Vitamin B12, as it is not biosynthesised without certain bacteria and algae must be taken with a diet. The most important natural source of vitamin B12 is animal products and deficiency of vitamin B12 most commonly appears as pernicious anaemia. However vitamin B12 deficiency is not only associated with pernicious anaemia but is also linked with neurological conditions. Therefore, patients with low serum concentrations of vitamin B12 are given vitamin B12 supplements at regular intervals.
Vitamin B12 deficiency is a common condition, although hypersensitivity reaction against vitamin B12 is rare. In this paper, vitamin B12 allergy developed in a patient who does not eat meat and a successful desensitisation procedure with cyanocobalamin is presented.
The 39-year-old vegetarian woman with vitamin B12 deficiency (pernicious anaemia) who was taking monthly injections of 10mg cyanocobalamin, referred to allergy clinic, and commonly presented with itchy, exanthematous skin rashes about 30min after the tenth dose. The physical examination revealed widely distributed urticarial plaques all of the skin. The patient had no history of allergic disease.
Skin prick tests (SPT) were performed with cyanocobalamin and a possible cross-reaction to the hydroxycobalamin (1mg/ml dilutions). Both Drug allergies and treatmethe preparations did not contain any dyes or preservatives. Histamine and saline were used as positive and negative controls, respectively. SPT were positive for both preparations: cyanocobalamin; wheal 4mm×5mm and flare 30mm×30mm, hydroxycobalamin; wheal 4mm×3mm and flare 20mm×30mm, histamine (positive control); wheal 3mm×3mm and flare 20mm×20mm. Any wheal and flare reaction were not induced by saline (negative control).
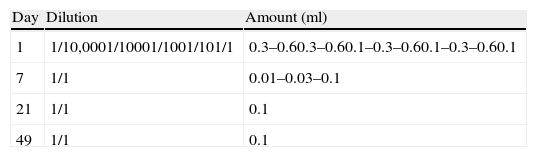
We desensitised the patient in our clinic as described in the literature1 (Table 1). After written consent was obtained, the desensitisation procedure began with 15-min intervals, and the desensitisation process started with increasing doses, one, two and four-week intervals, were similar to literature. The patient did not receive any premedication before the desensitisation procedure.
Desensitisation protocol with cyanocobalamin.1
| Day | Dilution | Amount (ml) |
| 1 | 1/10,0001/10001/1001/101/1 | 0.3–0.60.3–0.60.1–0.3–0.60.1–0.3–0.60.1 |
| 7 | 1/1 | 0.01–0.03–0.1 |
| 21 | 1/1 | 0.1 |
| 49 | 1/1 | 0.1 |
The desensitisation procedure was completed without any adverse events. At the end of the desensitisation procedure, SPT was performed with cyanocobalamin (1mg/ml) and resulted negative.
Drug allergies and treatment are the troublesome situations for the physicians in daily clinically practices. The patient who developed any adverse events after the drug treatment, the IgE-mediated allergic reactions should be confirmed with skin tests or specific IgE assays. Afterwards, desensitisation is performed in these cases if there are no suitable alternative drugs. Nowadays, desensitisation application is carried out successfully with antibiotics, aspirin, and even many different chemotherapeutic drugs.2–4
Unfortunately there is no standardised protocol for vitamin B12 desensitisation such as at antibiotics and aspirin. Therefore we used the same desensitisation protocol which Caballero et al. successfully applied in hydroxycobalamin and cyanocobalamin allergic patients are similar to our case1 (Table 1).
The desensitisation procedure should be started by the 1/100–1/1000 solutions of the drug target or the 1/10–1/1000 solutions of positive intradermal test dose and in increasing doses by doubling with 30–90min intervals until the therapeutic dose is achieved.5 Desensitisation must be carried out in a hospital setting by experienced personnel with adequate resuscitation equipment readily available.
It must be remembered that desensitisation is not always successful and the state of desensitisation is temporary. Therefore it is dependent on the continuous administration of the drug.
Vitamin B12 is the most chemically complex of all the vitamins, and cyanocobalamin and hydroxycobalamin are synthetically derived therapeutic forms of vitamin B12.6 Hydroxycobalamin protein binding capacity is greater than that of cyanocobalamin and both of them may cause allergic reactions.6 Vitamin B12 may lead to allergic reactions because of its cobalt molecule, molecular complexity or high molecular mass. The report of Olesen et al. suggested that treatment with exogenous B12 may cause the formation of immunogenic complex.7 Depending on the above-mentioned factors, cobalamin-IgG/M immune complexes may occur. However, there is no evidence for this hypothesis. Some factors, such as individual features or unknown molecules, may lead to antibody production against cobalamin, during the vitamin B12 replacement treatment.
Allergic reactions to cyanocobalamin or hydroxycobalamin are rare but a few case reports have been described.8,9 Our patients showed cross-sensitivity between cyanocobalamin and hydroxycobalamin with SPT; therefore, we had no substitute drug available.
The clinical pictures of vitamin B12 allergy caused by type 1 hypersensitivity that have been revealed with basophile histamine release test and skin prick tests as we have performed in our patient.10 We did not perform basophile histamine release test or specific IgE determination to indicate type 1 hypersensitivity reaction because of positive SPT results of both types of cobalamin preparation.
Due to the small number of cases in the literature there is no standard treatment regimen or desensitisation procedure for the vitamin B12 allergy yet. Therefore, we suggest that our case report may contribute to the formation of standardised desensitisation protocol in vitamin B12 allergy.
Conflict of interestThe authors have no conflict of interest to declare.