Our objective was to elaborate a predictive model of bladder cancer, in an unselected clinical population submitted to cystoscopy.
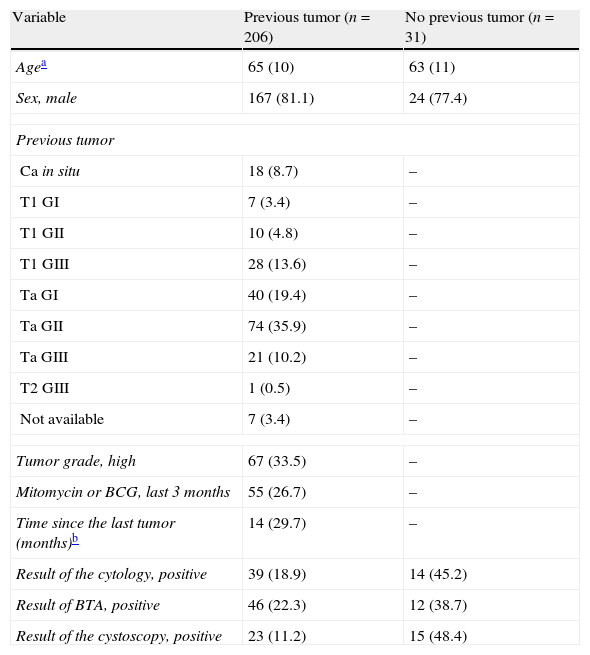
Materials and methodsWe recruited consecutive patients who underwent cystoscopy due to suspicion of bladder cancer or surveillance of a previously diagnosed bladder cancer. Urine cytology and a BTA-stat® (BTA) test were carried out for all patients. To avoid an assessment bias, the BTA-tests, cytologies and cystoscopies were conducted in a blinded fashion. We used logistic regression to predict cystoscopy results from cytology, BTA-test and clinical variables.
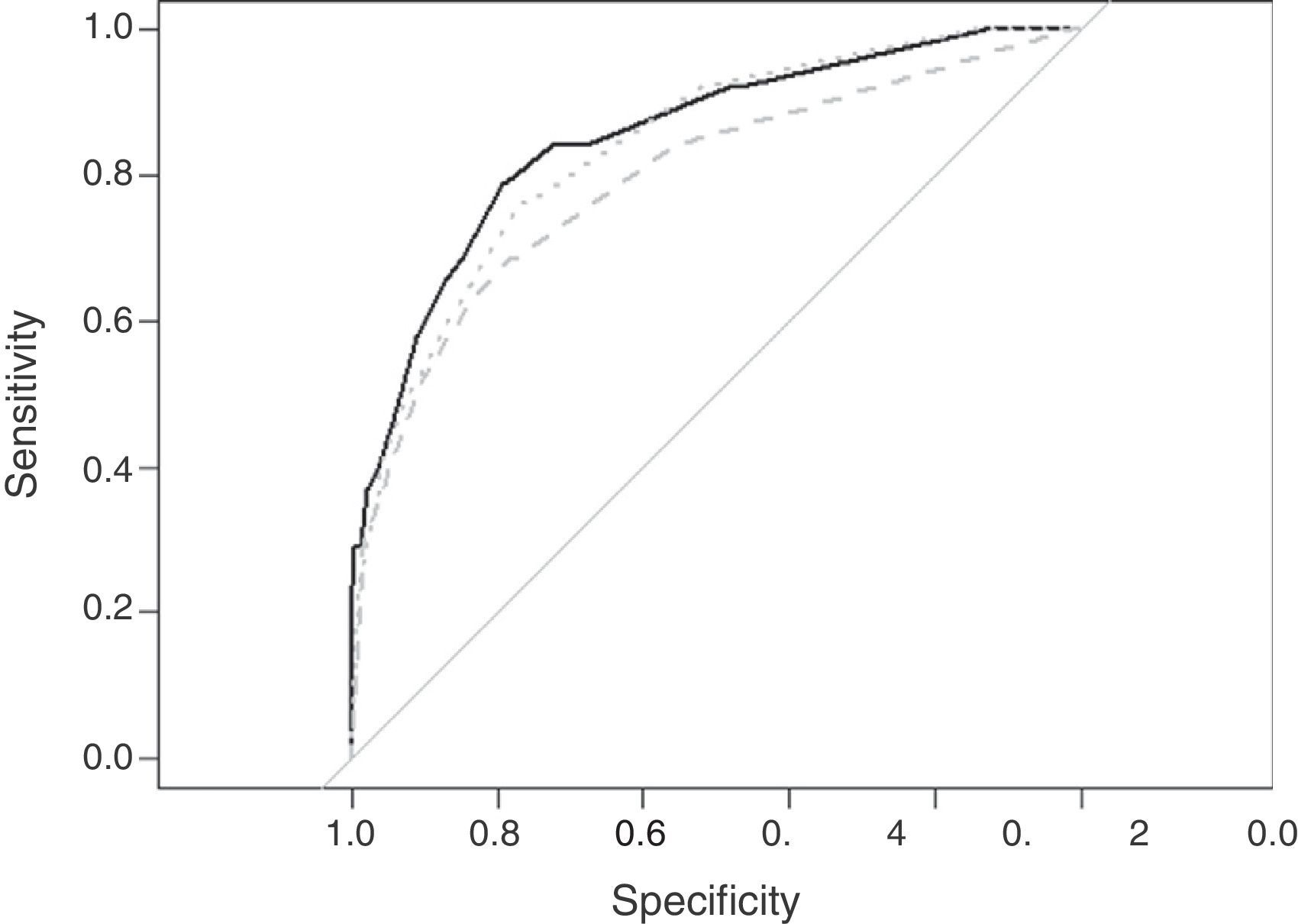
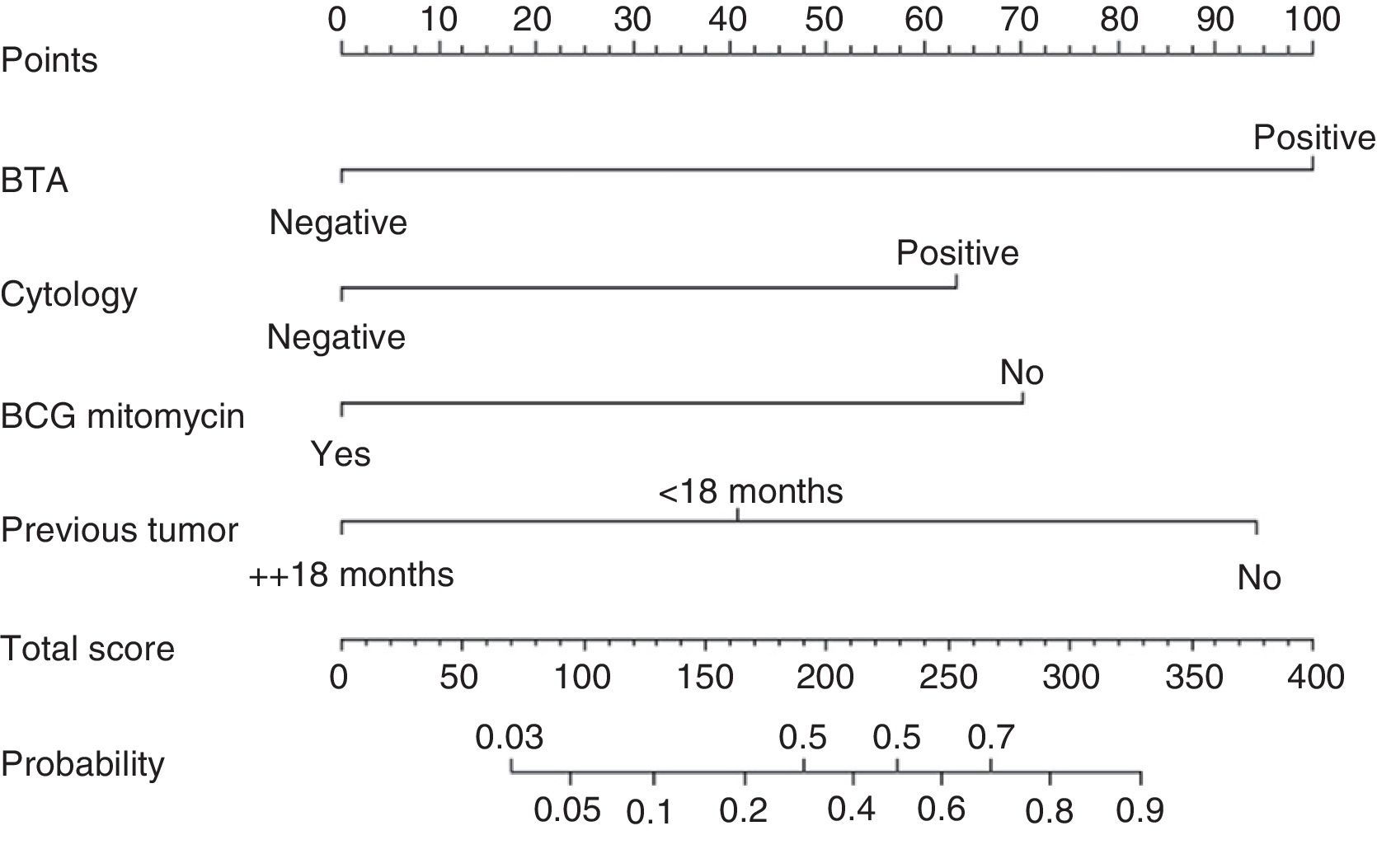
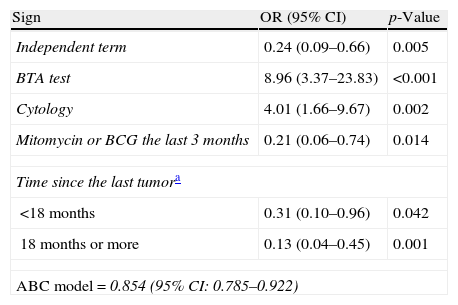
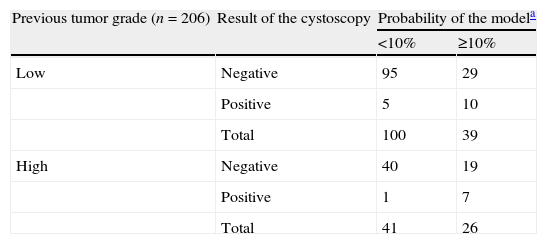
ResultsFrom August 2011 to July 2012, we recruited 244 patients and 237 were valid for analysis. Newly diagnosed and surveillance cases were 13% and 87% respectively. Cytology and BTA-test sensitivities were 57.9% (CI 95: 42.2–72.1) and 63.2% (CI 95: 47.3–76.6) with specificities of 84.4% (CI 95: 78.7–88.8) and 82.9% (CI 95: 77.1–87.5). The predictive model included the BTA-test, cytology, time since previous tumor, and treatment with mitomicin or BGC during the last three months. The model predictive accuracy (AUC) was 0.85 (0.78–0.92), and dropped to 0.79 when excluding the BTA-test (p=0.026). For the surveillance of bladder cancer, a 10% threshold on the model predicted probabilities resulted in an overall negative predictive value of 95.7%, and 95.0% in low grade tumors.
ConclusionIn a cost containment environment, our prediction model could be used to space out cystoscopies in patients with previous, low grade tumors, resulting in a more efficient use of resources in the healthcare system.
Elaborar un modelo predictivo de cáncer de vejiga en una población clínica no seleccionada derivada a cistoscopia.
Materiales y métodosPacientes consecutivos sometidos a cistoscopia debida a sospecha o seguimiento de un cáncer de vejiga previamente diagnosticado. Todos los pacientes fueron sometidos a citología urinaria y un BTA-stat®-test (BTA). Para evitar sesgos de evaluación, BTA, citologías y cistoscopias fueron realizados de forma ciega. Usamos regresión logística para predecir los resultados de la cistoscopia a partir de citología, BTA y variables clínicas.
ResultadosEntre agosto de 2011 y julio de 2012 seleccionamos 244 pacientes y 237 fueron válidos para el análisis. Un 13% fueron de nuevo diagnóstico y un 87% de seguimiento. Las sensibilidades de la citología y el BTA fueron 57,9% (IC 95%: 42,2–72,1) y 63,2% (IC 95%: 47,3–76,6) con especificidades de 84,4% (IC 95%: 78,7– 88,8) y 82,9% (IC 95%: 77,1–87,5). El modelo predictivo incluyó BTA, citología, tiempo transcurrido desde el diagnóstico del tumor previo y tratamiento con mitomicina o BGC en los últimos 3 meses. La precisión del modelo (AUC) fue 0,85 (0,78–0,92), y bajó a 0,79 al excluir el BTA (p=0,026). En los casos de seguimiento, un umbral de 10% en las probabilidades predichas por el modelo resultó en un valor predictivo negativo de 95,7%, y 95,0% en los tumores de bajo grado.
ConclusiónEn un contexto de contención de costes nuestro modelo puede usarse para espaciar las cistoscopias en pacientes con tumores de bajo grado previos, resultando en un uso más eficiente de recursos del sistema de salud.