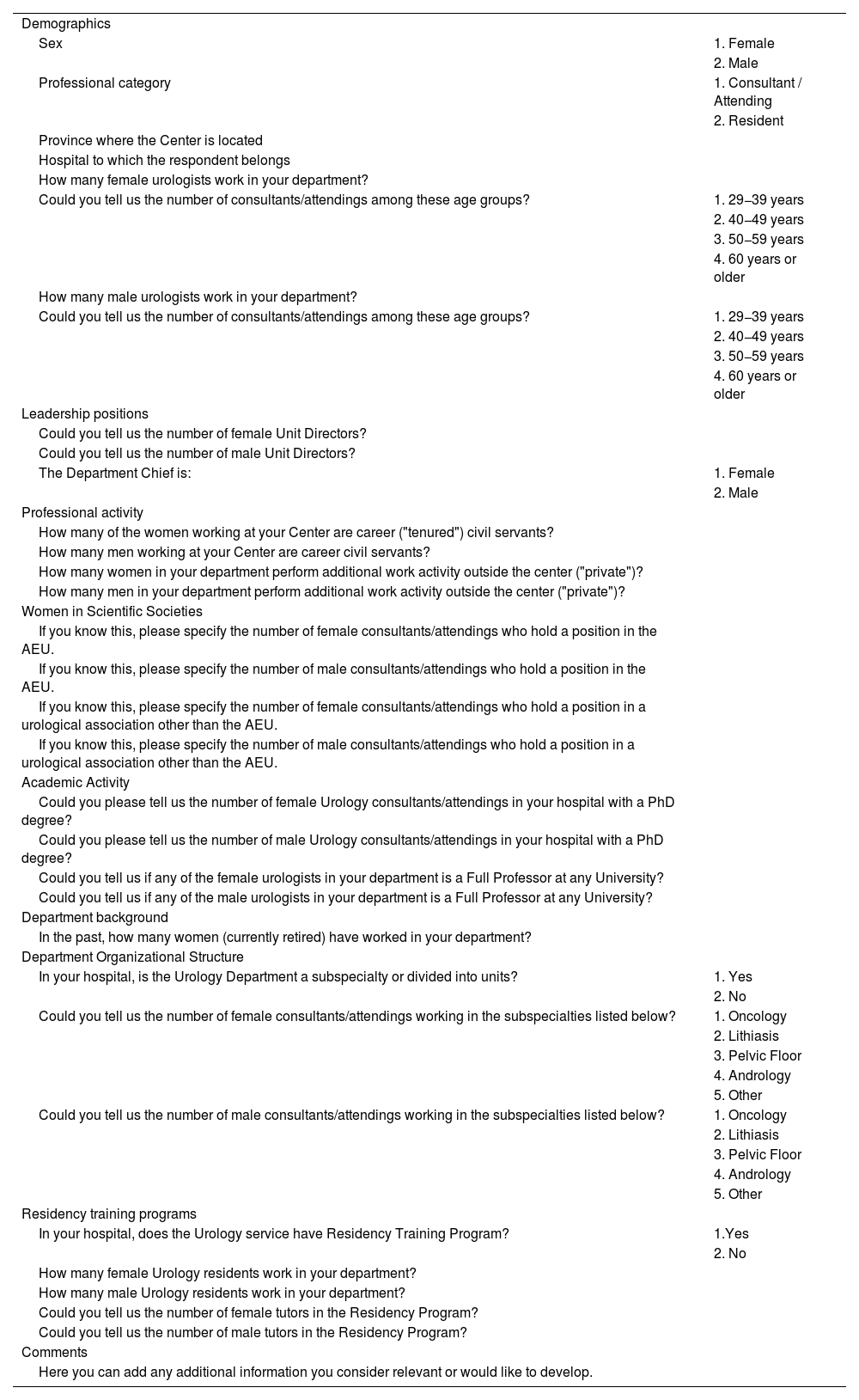
The surveyThe survey consisted of 33 questions, grouped into 8 different sections (Table 1).
The survey.
| Demographics | |
| Sex | 1. Female |
| 2. Male | |
| Professional category | 1. Consultant / Attending |
| 2. Resident | |
| Province where the Center is located | |
| Hospital to which the respondent belongs | |
| How many female urologists work in your department? | |
| Could you tell us the number of consultants/attendings among these age groups? | 1. 29−39 years |
| 2. 40−49 years | |
| 3. 50−59 years | |
| 4. 60 years or older | |
| How many male urologists work in your department? | |
| Could you tell us the number of consultants/attendings among these age groups? | 1. 29−39 years |
| 2. 40−49 years | |
| 3. 50−59 years | |
| 4. 60 years or older | |
| Leadership positions | |
| Could you tell us the number of female Unit Directors? | |
| Could you tell us the number of male Unit Directors? | |
| The Department Chief is: | 1. Female |
| 2. Male | |
| Professional activity | |
| How many of the women working at your Center are career ("tenured") civil servants? | |
| How many men working at your Center are career civil servants? | |
| How many women in your department perform additional work activity outside the center ("private")? | |
| How many men in your department perform additional work activity outside the center ("private")? | |
| Women in Scientific Societies | |
| If you know this, please specify the number of female consultants/attendings who hold a position in the AEU. | |
| If you know this, please specify the number of male consultants/attendings who hold a position in the AEU. | |
| If you know this, please specify the number of female consultants/attendings who hold a position in a urological association other than the AEU. | |
| If you know this, please specify the number of male consultants/attendings who hold a position in a urological association other than the AEU. | |
| Academic Activity | |
| Could you please tell us the number of female Urology consultants/attendings in your hospital with a PhD degree? | |
| Could you please tell us the number of male Urology consultants/attendings in your hospital with a PhD degree? | |
| Could you tell us if any of the female urologists in your department is a Full Professor at any University? | |
| Could you tell us if any of the male urologists in your department is a Full Professor at any University? | |
| Department background | |
| In the past, how many women (currently retired) have worked in your department? | |
| Department Organizational Structure | |
| In your hospital, is the Urology Department a subspecialty or divided into units? | 1. Yes |
| 2. No | |
| Could you tell us the number of female consultants/attendings working in the subspecialties listed below? | 1. Oncology |
| 2. Lithiasis | |
| 3. Pelvic Floor | |
| 4. Andrology | |
| 5. Other | |
| Could you tell us the number of male consultants/attendings working in the subspecialties listed below? | 1. Oncology |
| 2. Lithiasis | |
| 3. Pelvic Floor | |
| 4. Andrology | |
| 5. Other | |
| Residency training programs | |
| In your hospital, does the Urology service have Residency Training Program? | 1.Yes |
| 2. No | |
| How many female Urology residents work in your department? | |
| How many male Urology residents work in your department? | |
| Could you tell us the number of female tutors in the Residency Program? | |
| Could you tell us the number of male tutors in the Residency Program? | |
| Comments | |
| Here you can add any additional information you consider relevant or would like to develop. |
The responses to each item were analyzed and compared based on the sex of the specialists (for example, the number of female urologists versus the number of male urologists, etc.). The mean, median, mode, and standard deviation (SD) of each response were obtained. The mean of each response and its SD were compared by the Student's T test. Statistical significance was determined at p < 0.05. The program used was R version 3.6.2 (free software) and the SPSS v27 statistical package.
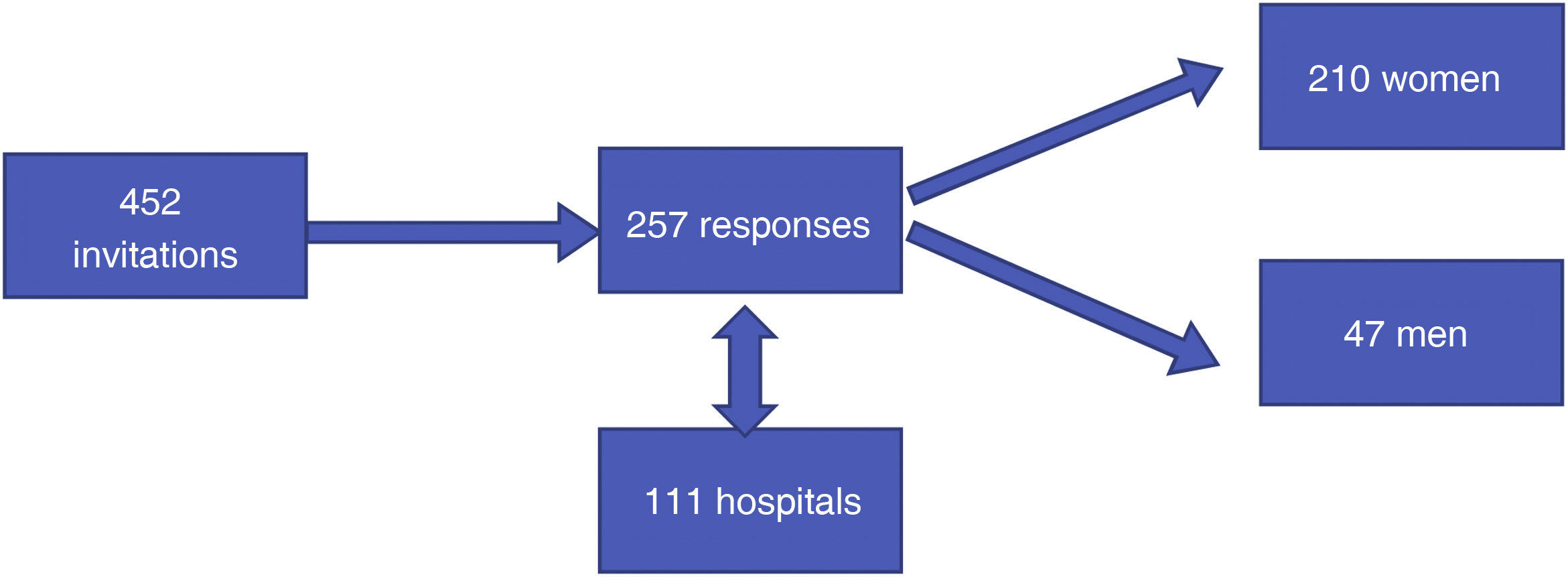
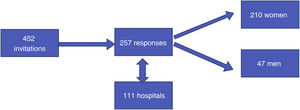
ResultsDemographicsOf the 452 survey invitations, 257 responses were obtained (56.85% of the respondents). A total of 210 women (81.71%) and 47 men (18.29%) completed the survey. The 257 responses were grouped by hospitals, resulting in 111 hospitals (Fig. 1).
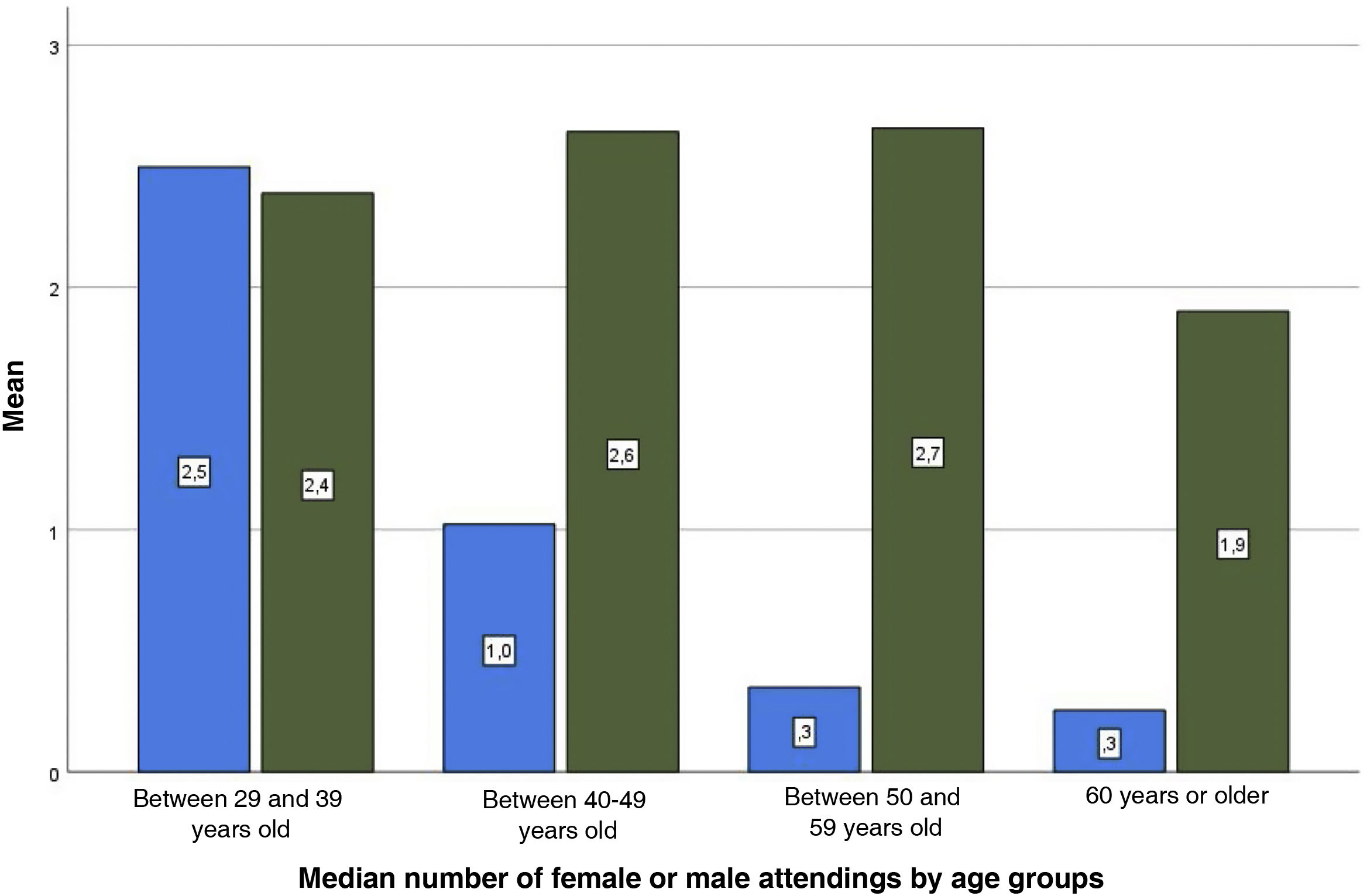
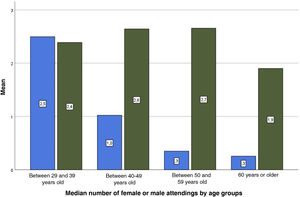
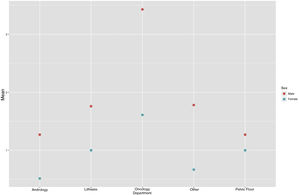
The median numbers of female versus male attending physicians were 3.14 (31.87%) and 7.56 (68.13%) respectively, with a statistically significant result (p < 0.001). This question was further subdivided into age ranges (29−39; 40−49; 50−59; 60 or older). The only age range without statistical significance and with a much more adjusted result was the youngest group (29−39 years) with a mean of 2.52 females versus a mean of 2.41 males (p = 0.79) (Fig. 2).
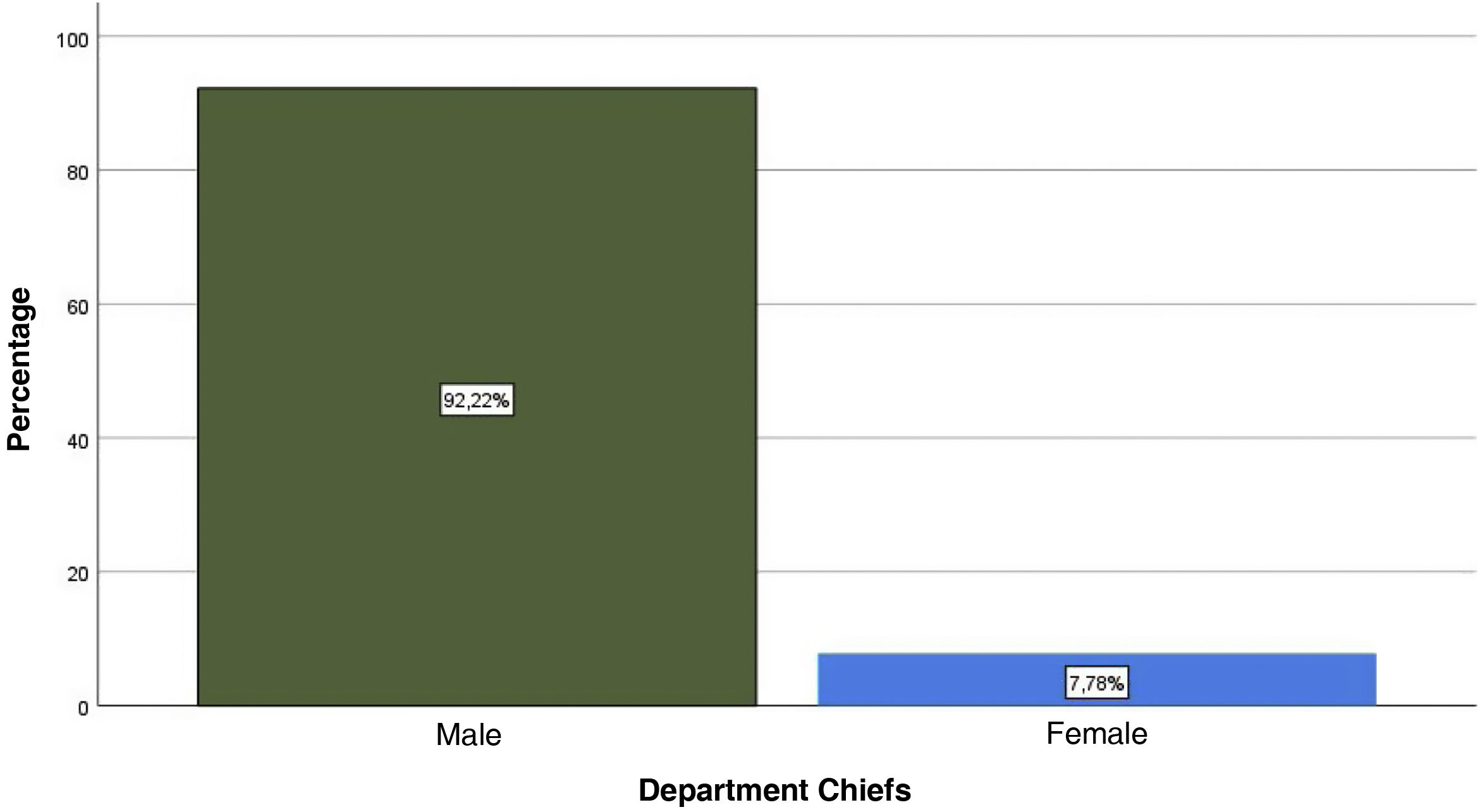
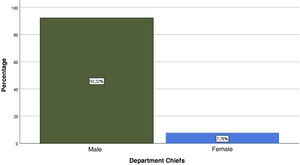
Leadership positionsRegarding Unit Directors, mean values of 0.17 women and 1.36 men (p < 0.0001) were obtained. Regarding Department Chiefs, of the 111 hospitals that responded to the survey, 104 hospitals had male Department Chiefs (92.2%) and 7 hospitals had female Department Chiefs (7.78%) (Fig. 3).
Professional career, scientific societies, academic activityThere was a statistically significant difference favoring the male sex in all these variables (p < 0.001).
Department backgroundWe obtained 106 responses on the number of women who had worked in the Department and had already retired. Eighty-seven hospitals reported not having previous female employees already retired, 16 departments informed there had been 1, 1 hospital mentioned 2, and another hospital informed of 4 already retired female employees.
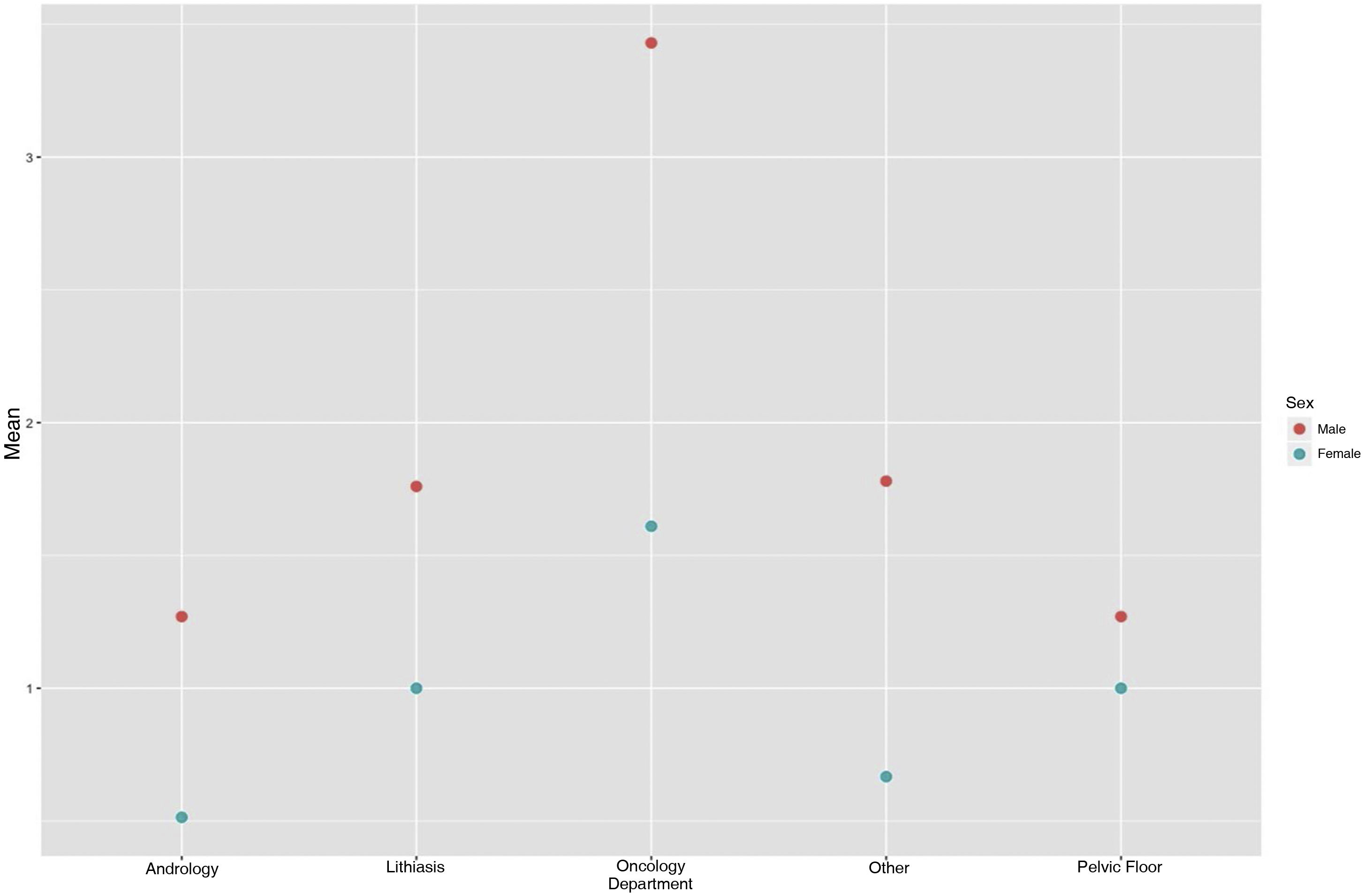
Department organizational structureOf the 111 hospitals, 67 (60.4%) had units, while 44 (35.6%) did not. In the subspecialty hospitals, we asked about the number of urologists in each unit. The only unit with no statistically significant difference (mean 1 vs. 1.76) was Pelvic Floor (p = 0.06). The male representation predominated in the remaining units (p < 0.001): Oncology (3.82 vs. 1.75), Lithiasis (2.02 vs. 0.93), and Andrology (1.49 vs. 0.53) (Fig. 4).
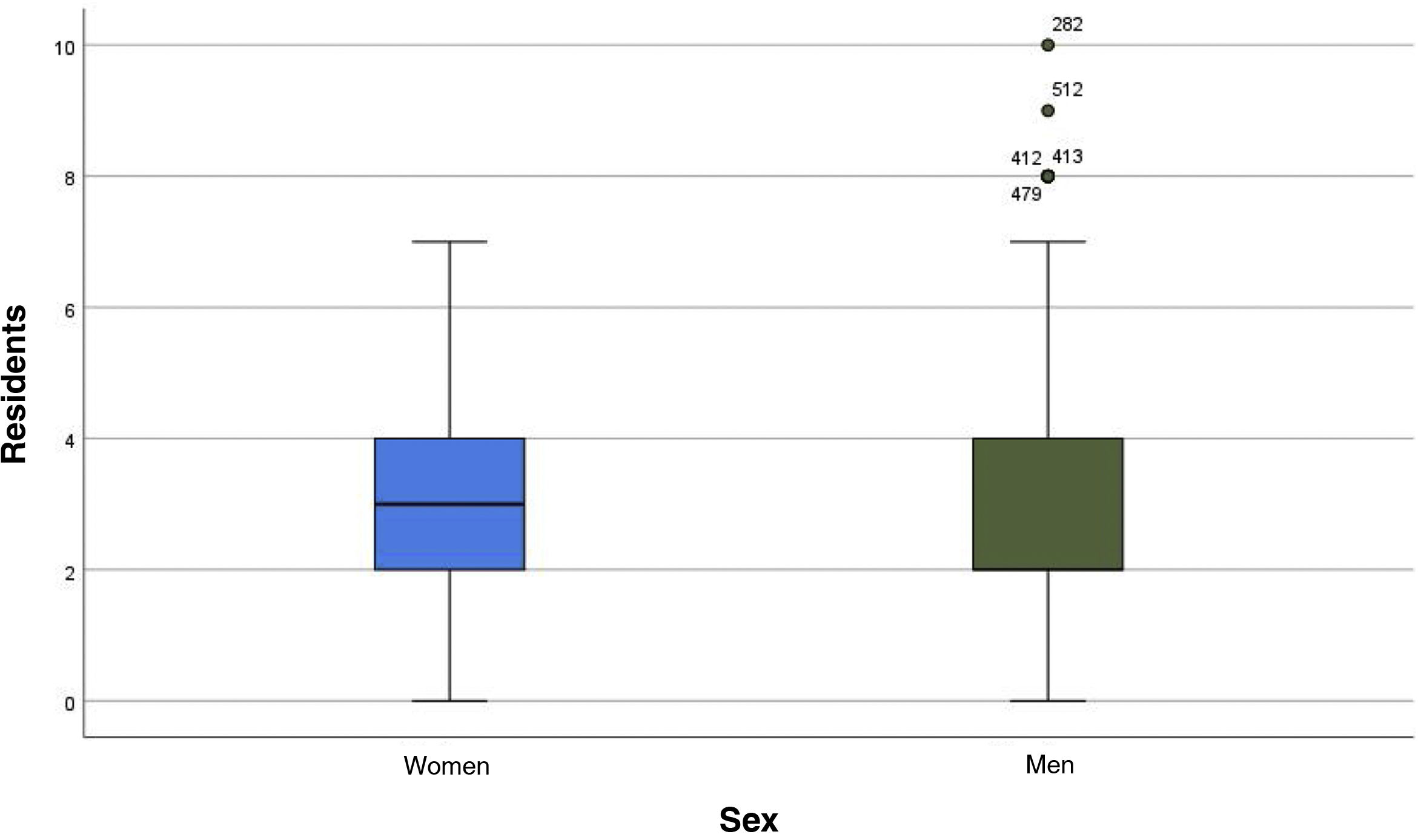
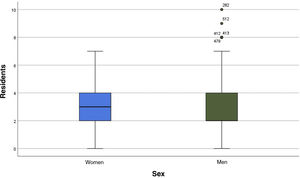
Residency programsOf the 111 hospitals, 39 (35.1%) did not have residency programs and 72 (64.9%) did. Women obtained a higher mean number than men (3 vs. 2) (Fig. 5) in these programs. As for the number of female and male tutors, the male representation was predominant (p < 0.001).
DiscussionUrology has traditionally been a male dominated field. However, there is a clear trend towards feminization of this specialty, not only in Spain, but also in countries such as the U.S.6
When analyzing the number of attendings according to age group, the number of female urologists increases as age decreases. This result is comparable to studies carried out in the U.S. 7. Similarly, there is an increasing number of female residents from 1978 to 2013, rising from 0.9% to 23.8%.3 In this sense, the results of the survey regarding Residency Programs show that the number of women choosing Urology is tends to increase. This escalating female representation is also reflected in specialties such as General Surgery.8,9 However, in Neurosurgery or Orthopedic and Trauma Surgery, it is much lower.10–12 According to some authors, the very perception that being a woman is a disadvantage in her professional career means that women have less access to those professions traditionally perceived as ‘male’ fields.13 On the other hand, the lack of female referents also reduces the interest of female medical students in joining these areas. Particularly significant is the scarce representation in meetings, lectures, or webinars.4,14
Regarding positions of responsibility, these usually belong to men.15 The survey shows a significant difference. This can be due to the fact that the most qualified women for the position, in terms of experience and age, i.e., those over 50 years old, are fewer than the men of the same rank. Therefore, it can be deduced that the number of women and men in leadership will eventually equalize. And, if time is the determining factor, the number of women should become even higher, since there are already more female urologists than male urologists in the younger ranks, according to the results of this survey.
Several studies evaluate the so-called "glass ceiling" effect in medicine.16–18 According to Zhuge et al.,17 three major barriers contribute to this fact: traditional gender roles, a "sexist" environment, and a lack of mentors, especially female mentors.16 The absence of mentorship and visibility is especially relevant in the academic environment,19–21 resulting in the absence of role models and mentors to follow, especially among the younger ones.
Regarding subspecialty units, Pelvic Floor has traditionally been associated with women.22,23 In the survey, it is the only specialty with no statistically significant differences between men and women. Despite this, the number of female speakers at Functional Urology meetings remains low.24
The main limitation of the study is the population of the survey, as it did not include all hospitals in Spain. The study population derived from the database corresponds only to young female or male attendings and residents (under 35 years of age). However, the survey presents strictly objective questions that can be responded by only one person from each Urology Department, so the potential selection bias does not influence the results of the survey.
Despite its limitations, the survey constitutes a turning point in the knowledge of the demographic situation of urology in Spain, and it could be the starting point for more surveys to expose the evolution of these demographics. Further surveys could be considered to shed light on whether the lack of women in positions of responsibility is a time-determined factor or, on the contrary, there is a glass ceiling.
ConclusionsWe have seen that the number of female residents slightly exceeds the number of male residents in Spain. Specialties such as Functional Urology have a higher female representation compared to other subspecialties. However, the number of female urologists in leadership positions is still anecdotal. Further studies would be necessary to assess whether the increase of women in the older age ranges, assuming age and experience as key factors for access to these positions, is correlated with an increased number of women in leadership positions.
FundingThe authors of this manuscript did not receive any funding.
In the first place, we would like to thank all those who took the time to complete the survey. To Dr. Mariano Pérez Albacete for his relentless search and for being one of the first urologists to study the role of the female specialist in Urology. To Diego Carrión Monsalve and Daniel González Padilla for their contributions. To the members of the Residents and Young Urologists group: Marta Antón, Clàudia Mercader, Luis Enrique Ortega. To Alejandro Moya, statistician at the General University Hospital of Elche for his analysis and statistical advice on the work. To Jesús Campo Martínez, statistician, for his final collaboration. To Lucía Sánchez Cózar, for her invaluable help and patience.