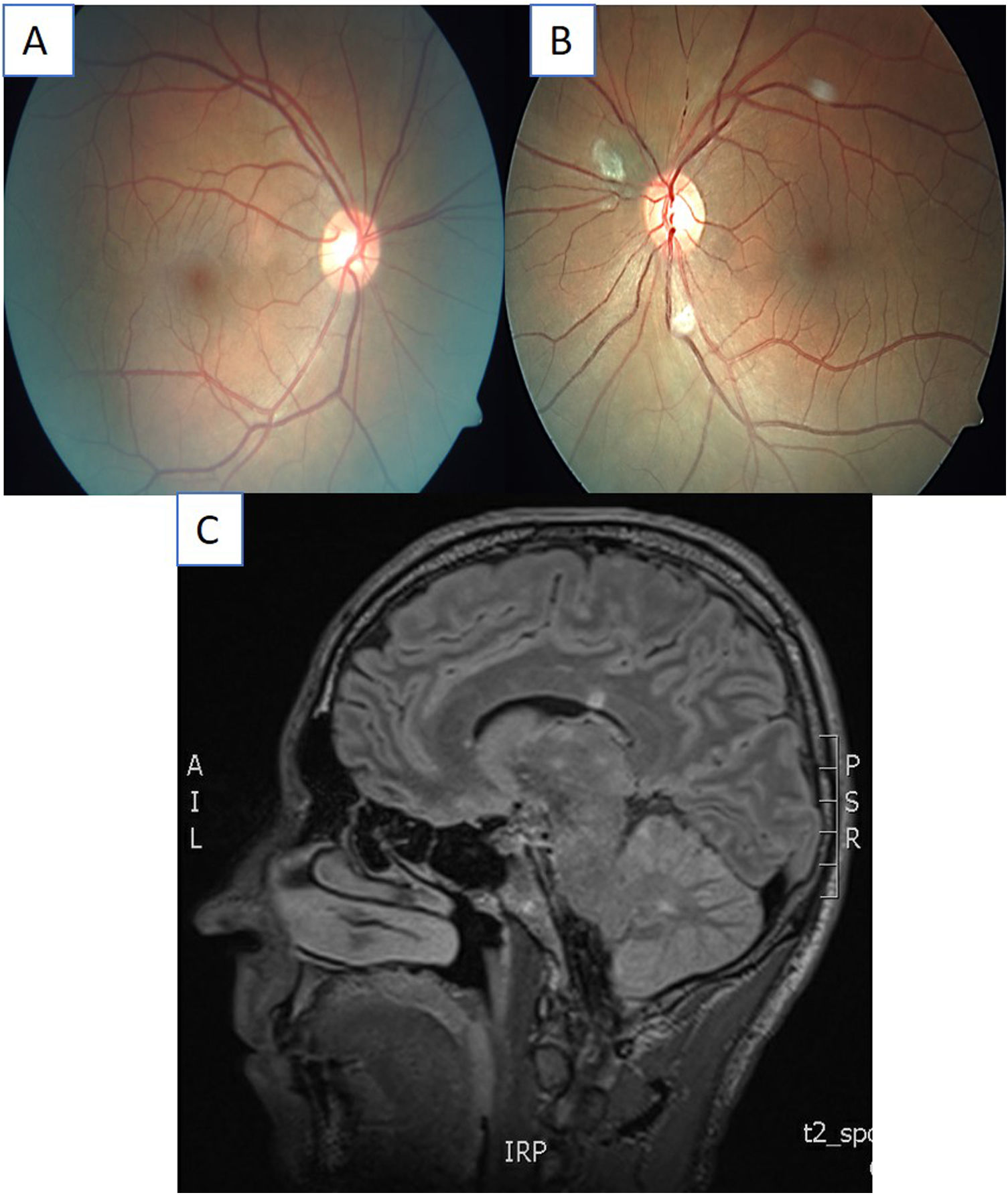
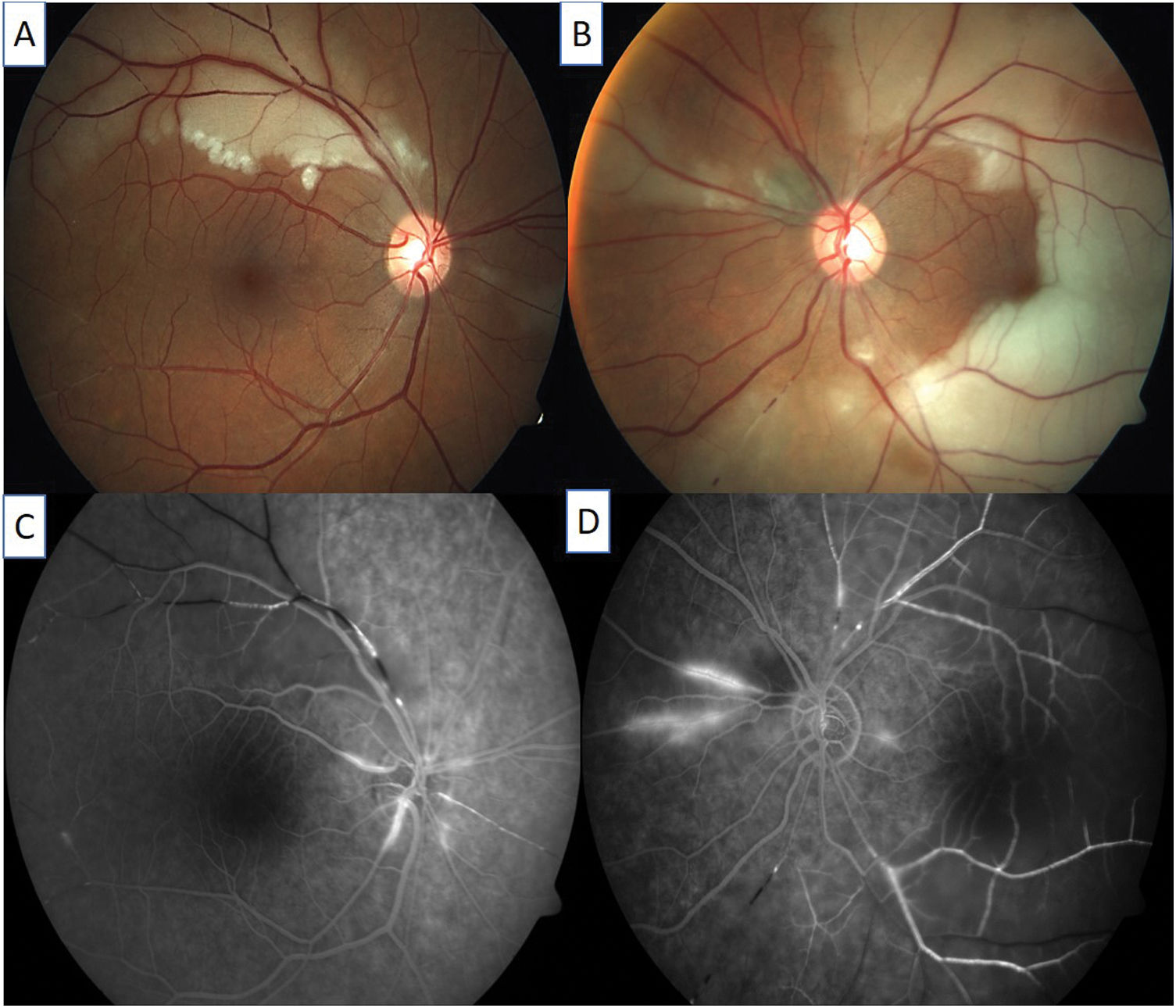
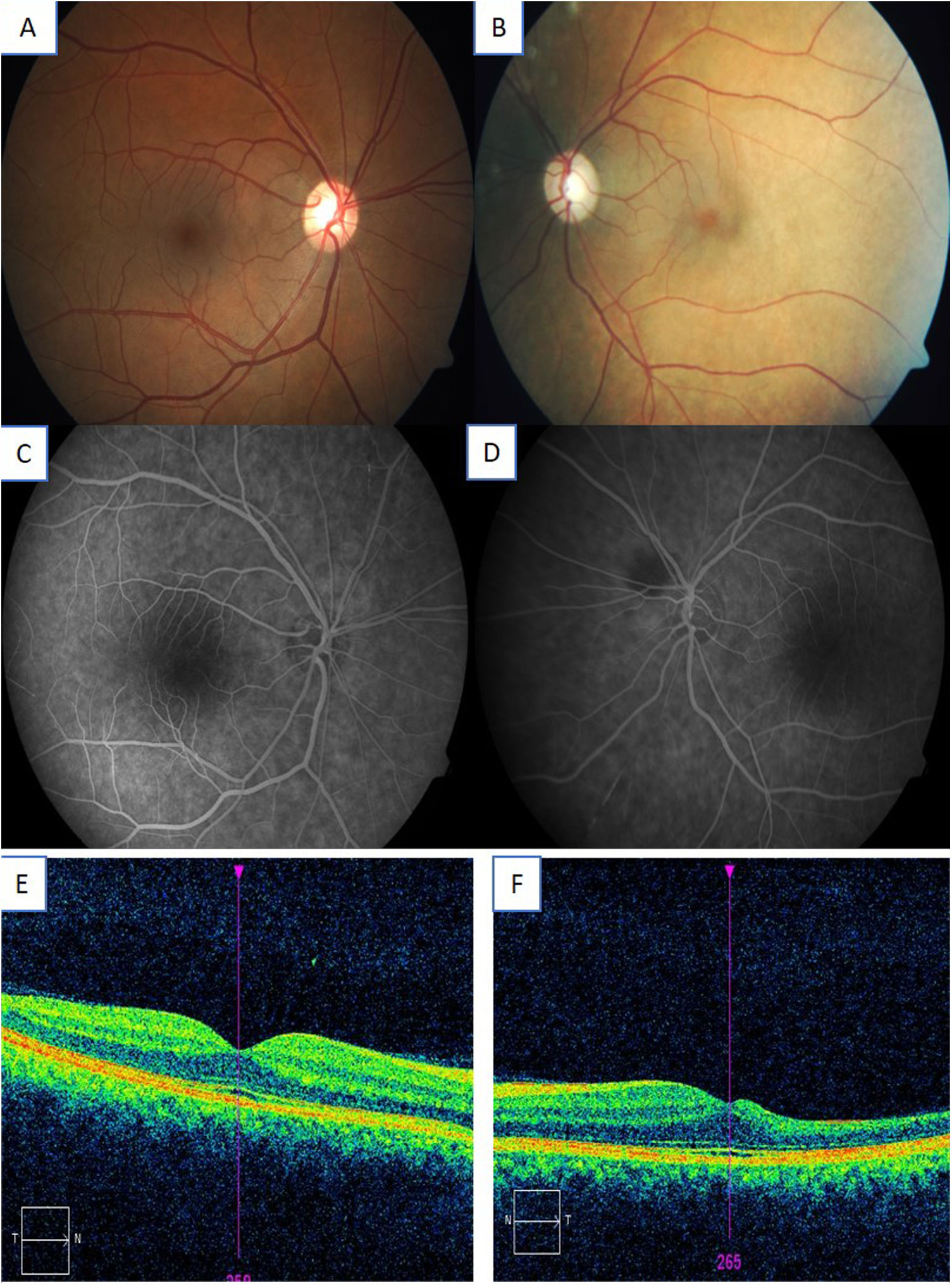
A 38-year-old man who attended the emergency department with headache, accompanied by vomiting, bradypsychia and gait instability, for which he was admitted to Neurology for study. During his admission, he began to present bilateral hearing loss and blurred vision in the left eye, with areas of arterial occlusion and hyperfluorescence of the arterial wall being observed in the ophthalmological examination. As a result, he was diagnosed with Susac syndrome.
He was treated with systemic corticosteroids, as well as with rituximab and subsequently, with intravenous immunoglobulins and mycophenolate mofetil.
The patient managed to preserve visual acuity, with gait instability and bilateral hearing loss as sequelae.
Early diagnosis of Susac syndrome is important, because a delay in the start of treatment can lead to irreversible sequelae such as deafness, blindness or neurological involvement.
Varón de 38 años que acude a urgencias con cefalea, acompañada de vómitos, bradipsiquia e inestabilidad de la marcha, por lo que ingresa en neurología para estudio. Durante el ingreso, comienza con hipoacusia bilateral y visión borrosa en el ojo izquierdo, apreciándose en la exploración oftalmológica áreas de oclusión arterial e hiperfluorescencia de la pared arterial, por lo que es diagnosticado de síndrome de Susac.
Se realiza tratamiento con corticoides sistémicos, así como con rituximab, y posteriormente con inmunoglobulinas intravenosas y micofenolato de mofetilo.
El paciente consigue preservar la agudeza visual y presenta como secuelas, inestabilidad de la marcha y pérdida de audición bilateral.
El diagnóstico precoz del síndrome de Susac es importante, porque un retraso en el inicio del tratamiento puede dar lugar a secuelas irreversibles como sordera, ceguera o afectación neurológica.