Wheezing constitutes a common respiratory symptom in children, and several risk factors have been associated with the prevalence of recurrent wheezing (RW) and its severity, especially viral respiratory infections and second-hand smoke (SHS) exposure.
ObjectiveTo analyze the relationship between smoking patterns in the home and wheezing, in infants from the city of Córdoba, Argentina, during their first year of life.
MethodsParents of infants were invited to complete a standardized questionnaire voluntarily and anonymously (WQ-P1-EISL). Wheezing in the first 12 months of life was classified as occasional wheezing (OW) when having one or two episodes during the first 12 months of life; recurrent wheezing (RW) if having three or more, and more frequent wheezing (MFW) ≥6 episodes.
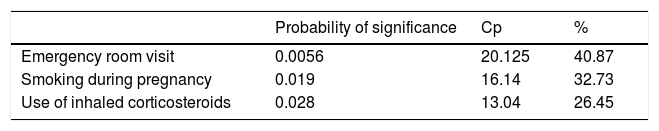
Results409 infants (39.0%) had one or more episodes of wheezing in the first 12 months. Of these, 214 infants (52.3%) presented occasional wheezing (OW), 135 (33%) had recurrent wheezing (RW), and 60 (14.7%) more frequent wheezing (MFW). SHS was significantly related to MFW, especially if the mother smoked (OR=2.7; IC 95%: 1.4–5.18; p=0.0009) or if she smoked during pregnancy (OR=4; IC 95%: 1.8–8.5; p=0.0001). This group of MFW was also associated with SHS as well as having been to the emergency room for wheezing (40.87%, p=0.0056).
ConclusionThe results indicate that second-hand tobacco smoke is a significant risk factor for the presence of wheezing in infants, and for its severity. Our findings have significant implications for public health, as smoking is a modifiable behavior.
Passive exposure to tobacco smoke is common, and its damaging effects on health have been well known for decades.1 However, the magnitude of the problem worldwide is poorly described.
Wheezing constitutes a common respiratory symptom in children; it has a number of causes and responds to different conditions in the lower respiratory tract. Wheezing has a significant impact on the quality of life of affected children and their families; it produces a significant increase in the use of health resources, regardless of the cause, and has high economic and social costs, especially recurrent episodes. It is called recurrent wheezing (RW) when three or more episodes occur during twelve consecutive months; it is a frequent cause of pediatric consultation and an important challenge for public health globally. In most cases, the initial events occur in the first year of life.2
Several risk factors have been associated with the prevalence of RW and its severity, especially viral respiratory infections. It has been reported that in Latin America around 100,000 infants died from acute respiratory infections in their first year of life (2008–2010), with a significant proportion of them having a history of recurrent wheezing.3 On the other hand, another study has estimated that 603,000 deaths were attributable to SHS in the year 2004, representing 1% of world mortality, of which 28% occurred in children.4
A growing body of literature has highlighted the importance of prenatal factors on the subsequent development of RW and asthma. In particular, in utero tobacco smoke exposure has been well established as promoting respiratory morbidity. In utero exposure to tobacco smoke remains a public health concern, as 13.2% of mothers in the United States were noted to smoke during pregnancy in 2006.5 Antenatal maternal smoking has been associated with the subsequent development of wheezing in childhood6,7; in utero cigarette smoke-induced transgenerational inheritance of disease risk8; and it is also a risk factor for subsequent development of COPD.9
The effect of Second-hand Smoke (SHS) on respiratory health has been of interest for many years. In the US Surgeon General’s report of 2006,10 the authors examined the effect of passive smoking on asthma and wheezing in children and found that if either parent smoked, the risk of asthma in childhood increased by around 40%. Whereas postnatal maternal smoking increased the incidence of wheezing, before the age of six by 30%, and during school-age years by 13%. This group concluded that the evidence is sufficient to infer a causal relationship between SHS exposure from parental smoking and the onset of wheezing illnesses in early childhood and is suggestive but not sufficient to infer a causal relationship between secondhand smoke exposure from parental smoking and the onset of childhood asthma. A recent systematic review and meta-analysis has quantified the strength of the associations,11 with data coming predominantly from developed countries.
Epidemiological studies contributed to the knowledge on the prevalence and risk factors of wheezing in three age groups younger than 12 months of age (EISL).12
The aim of the present study was to analyze the relationship between smoking in the home and wheezing, in one-year-old infants from the city of Córdoba, Argentina.
Material and methodsSubjects and samplingThe standardized written questionnaire (WQ-P1-EISL)13 was administered consecutively to the parents or guardians of infants who attended vaccination centers for routine immunization (National Vaccination Schedule), and who agreed to complete the questionnaire, between August 1, 2013 and March 31, 2014. Infants aged between 12 and 18 months old living in the city of Córdoba, Argentina were selected. In order to be representative from different socioeconomic strata and all regions of the city, the three largest public vaccinations centers (located in the southwest, southeast and north of the city) and two private vaccination centers were selected.
Wheezing was defined as an affirmative response to the question, “Has your child had wheezing or wheezed during the first 12 months of his/her life?” and this question had been previously validated in another study.12
We classified wheezing as occasional wheezing (OW), defined as having one or two episodes of wheezing reported by the parents during the first 12 months of life; recurrent wheezing (RW) was defined as three or more, and more frequent wheezing (MFW) more than six episodes.
Parental smoking was classified, based on the responses in the questionnaire, into four mutually exclusive categories: 1) no smoking parent; 2) only the mother smokes; 3) mother smoked during pregnancy; and 4) other smokers in the home. In this cross-sectional study, we searched for the condition at the time of the questionnaire and background.
The Clinical Research Ethics Committee of Córdoba, of the Ministry of Health of the Government of the Province of Cordoba, approved the study.
Statistical analysisData obtained with the WQ-P1-EISL were coded in Epi-InfoTM version 7 sheets and statistically analyzed with SPSS version 17.5 software in Spanish. Parametric tests (one-way ANOVA) and linear regression were applied.
All significant variables were selected and evaluated by multiple regression with Backward SAS, NAC. Level of significance was set at ≤0.05 p value. Odds Ratio used a two-by-two table in order to evaluate risk or protective factors.
We used wheezing in the last 12 months and more frequent wheezing as dependent variables, and as independent variables: frequent nocturnal awakening, use of inhaled corticosteroids, smoking during pregnancy, smoking mother, visit to the emergency room, first episode of wheezing <3 months of life, smoking at home, male gender, mother's education >12 years.
ResultsDuring the mentioned period, 1101 questionnaires were completed. From those, 69 reports corresponded to children living outside the region and were excluded; finally, 1062 questionnaires were analyzed, giving us a rejection rate of 29.2%. Mothers (99.1%) and fathers (0.3%) completed the questionnaires.
On the total sample of infants under one year of age, 409 children (39.0%) had one or more episodes of wheezing in the first 12 months and the average age of onset was 4.47±2.96 (r: 112 months). Of these, 214 children (52.3%) presented with OW, 135 (33%) had RW, and 60 (14.7%) had MFW.
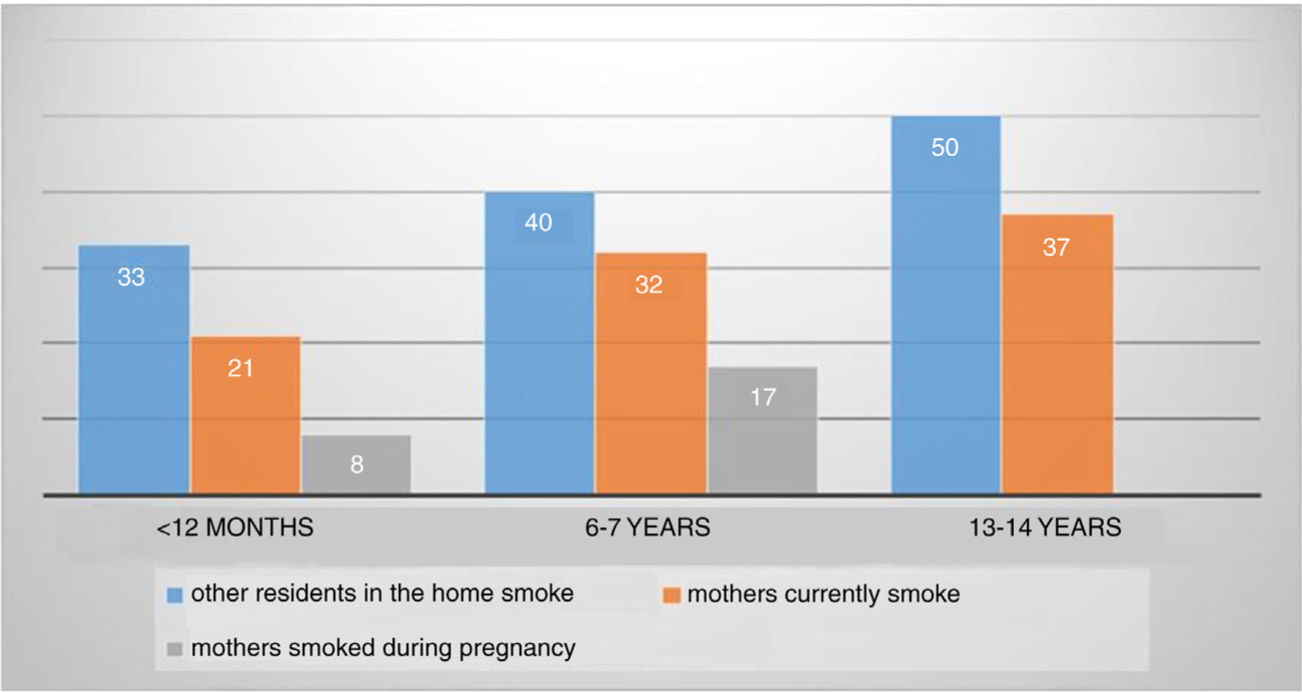
When evaluating smoking patterns in the home, we found that 8.4% of mothers smoked during pregnancy, 21.8% of mothers currently smoked, and 33.4% of other residents smoked.
Second-hand smoke notably influenced the presence of wheezing, particularly when the mother smoked (OR=2.7; IC 95%: 1.4–5.18; p=0.0009) and even worse during pregnancy (OR=4; IC 95%: 1.8–8.5; p=0.0001). Not only is a mother that smokes in the home harmful; the presence of other smoking inhabitants contributed to a higher risk of wheezing as well (OR=1.8; IC 95%: 1.01–3.4; p=0.002).
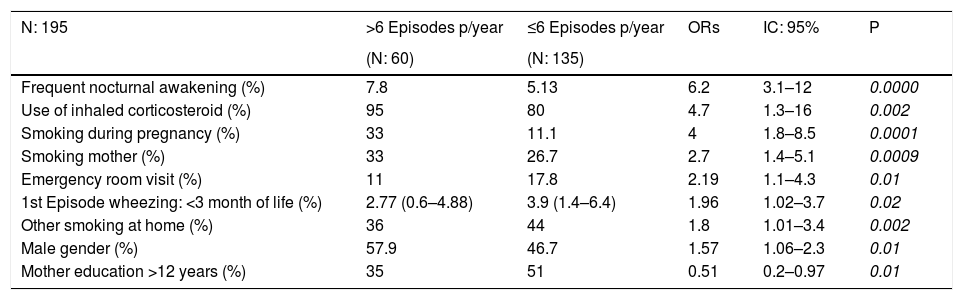
Some socio-economic patterns were found to decrease the risk of recurrent wheezing (RWMFW): working mothers (OR=0.59, 95% CI 0.39 to 0.91, p=0.007) and having an in-house toilet (OR=0.4, 95% CI 0.2 to 0.80, p=0.004), data found in our previous study.16 In the MFW subgroup we found that the educational level of mothers (university) (OR=0.51, 95% CI 0.17–0.97, p=0.01) was a protective factor for severity (Table 1).
More frequent wheezing: demographic and health characteristics (N: 195).
| N: 195 | >6 Episodes p/year | ≤6 Episodes p/year | ORs | IC: 95% | P |
|---|---|---|---|---|---|
| (N: 60) | (N: 135) | ||||
| Frequent nocturnal awakening (%) | 7.8 | 5.13 | 6.2 | 3.1–12 | 0.0000 |
| Use of inhaled corticosteroid (%) | 95 | 80 | 4.7 | 1.3–16 | 0.002 |
| Smoking during pregnancy (%) | 33 | 11.1 | 4 | 1.8–8.5 | 0.0001 |
| Smoking mother (%) | 33 | 26.7 | 2.7 | 1.4–5.1 | 0.0009 |
| Emergency room visit (%) | 11 | 17.8 | 2.19 | 1.1–4.3 | 0.01 |
| 1st Episode wheezing: <3 month of life (%) | 2.77 (0.6–4.88) | 3.9 (1.4–6.4) | 1.96 | 1.02–3.7 | 0.02 |
| Other smoking at home (%) | 36 | 44 | 1.8 | 1.01–3.4 | 0.002 |
| Male gender (%) | 57.9 | 46.7 | 1.57 | 1.06–2.3 | 0.01 |
| Mother education >12 years (%) | 35 | 51 | 0.51 | 0.2–0.97 | 0.01 |
In private centers, 76.8% of the reported patients had working mothers but in public hospitals, only 32% had working mothers. Working was significantly associated with less current smoking pattern (OR: 0.71 95% CI: 0.52–0.96, p: 0.015); to having smoked less during pregnancy (OR: 0.52, 95% CI: 0.32–0.85, p: 0.03); and to have fewer smokers at home (OR: 0.42, 95% CI: 0.32–0.56, p: 0.0000).
Accordingly, the highest level of education was found in mothers attending the private institutions (89.8% vs. 37%). Again, educational level was a protective factor for current smoking (OR: 0.72, 95% CI: 0.53–0.97, p: 0.01); for having smoked during pregnancy (OR: 0.46, 95% CI: 0.29–0.76, p: 0.0005); and for having other smokers in the home (OR: 0.57, 95% CI: 0.44–0.77, p: <0.0001). Having a toilet inside the home (as a proxy of poverty) was not statistically different between parents attending the public and private centers (91.6% vs. 98%).
DiscussionExposure to second-hand smoke is still one of the most common indoor pollutants worldwide. On the basis of the proportions of SHS exposure, at least 40% of children, 35% of non-smoking women, and 33% of non-smoking men are regularly exposed to SHS indoors.4 It was estimated that 165,000 children younger than five years die every year from lower respiratory infections caused by exposure to SHS. Children’s exposure to SHS most likely happens in the home. The combination of infectious diseases and tobacco seems to be a deadly combination for children, and might hamper the efforts to reduce the mortality rate for those aged younger than five years, as sought by the WHO Millennium Development Goal.4
One weakness of epidemiological studies is the tendency towards under-reporting of smoking frequency of parents and caregivers of children with respiratory diseases, especially given the fact they are aware of the harmful effects of smoking.14 In our study, the report of smoking pattern was low but significant: other people smoke in the home 33.7%, smoking mother 21.8% and smoking during pregnancy 8.4%. Because the ISAAC Phase III study in 200315 used the same methodology as that of our study, we observed a significant decrease in the percentages of smokers in the home in the 6–7year age group years. In that group we found: 17% of mothers smoked during pregnancy; 32% of mothers currently smoke and 40% of other residents in the home smoke; and in the teenage group of ISAAC: 37% of mothers currently smoked and 50% of other residents in the home smoked (Graphic 1).
As a consequence of the prohibition of smoking in public places by law, a reduction in smoking inside the home is expected as well.16
Other studies have demonstrated that exposure to parental smoking continues to be high in this group (infants) (greater than 51% in both parents and other smokers in the home).17
Since in-utero smoking/nicotine exposure may inhibit the individual from attaining their maximum lung growth, they are more predisposed to premature pulmonary aging and the development of chronic obstructive pulmonary disease.18 And while maternal smoking during pregnancy plays a major role on adverse postnatal outcomes, it may cumulate negatively with smoking during lactation and with SHS exposure. There is overall consistency in the literature regarding the negative effects of fetal and postnatal exposure to parental tobacco smoking on several outcomes: preterm birth, fetal growth restriction, low birth weight, sudden infant death syndrome, neurodevelopmental and behavioral problems, obesity, hypertension, type 2 diabetes, impaired lung function, asthma and wheezing. While maternal smoking during pregnancy plays a major role in adverse postnatal outcomes, it may also cumulate negatively with smoking during lactation and with SHS exposure.19
In infants, there is an increased risk of having RW and MFW if the mother or another member of the family smoked during lactation. We would like to emphasize that if the mother smoked during pregnancy, the possibility of MFW increases (Table 2).
We also found that in MFW infants, there is a greater relationship with the use of inhaled corticosteroids and this was observed both in the simple analysis and in the multiple regression analysis. We speculate that it was due to the exacerbation of bronchospasm or the association with smoking during the pregnancy, as mentioned by several authors who found a greater resistance to medication in smokers20,21 (Table 2).
The magnitude of the association is greater for current smoking by mothers than fathers, which may be due to infants spending more time in the home with their mothers.
We also observed an association with socioeconomic level. Accordingly, it seems that working mothers (usually attending private centers) expose their children less to SHS.
The present study has some limitations. Due to its cross-sectional design, a causal relationship cannot be established between SHS and wheezing. In addition, the data came from a questionnaire, with no objective measurement of exposure to smoking.
This might lead to some misclassification, but is unlikely to result in any systematic bias. It is worth mentioning that the validity of questionnaires in the evaluation of smoking in epidemiological studies is widely contrasting. Several studies have shown a strong correlation between smokers evaluated by questionnaire and environmental nicotine levels.22,23
Even having had a potential limitation from almost a 30% of rejection rate, one of the present study’s strengths includes the large and representative sample size, and another of its advantages was the use of the EISL study questionnaire validated internationally and also validated in the city of Cordoba.
The aforementioned studies demonstrated the effect of tobacco on early life lung function, evaluating the interaction of those risk factors in lung growth and development, becoming important and affecting the later development of asthma symptoms. Although we could not reinforce these findings from our epidemiological studies of ISAAC in the 6–7years age group carried out in the city of Cordoba (2003), it was evident in the group of adolescents with a strong association between mothers smoking and diagnosis of asthma (OR=1.332, 95% CI: 1.003–1.681, p=0.018. Gomez et al. observed similar results in adolescents exposed passively and actively to tobacco, being more likely to have asthma symptoms.24
ConclusionThe results of the present study support the association of second-hand smoke with the presence of wheezing in infants and for its greater frequency.
Additionally, we would like to stress that smoking in the home has decreased in recent years, but is still significant, and there has been an increase in smoking among those of lower socioeconomic status.
Our findings have significant implications for public health policy, as smoking is a modifiable behavior, which increases the possibility of reducing its impact on the pediatric population. This information about the magnitude and distribution of the burden of disease caused by SHS is particularly pertinent to policy makers, because this harm is eminently preventable.
Conflict of interestThe authors have no conflict of interest to declare.
FundingThe study has been self-financed as part of first author PhD.
Ethical disclosuresProtection of human and animal subjects
The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of data
The authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consent
The authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.