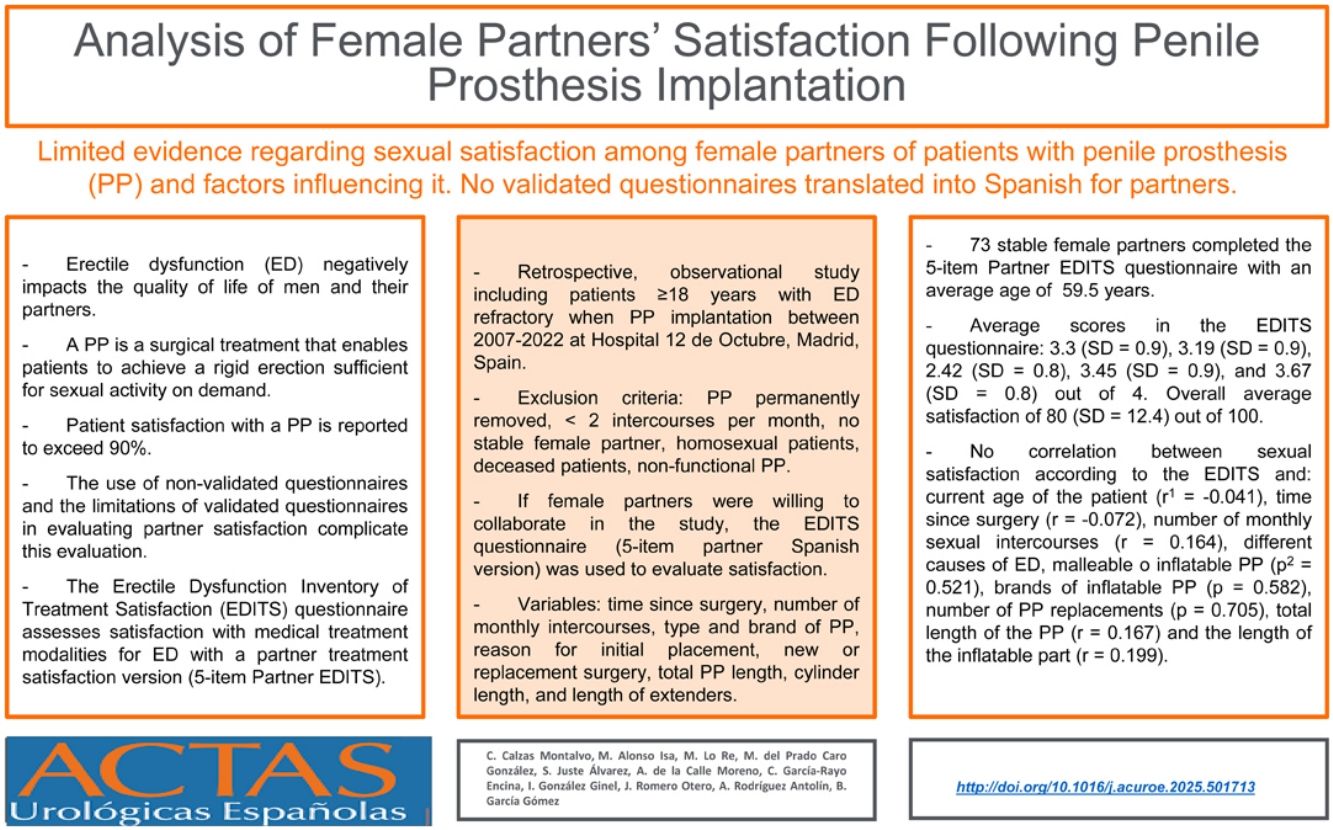
There is limited evidence regarding sexual satisfaction among female partners of patients with penile prosthesis (PP) and factors influencing it.
Materials & methodsSingle-center, retrospective, observational study including all patients aged ≥18 years who underwent PP implantation (inflatable and malleable types) between October 2007-December 2022 at Hospital 12 de Octubre, Madrid, Spain. 73 female partners completed the Erectile Dysfunction Inventory of Treatment Satisfaction (EDITS) questionnaire (5-item partner version). Each question was scored from 0 (lowest satisfaction) to 4 (highest satisfaction), resulting in an overall EDITS score ranging from 0 to 100. Variables collected: time since surgery, monthly intercourse frequency, type and brand of PP, initial placement rationale, new versus replacement surgery, total and inflatable PP part length.
ResultsAverage (standard deviation) scores were: 3.3 (0.9), 3.19 (0.9), 2.42 (0.8), 3.45 (0.9), and 3.67 (0.8). The overall average satisfaction score was 80 (12.4). Statistical analysis revealed no significant correlations between female partners' satisfaction and their age (r = −0.128), actual age of the patient (r = −0.041), time since surgery (r = −0.072), monthly intercourse frequency (r = 0.164), type of PP (p = 0.521), brand of inflatable PP (p = 0.582), causes of erectile dysfunction (p = 0.174), number of replacements (p = 0.705), total (r = 0.167) or inflatable PP part length (r = 0.134).11
PP: penile prosthesis. EDITS: Erectile Dysfunction Inventory of Treatment Satisfaction.
ConclusionsSexual satisfaction among female partners in our cohort is high but we did not demonstrate any predictors of couple satisfaction.
Existen pocos datos sobre la satisfacción sexual de las parejas femeninas de pacientes con prótesis de pene (PP) y los factores que influyen en ella.
Materiales y métodosEstudio observacional, retrospectivo, unicéntrico, que incluyó a todos los pacientes de ≥18 años sometidos a la implantación de una PP (inflable y maleable) entre octubre de 2007 y diciembre de 2022 en el Hospital 12 de Octubre, Madrid, España. En total, 73 parejas femeninas completaron el cuestionario Erectile Dysfunction Inventory of Treatment Satisfaction (EDITS) (versión para parejas de 5 ítems). Cada pregunta se puntuó de 0 (menor satisfacción) a 4 (mayor satisfacción), dando como resultado una puntuación EDITS global que osciló entre 0 y 100. Variables recogidas: tiempo transcurrido desde la cirugía, frecuencia mensual de las relaciones sexuales, tipo y marca de la PP, motivo inicial de la implantación, cirugía nueva frente a cirugía de sustitución, longitud total y de la parte inflable de la PP.
ResultadosLas puntuaciones medias (desviación estándar) fueron: 3,3 (0,9), 3,19 (0,9), 2,42 (0,8), 3,45 (0,9) y 3,67 (0,8). La puntuación media de satisfacción global fue de 80 (12,4). El análisis estadístico no reveló correlaciones significativas entre la satisfacción de la pareja femenina y su edad (r = -0,128), la edad actual del paciente (r = -0,041), el tiempo transcurrido desde la intervención (r = -0,072), la frecuencia mensual de las relaciones sexuales (r = 0. 164), el tipo de PP (p = 0,521), la marca de la PP inflable (p = 0,582), causas de la disfunción eréctil (p = 0,174), número de sustituciones (p = 0,705), longitud total (r = 0,167) o de la parte hinchable de la PP (r = 0,134).22
PP: Prótesis de pene. EDITS: Inventario de Satisfacción con el Tratamiento de la Disfunción Eréctil.
ConclusionesLa satisfacción sexual entre las parejas femeninas de nuestra cohorte es elevada, pero no hemos encontrado evidencia de factores predictivos de la satisfacción de la pareja.
Erectile dysfunction (ED) is defined as the persistent inability to initiate and maintain an erection sufficient to permit satisfactory sexual performance.1 In men aged 50–80 years, the overall prevalence of ED is 48.7%.2 ED negatively impacts the quality of life of both men and their partners and can be an early manifestation of cardiovascular disease.3
A penile prosthesis (PP) is a surgical treatment option offered to patients who are either unsuitable for or unresponsive to other treatment modalities or who prefer a definitive therapy.4 The PP enables patients to achieve a rigid erection sufficient for sexual activity on demand with excellent long-term outcomes.5 The two currently available types of PP include inflatable (two- and three-piece) penile prosthesis (IPP) and malleable (semi-rigid mechanical, soft flexible) penile prosthesis (MPP). Although IPPs provide a more natural appearance in both erect and flaccid states, no prospective randomized controlled trial has compared patient satisfaction rates between these two types of implants.4
Patient satisfaction with a PP has been widely studied and is reported to exceed 90%.5 While it is postulated that sexual function reinforces pair-bonding in couples, there is limited evidence regarding sexual satisfaction among female partners of patients with a PP and the factors that may contribute to it.6–23 Furthermore, the widespread use of non-validated questionnaires and the limitations of validated questionnaires in evaluating patient and partner satisfaction complicate this evaluation.24 Additionally, there are no validated questionnaires translated into Spanish for partners, which further complicates the assessment of couple satisfaction with a PP.3
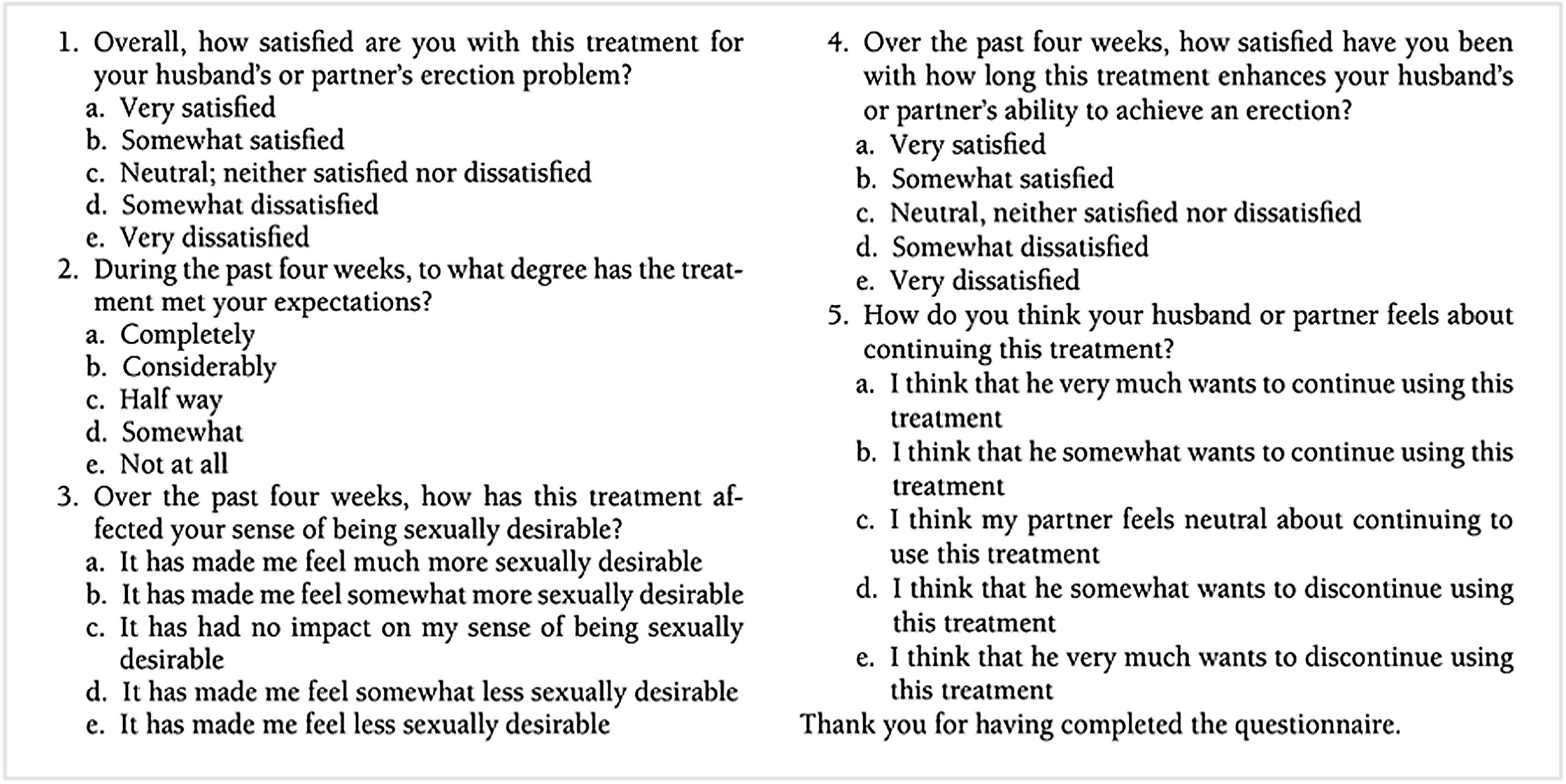
The Erectile Dysfunction Inventory of Treatment Satisfaction (EDITS) questionnaire was developed in 1999 to assess satisfaction with medical treatment modalities for ED.25 One version is intended to assess patient treatment satisfaction (11-item Patient EDITS), and to assess partner treatment satisfaction (5-item Partner EDITS).
The aim of this study is to investigate sexual satisfaction among female partners of patients undergoing PP implantation and to assess the different variables that may be related to it.
Materials & methodsSubject selectionWe conducted a single-center, retrospective, observational study including all patients aged ≥18 years at the time of PP implantation (IPP and MPP), performed between October 2007 and December 2022 at Hospital 12 de Octubre, Madrid, Spain. All surgeries were performed by the same three experienced andrologists.
The patient population included those with ED refractory to oral pharmacotherapy and/or topical/intraurethral alprostadil, and those who failed or rejected penile injection therapy due to ineffectiveness or intolerance. All participants signed written consent prior to surgery.
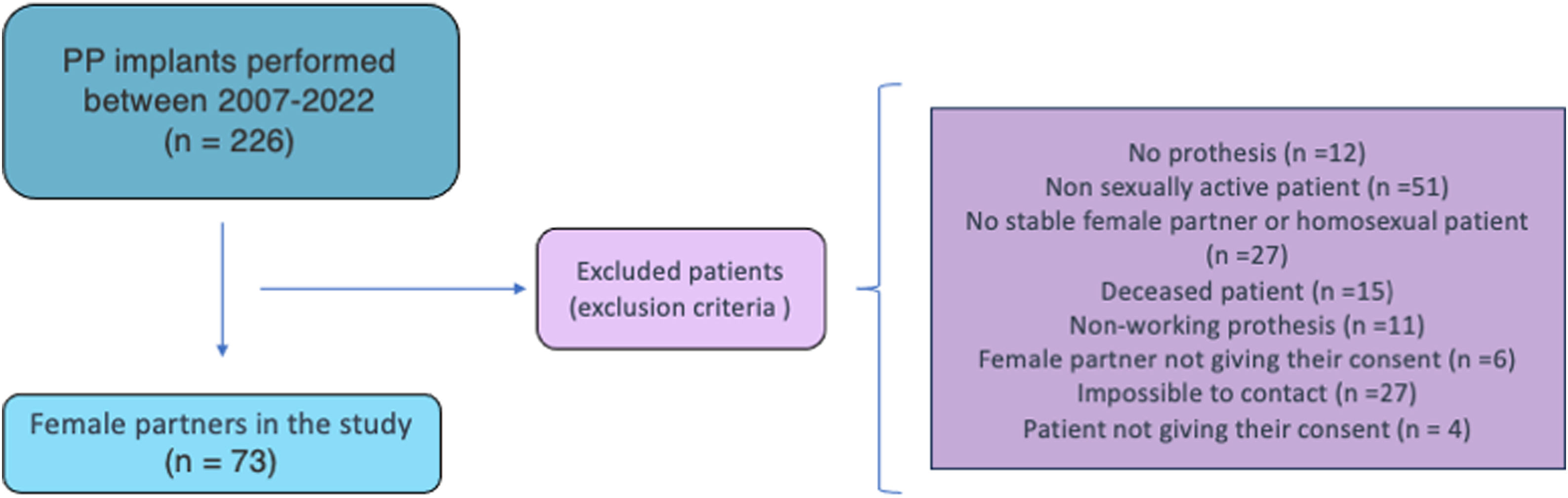
Patients were contacted by phone in December 2023 and asked if they were willing to participate in the study. Exclusion criteria were: PP permanently removed at the time of the interview, non-sexually active patients (defined as fewer than 2 intercourses per month, as an arbitrary definition for our study), absence of a stable female partner, homosexual patients, deceased patients, non-functional PP for any reason, patients or female partners not giving their consent, loss of follow-up or inability to contact them. Consequently, 73 questionnaires were completed by female partners (Fig. 1, flow chart: patient recruitment).
Variables collectedPatient characteristics, including demographics and comorbidities, perioperative complications and postoperative follow-up details were collected retrospectively from the electronic clinical database. We also collected variables potentially related to sexual satisfaction: time since surgery, number of monthly intercourses, type and commercial brand of PP (Coloplast®, Humlebaek, Denmark or Boston Scientific®, Marlborough, Massachusetts, USA), reason for initial placement, new or replacement surgery, total PP length, cylinder length, and length of extenders, if any, among others.
Patients were asked if their female partners were willing to collaborate in the study. If so, the EDITS questionnaire4 (5-item partner Spanish version),26 was used to evaluate partner satisfaction through a telephone interview conducted in a private room to avoid patient influence. Each question was scored from 4 (best satisfaction) to 0 (no satisfaction), and the EDITS score (mean of the individual item scores multiplied by 25) ranged from 100 (extremely high treatment satisfaction) to 0. Partners were also asked how challenging they considered the management of the PP using a Likert scale ranging from 0 (very easy) to 6 (very difficult).
Patients and their partners provided verbal informed consent for the use of their health data in this scientific research study.
Statistical analysisCategorical variables were presented as frequencies expressed as percentages. Quantitative variables were presented as means and standard deviations (SD).4 Statistical analysis was based on descriptive analysis, the Mann-Whitney U test, and the Pearson correlation5 coefficient. Data were analyzed using the Statistical Package for Social Sciences version 23.0 (SPSS Inc., Chicago, Illinois, USA).
Results73 stable female partners completed the 5-item Partner EDITS questionnaire (Fig. 2) at least one year after PP surgery. The average partner age was 59.5 years (SD = 10.8). The time since surgery ranged from 12 to 168 months, with an average of 58.6 months (SD = 44.8). The average number of sexual intercourses per month was 6.5 (SD = 6.8).
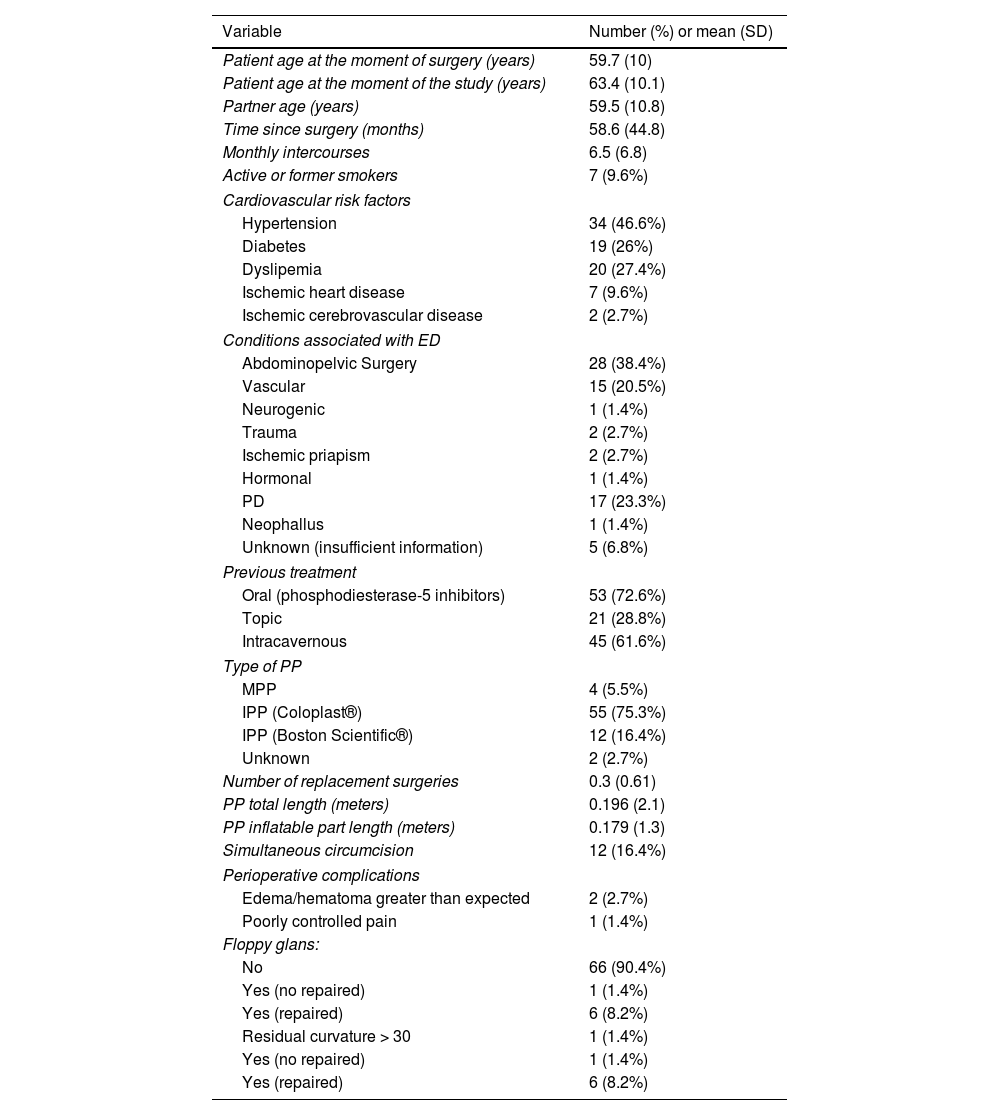
Baseline and PP characteristics of the 73 patients and partners are shown in Table 1. The average patient age at the time of the questionnaire was 63.4 years (SD = 10.1). 43 (58.9%) patients had a cardiovascular risk factor, predominantly hypertension in 34 (46.6%). Additionally, 22 (30.1%) patients were smokers or former smokers and 7 (9.6%) had ischemic heart disease. The most common condition associated with ED in our cohort was previous abdominopelvic surgery (radical prostatectomy or radical cystoprostatectomy, among others) in 28 (38.4%) patients. The second most common condition associated with ED was Peyronie's disease (PD) not responding to conventional medical therapy (n = 17, 23.3%), resulting in no curvature or minimal residual curvature after PP implantation. In 2 (2.5%) patients with ischemic priapism lasting more than 48 h, an early PP was implanted.
Baseline characteristics of the patients in the cohort.
| Variable | Number (%) or mean (SD) |
|---|---|
| Patient age at the moment of surgery (years) | 59.7 (10) |
| Patient age at the moment of the study (years) | 63.4 (10.1) |
| Partner age (years) | 59.5 (10.8) |
| Time since surgery (months) | 58.6 (44.8) |
| Monthly intercourses | 6.5 (6.8) |
| Active or former smokers | 7 (9.6%) |
| Cardiovascular risk factors | |
| Hypertension | 34 (46.6%) |
| Diabetes | 19 (26%) |
| Dyslipemia | 20 (27.4%) |
| Ischemic heart disease | 7 (9.6%) |
| Ischemic cerebrovascular disease | 2 (2.7%) |
| Conditions associated with ED | |
| Abdominopelvic Surgery | 28 (38.4%) |
| Vascular | 15 (20.5%) |
| Neurogenic | 1 (1.4%) |
| Trauma | 2 (2.7%) |
| Ischemic priapism | 2 (2.7%) |
| Hormonal | 1 (1.4%) |
| PD | 17 (23.3%) |
| Neophallus | 1 (1.4%) |
| Unknown (insufficient information) | 5 (6.8%) |
| Previous treatment | |
| Oral (phosphodiesterase-5 inhibitors) | 53 (72.6%) |
| Topic | 21 (28.8%) |
| Intracavernous | 45 (61.6%) |
| Type of PP | |
| MPP | 4 (5.5%) |
| IPP (Coloplast®) | 55 (75.3%) |
| IPP (Boston Scientific®) | 12 (16.4%) |
| Unknown | 2 (2.7%) |
| Number of replacement surgeries | 0.3 (0.61) |
| PP total length (meters) | 0.196 (2.1) |
| PP inflatable part length (meters) | 0.179 (1.3) |
| Simultaneous circumcision | 12 (16.4%) |
| Perioperative complications | |
| Edema/hematoma greater than expected | 2 (2.7%) |
| Poorly controlled pain | 1 (1.4%) |
| Floppy glans: | |
| No | 66 (90.4%) |
| Yes (no repaired) | 1 (1.4%) |
| Yes (repaired) | 6 (8.2%) |
| Residual curvature > 30 | 1 (1.4%) |
| Yes (no repaired) | 1 (1.4%) |
| Yes (repaired) | 6 (8.2%) |
SD: standard deviation. ED: erectile dysfunction. PD: Peyronie’s disease. PP: penile prosthesis. MPP: malleable penile prosthesis. IPP: Inflatable penile prosthesis.
The vast majority of patients had prior treatment for ED. Most of them started with phosphodiesterase-5 inhibitors with or without intraurethral treatment, attempting penile injection therapy if they were willing to do so. 53 (72.6%), 21 (28.8%), and 45 (61.6%) patients tried phosphodiesterase-5 inhibitors, intraurethral alprostadil and intracavernous injection therapy, respectively.
Regarding the type of PP used in our study, selection was based on the baseline characteristics of the patient and their preferences. A MPP was implanted in 4 (5.5%) patients, while an IPP was chosen for 67 (91.7%) patients. The type of PP was unknown in 2 (2.5%) patients due to lack of references in the surgical protocol, particularly in cases operated on more than 10 years ago, before the establishment of electronic clinical databases. Simultaneous circumcision was performed in 12 (16.4%) patients during PP surgery.
Among the 73 patients, 15 (20.5%) required replacement surgery during follow-up, mostly due to mechanical issues. Among the 73 women interviewed, 23 (31.5%) reported not regularly inflating and deflating the PP. The remaining 50 partners were asked to rate the challenge of managing the PP using a Likert scale, with an average score of 1.3 (very easy) out of 6 (SD = 1.4).
The average scores for each question in the EDITS questionnaire were 3.3 (SD = 0.9), 3.19 (SD = 0.9), 2.42 (SD = 0.8), 3.45 (SD = 0.9), and 3.67 (SD = 0.8) out of 4, respectively, with an overall average satisfaction of 80 (SD = 12.4) out of 100.
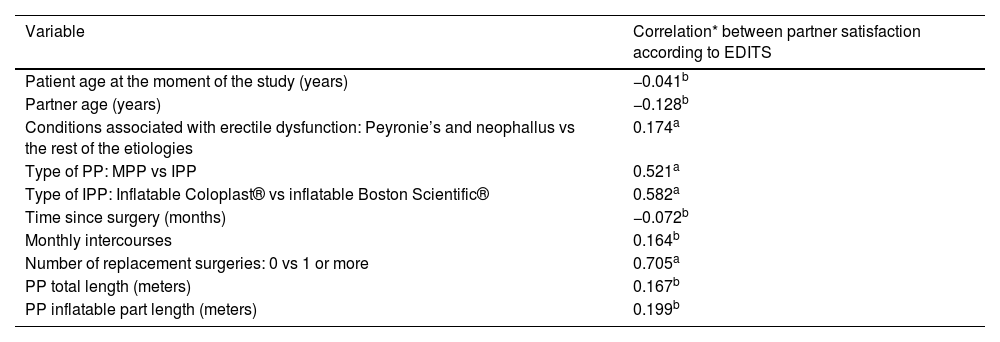
The relationship between various variables and sexual satisfaction in female partners is presented in Table 2. There was no correlation between the age of the female partner and sexual satisfaction according to the EDITS questionnaire (r = −0.128). Similarly, no correlation was observed with the current age of the patient (r = −0.041), time since surgery (r = −0.072) or number of monthly sexual intercourses (r = 0.164). Grouping different causes of ED, no significant relationship with sexual satisfaction was found (p = 0.174). There were also no differences in sexual satisfaction between IPP and MPP (p = 0.521) or among different brands of IPP (p = 0.582). The number of PP replacements did not influence sexual satisfaction (p = 0.705). Finally, there were no statistically significant correlations between the total length of the PP (r = 0.167) or the length of the inflatable part (r = 0.199) and sexual satisfaction.
Studied variables and their relationship with female partner sexual satisfaction.
| Variable | Correlation* between partner satisfaction according to EDITS |
|---|---|
| Patient age at the moment of the study (years) | −0.041b |
| Partner age (years) | −0.128b |
| Conditions associated with erectile dysfunction: Peyronie’s and neophallus vs the rest of the etiologies | 0.174a |
| Type of PP: MPP vs IPP | 0.521a |
| Type of IPP: Inflatable Coloplast® vs inflatable Boston Scientific® | 0.582a |
| Time since surgery (months) | −0.072b |
| Monthly intercourses | 0.164b |
| Number of replacement surgeries: 0 vs 1 or more | 0.705a |
| PP total length (meters) | 0.167b |
| PP inflatable part length (meters) | 0.199b |
EDITS: Erectile Dysfunction Inventory of Treatment Satisfaction; PP: penile prosthesis. IPP: inflatable penile prosthesis. MPP: malleable penile prosthesis.
Our original study involved 73 women whose partners underwent a PP implantation, and they were interviewed using the 5-item Partner EDITS questionnaire. This is a relatively understudied area within prosthetic urology, often characterized by the evaluation of small, heterogeneously studied couples.
Historically, various methods have been employed to evaluate partner satisfaction after PP surgery: single questions,7,10,12,14,16 unspecified questionnaires or researcher-designed surveys8,11,13,17,18 and validated instruments.6,9,15,17,19–23 Among these latter, the most commonly used include the Female Sexual Function Index (FSFI),15,19,23 the EDITS questionnaire (5-item Partner EDITS),6 and its modified versions,20–22 and the Arizona Sexual Experiences Scale (ASEX).21 However, these instruments may not accurately capture the experiences of patients undergoing PP surgery and their partners due to the lack6 of specific validation for this population. In our study, we opted for the Partner EDITS questionnaire because it is widely utilized in this context.27 It focuses specifically on satisfaction with ED treatment, is brief, easy to comprehend and respond to, and centers on the patient's partner. We believe it can be adapted effectively for our objectives compared to other questionnaires.
Out of all couples, 50 (68.4%) have manually operated (inflated and deflated) the IPP at least once, though not regularly, a finding consistent with other studies.10 Despite irregular use, those who did handle the IPP did not find it particularly challenging. We advocate for involving the sexual partner in both the decision-making process and the ongoing use of the PP to normalize its usage and enhance satisfaction.
In our study, partners scored near 4 (indicating high satisfaction) on the 5-item Partner EDITS questionnaire, with an overall EDITS score of 80 out of 100, consistent with satisfaction levels reported in the literature. For example, Özbay et al.,21,22 in their original papers evaluating partner satisfaction after PP surgery, obtained satisfaction scores of 78 and 86.7 using a modified EDITS questionnaire, similar to the findings of Çayan et al.,20 who reported high satisfaction in over 70% of partners. Similarly, Vakalopoulos et al.,6 reported a satisfaction rating of 70 ± 22 using the EDITS questionnaire.
Sexual satisfaction among female partners of patients with PD and refractory ED was high, with no statistically significant differences observed compared to other etiologies of ED. Usta et al.,14 reported 72% and 80% satisfaction rates among female partners following PP placement with subsequent correction of residual curvature in PD patients.
While our study did not demonstrate any predictors of couple satisfaction, it contributes to the body of research attempting to correlate various factors with female satisfaction, particularly focusing on different characteristics of PP.
We did not find statistically significant differences in female sexual satisfaction based on the type of PP (IPP vs. MPP) or the brand of IPP used. Çayan et al.,20 using a modified EDITS questionnaire in 883 couples, noted significantly higher couple satisfaction rates in the IPP group compared to the MPP group, but found no differences in satisfaction based on brands of three-piece implants. Similar to Beutler et al.,9 who found that the 49 partners of patients receiving IPP were significantly more satisfied than those receiving MPP, based on a researcher-designed questionnaire. Romero Otero et al.,18 identified a significant difference in couple satisfaction between two IPP models (700CX™ and Titan) using a non-validated two-item questionnaire in 209 female partners. Montorsi et al.13 did not find any statistically significant correlation between different types of IPP (Ultrex®, Ultrex Plus®, CX®, CX Plus®, CXM®) and female satisfaction.
In our analysis, no relationship was found between female sexual satisfaction and variables such as female and patient age, time since surgery, number of sexual intercourses, conditions associated with ED, number of replacements, total length of the PP or its inflatable part. Similarly, Çayan et al.,20 reported no significant differences in female sexual satisfaction based on patient age, partner age or various causes of ED. Additionally, some research has shown positive correlations between female sexual satisfaction and the duration of the partner relationship17 and marital status,6 as well as an inverse correlation between female age and satisfaction.19 Furthermore, significant relationships have been demonstrated between female sexual satisfaction and patient satisfaction with the PP.6,17
Study limitationsThis retrospective cohort study is subject to several typical limitations. Being conducted at a single center limits the generalizability of the findings to broader populations. Furthermore, the evaluation of satisfaction was limited to heterosexual couples. The study lacked data on women's sexual satisfaction before PP surgery, preventing the observation of changes post-procedure. Similarly, patient satisfaction with the PP was not assessed, precluding analysis of potential correlations between patient and partner satisfaction. Additionally, the limited number of couples in our study may restrict our ability to observe statistically significant differences. Increasing the study population could enhance our statistical power.
Moreover, the EDITS questionnaire used to assess partner satisfaction after PP surgery has not been specifically validated for this purpose, nor is it validated in Spanish, the native language of the interviewed sexual partners.
ConclusionsAlthough sexual satisfaction among female partners of patients undergoing PP implantation in our cohort is high, no statistically significant differences were found in couple satisfaction based on variables such as time since surgery, type of PP, brands of IPP, total length of the PP, or length of the inflatable part. Further studies involving a larger number of patients and female partners are needed to validate these findings.
The development of new, validated questionnaires in various languages specifically designed to assess female satisfaction in couples where a PP is present is essential to draw definitive conclusions and improve understanding in this field.
Ethical approvalThe study was conducted in accordance with Good Clinical Practice (GCP) guidelines as defined by the International Council for Harmonization (ICH/135/95) and adheres to the provisions of the Declaration of Helsinki (as revised in Fortaleza, Brazil, October 2013). The study complied with local regulations and operational procedures for clinical investigations and documentation management. Additionally, the study was carried out in compliance with Spanish regulations, specifically the Biomedical Research Law of July 3, 2007 (BOE n 159).
Ethical approval of studies: not applicable. The research was a retrospective study and it does not affect the patient management. However, patients and partners were asked if they were willing to collaborate in the study and they gave a verbal consent. All participants signed written consent prior to PP surgery.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
PP: penile prosthesis. EDITS: Erectile Dysfunction Inventory of Treatment Satisfaction.