Seguridad del Paciente en Atencion Primaria
More infoPrimary care is an essential foundation for the global response to COVID-19 pandemic. It plays a significant role in the health care response: identifying and triaging potential COVID-19 cases, making an early diagnosis, helping vulnerable people cope with their anxiety about the virus, strengthening compliance with prevention and protection measures, and reducing the demand for hospital services. Primary care teams have continued to address citizens’ health problems during the pandemic, adapting to strict social control measures imposed by governments such as closing of borders, lockdowns and self-isolation of cases and contacts. We describe the COVID-19 response from primary care in Hong Kong and China, based on their recent pandemic experiences. We also present that of a European country, United Kingdom, less experienced in pandemic management, but with universal and highly developed primary care with great social recognition. Finally, we point out some crucial learning for future pandemic management, highlighting the crucial need to improve the relationship between primary care and public health to improve pandemics response.
La atención primaria es una parte esencial de los sistemas de salud para la respuesta global a la pandemia COVID-19. Desempeña un papel importante en la respuesta asistencial y en su control: identificando y clasificando los posibles casos de COVID-19, realizando un diagnóstico precoz, ayudando a las personas vulnerables a hacer frente a su ansiedad por el virus, reforzando el cumplimiento de las medidas de prevención y protección y reduciendo la demanda de servicios hospitalarios. Los equipos de atención primaria han continuado atendiendo los problemas de salud de los ciudadanos durante la pandemia, adaptándose a las estrictas medidas sociales de control impuestas por los gobiernos como el cierre de fronteras, el confinamiento de la sociedad, y el autoaislamiento de casos y contactos. En este artículo se describe la respuesta a la pandemia COVID-19 desde el nivel de atención primaria en Hong Kong y China, basada en sus experiencias de pandemias anteriores. También se describe la de Reino Unido, con menos experiencia en gestión de pandemias, pero con una atención primaria muy desarrollada, con una cobertura universal de la población y con gran reconocimiento social. Finalmente, se señalan algunos aprendizajes cruciales para la gestión de la pandemia en atención primaria de cara al futuro, entre ellas la importante necesidad de potenciar la relación entre atención primaria y salud pública.
One month after the first cluster of cases of unusual pneumonia was identified in China, the Director General of WHO declared a Public Health Emergency of International Concern (PHEIC) at the end of January 2020. By early March 2020 COVID-19 was declared as a pandemic.1
A pandemic is defined as “an epidemic occurring worldwide, or over a very wide area, crossing international boundaries and usually affecting a large number of people”.2
It is widely recognised that pandemics, like COVID-19, alongside an array of non-communicable diseases (NCDs) are disproportionately affecting those who are economically and socially disadvantaged.3 With family doctors and primary care teams (PCT) working in communities, dealing with these economic and social disparities, is business-as-usual, leaving primary care teams well placed to address both the early warning system and the early comprehensive response to the pandemic.
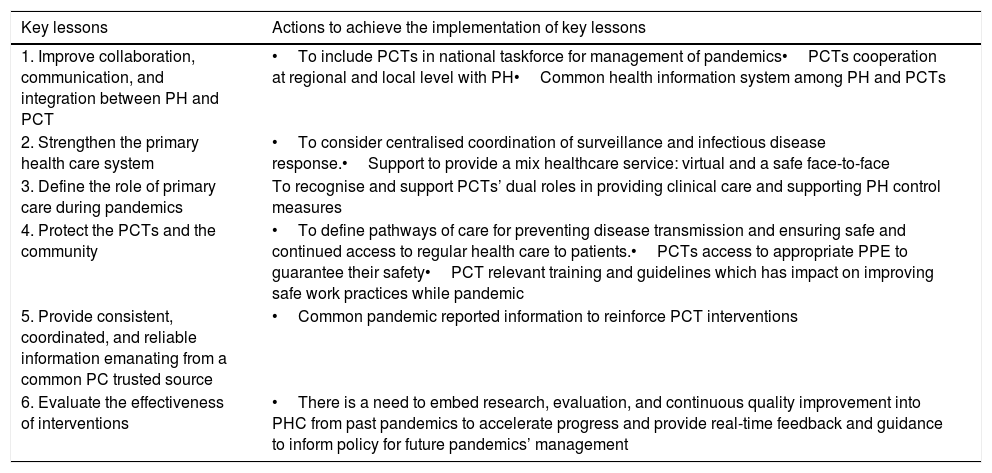
Past pandemics affected PCT and public health (PH) as well. A recent review summarised six main lessons from previous pandemics that should have been considered in the present COVID-19 pandemic4 (Table 1).
Six key lessons for the global primary care response. Actions to achieve the implementation of key lessons.
| Key lessons | Actions to achieve the implementation of key lessons |
|---|---|
| 1. Improve collaboration, communication, and integration between PH and PCT | •To include PCTs in national taskforce for management of pandemics•PCTs cooperation at regional and local level with PH•Common health information system among PH and PCTs |
| 2. Strengthen the primary health care system | •To consider centralised coordination of surveillance and infectious disease response.•Support to provide a mix healthcare service: virtual and a safe face-to-face |
| 3. Define the role of primary care during pandemics | To recognise and support PCTs’ dual roles in providing clinical care and supporting PH control measures |
| 4. Protect the PCTs and the community | •To define pathways of care for preventing disease transmission and ensuring safe and continued access to regular health care to patients.•PCTs access to appropriate PPE to guarantee their safety•PCT relevant training and guidelines which has impact on improving safe work practices while pandemic |
| 5. Provide consistent, coordinated, and reliable information emanating from a common PC trusted source | •Common pandemic reported information to reinforce PCT interventions |
| 6. Evaluate the effectiveness of interventions | •There is a need to embed research, evaluation, and continuous quality improvement into PHC from past pandemics to accelerate progress and provide real-time feedback and guidance to inform policy for future pandemics’ management |
PH: public health; PC: primary care; PCTs: primary care teams; PPE personal protective equipment.
Source: Adapted from Desborough J, Dykgraaf SH, Phillips C, Wright M, Maddox R, Davis S, Kidd M. Lessons for the global primary care response to COVID-19: a rapid review of evidence from past epidemics. Fam Pract 2021;cmaa142. doi:10.1093/fampra/cmaa142.
Some of them have been implemented in some countries and might be related to better results in managing the COVID-19 Pandemic.5
We describe two perspectives and experiences of dealing with the actual pandemic Hong Kong and China, and United Kingdom (UK).
Hong Kong and China and the bigger pictureIn the aftermath of the SARS outbreak in 2003 and the Ebola outbreak in 2013, one of the key lessons to take from each was the hugely negative impact of the pandemics in communities where strong community-based primary care systems were not in place. Family medicine is well established in Hong Kong. After the outbreak of SARS in 2003,6 the role of family doctors in Hong Kong in risk reduction and preparedness for medical emergencies quickly gained recognition,7 with Non-Government Organisations8 taking the lead in establishing community-based plans. Development of disaster preparedness plans and disaster risk reduction plans are now gaining traction in numerous communities and countries across the world.
The experiences of SARS and Ebola exposed the need for many countries to strengthen their primary care systems, including in China where, in 2016, a huge initiative was established to train primary care doctors and extend the availability of family medicine to the whole country by 2020.9 Despite huge strides in achieving the numbers, the goal has not yet been reached.
The global COVID-19 outbreak reinforced the need for comprehensive primary care being available, in recognition of the role played by family doctors as the first step in identifying and reducing health risks in China. Patients flocked to hospitals seeking testing and treatment, which quickly overwhelmed the system and helped to spread the virus. Having well-qualified family doctors based in communities builds trust which is impossible to replicate in hospitals and by secondary care clinicians.10 Family doctors working together with public health specialists and other professionals can ensure appropriate actions are taken.11
Developing community-based plans to detect and tackle health emergencies creates important co-operative and collaborative bonds between and across different professionals, which then are more effective should an emergency develop. In the absence of local government-organised community-based risk reduction strategies, the family doctor is well placed to take the initiative to establish such a strategy. Participation in development of community-based risk reduction strategies creates channels of communication to gather and share information quickly, to provide advice to patients and communities, and to establish trace and treatment arrangements. Working together, across professions and community groups, and having a plan in place, ensures that action can happen quickly to reduce risks for professionals and the communities in which they work, irrespective of the crisis they face.12 After SARS, the Hong Kong government adopted a clearly defined, tiered command structure to prepare for and respond to future outbreaks and consolidated all health protection functions under a new centralised agency.13 In parallel, massive investment has gone into research preparedness, with dialogue between the scientific and policy making communities in real time. Ever more stringent border restrictions have been adopted,14 and quarantine arrangements for both imported and local patients have improved.
Family doctors are frequently among the first responders to health emergency, and they have been keying across the world during the COVID-19 crisis. When the crisis subsides, eventually, through effective vaccination programmes and new treatment protocols, it is family doctors who are the clinical professionals left to manage the aftermath among their patients. The ‘first in, last out’ concept, as it relates to family medicine, holds true in this case.15 People in every country continue to live and present with ‘normal’ illnesses and diseases, which must also be evaluated, diagnosed and treated. In addition, the physical and mental health repercussions of a global pandemic live on in communities for many years, affecting successive generations, while successive generations of family doctors continue to provide care and treatment within those communities.
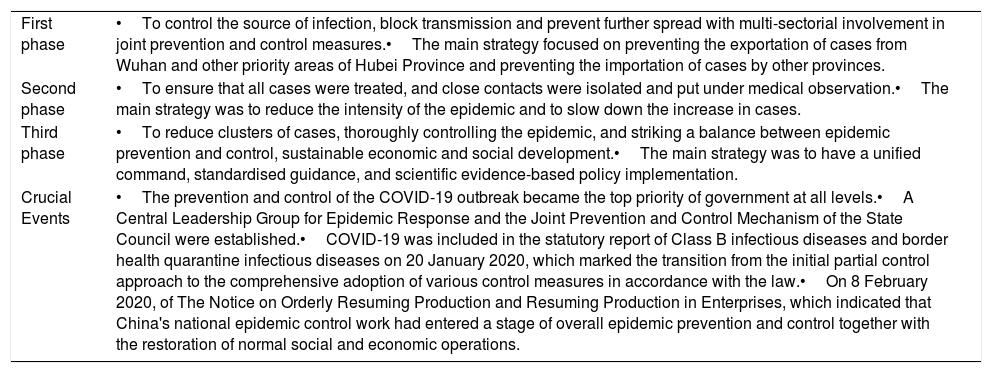
In China, as reported by the WHO-led Joint Mission in mid-February 2020,16 at the first recognition of the seriousness of the virus, a three-phase response was quickly established (Table 2). Phase 1 was to prevent cases spreading all over the nation, to control the source of infection, block transmission and prevent further spread. Phase 2 was to reduce the epidemic and slow the increase in cases, with all patients treated and close contacts isolated, while Phase 3 focussed on reducing clusters of cases, controlling the epidemic, and striking a balance between epidemic prevention and sustainable social and economic development. Family doctors had key roles to play throughout.
Three-phase response to COVID-19 in China, WHO-led Joint Mission report.
| First phase | •To control the source of infection, block transmission and prevent further spread with multi-sectorial involvement in joint prevention and control measures.•The main strategy focused on preventing the exportation of cases from Wuhan and other priority areas of Hubei Province and preventing the importation of cases by other provinces. |
| Second phase | •To ensure that all cases were treated, and close contacts were isolated and put under medical observation.•The main strategy was to reduce the intensity of the epidemic and to slow down the increase in cases. |
| Third phase | •To reduce clusters of cases, thoroughly controlling the epidemic, and striking a balance between epidemic prevention and control, sustainable economic and social development.•The main strategy was to have a unified command, standardised guidance, and scientific evidence-based policy implementation. |
| Crucial Events | •The prevention and control of the COVID-19 outbreak became the top priority of government at all levels.•A Central Leadership Group for Epidemic Response and the Joint Prevention and Control Mechanism of the State Council were established.•COVID-19 was included in the statutory report of Class B infectious diseases and border health quarantine infectious diseases on 20 January 2020, which marked the transition from the initial partial control approach to the comprehensive adoption of various control measures in accordance with the law.•On 8 February 2020, of The Notice on Orderly Resuming Production and Resuming Production in Enterprises, which indicated that China's national epidemic control work had entered a stage of overall epidemic prevention and control together with the restoration of normal social and economic operations. |
Source: SARS Expert Committee; 2003. Internet. Available from: https://www.sars-expertcom.gov.hk/english/reports/reports/reports_fullrpt.html [accessed 12.06.21].
Family doctors worked to conduct health checks, providing medical advice, referring patients for treatment where necessary, leading the efforts on contact tracing, treating patients both in communities and in hospitals, and providing care to discharged patients.
In addition to the personal hands-on approach adopted by family doctors in China, it was recognised early in the pandemic that use of information technology and artificial intelligence could be adapted to create health screening networks to assist with contact tracing and the investigation of sources of infection. Use of social messaging (WeChat) provided a speedy method of disseminating health messages and advice, particularly around use of masks, handwashing, avoidance of social gatherings and the importance of good ventilation.17 Social messaging was also used to provide counselling and support to the community, to allay fears and panic.
The use of online consultations between family doctors, primary care teams and patients became a necessary primary care delivery method across the globe during the worst of the pandemic. For some, online consultations will continue to be a feature of providing care after the pandemic subsides. Others are concerned at the loss of a key element of family medicine, the personal interaction and relationship between clinician and patient. Time and again, the importance of continuity of care is raised as a key factor in the efficacy of online consultations. China needs modernising its primary health-care system through the establishment of a learning health system built on digital data and innovative technologies.18 In recognition of the growing use of online consultations and the speedy development of platforms to host online consultations WONCA has taken the initiative to get involved in their development so that applications are specifically produced for family medicine. WONCA wants to define the standards, rather than letting standards be defined for others.19
The United Kingdom's responseThe U.K. had its first confirmed cases of COVID-19 in the last days of January 2020 but did not move to a full lockdown and border closure until almost two months later. Three other major issues were: uncertainty about the whole situation; lack of appropriate personal protective equipment, especially in social care settings; and provision of routine care under radically changed and rapidly moving circumstances.
What worked? The comprehensive coordinated service offered by the National Health Service (NHS)20 has highlighted its enormous value and efficiency during the pandemic. There was national guidance tailored to all four countries21 from public health leaders with really robust scientific training; data from both primary and secondary care were being uploaded and analysed every day; communications cascades could reach both clinical and administrative staff all over the country; and the health service acted as an organisational structure which could respond to public need, and to emergent problems.
The contribution of General Practitioners (GPs) and their teams also deserved wide praise because they stayed open throughout, adapting to the very different risks and doing much more online22; then, in the last months, leading the vaccination of the adult British population. GPs have been involved ‘from the top down’,21 leading researchers from primary care making major contributions to the evidence; an officer of our WONCA member organisation being a member of the Joint Committee on Vaccination and Immunisation; GPs in leadership positions in their locality helping to organise ‘safe’ clinics and vaccine hubs, and people coming back from retirement to work in practice.
However, government figures at the start of April 2021 showed that “There have been more than 4.3 million confirmed cases of coronavirus in the UK and nearly 130,000 people have died”. These figures include only people who have died within 28 days of testing positive for COVID-19 and other measures suggest the number of deaths is higher, with another government chart putting the deaths at above 150,000.23 Apart from these tragic losses, there are questions to be answered about the effectiveness of some of the contact test and trace schemes put in place. Private contracts for these (as well as personal protective equipment) appeared to have been issued in a rush, and to have been very expensive without being very effective. There were variations in national responses in each country in the UK, with different dates for lockdown, issues around supply chains for PPE and vaccines, and regional variations in contact tracing the impacts of these remain to be evaluated. However, overall, the U.K. fared badly compared to many other countries in Europe or indeed globally. Whether this was a consequence of being a crowded group of islands with significant reliance on dense housing and public transport, or whether it relates to more preventable factors remains to be seen. There is a current call for a full independent enquiry into this, though this is likely to be delayed until Parliament has time to do it justice.24
What have been the consequences? NHS data and our experience in community settings are showing massive psychological sequalae from the pandemic and lockdown, as well as significant ongoing physical morbidity for some of those who have contracted COVID-19. ‘Long COVID-19’25 is becoming a recognised condition needing long term rehabilitation and support. The U.K. is also now experiencing huge backlogs in planned hospital care, and increase of waiting lists26; also, a build-up of chronic disease checks27 and screening interventions in primary care.
The pandemic has seen the exacerbation of health inequalities for several reasons28 there is significant increase in unemployment, despite the interventions of government to support employers by providing furlough allowances (mandatory suspension supported financially by government). The people who were on low wages attempted, where possible, to continue to work, possibly offsetting risk against earnings and this includes many health and social care support staff.29 In addition, poverty is associated with earlier comorbidities, which turned out to predispose to COVID-19 related complications. We have also seen a significantly greater impact on people from ethnic minority backgrounds. Again, this may correlate with income and circumstances, as well as pre-existing risk factors, but it is a sad fact that some of our non-white communities have been much more impacted by COVID-19.
So, what are the challenges? The Royal College of General Practitioners (RCGP),30 which is the WONCA membership organisation for GPs in the U.K., had already identified workforce and workload sustainability as priorities, coupled with a continued focus on “relationship-based care”. The last of these is about the valuable role of GPs and their teams in integrating care round the patient and their needs and preferences. The new opportunities of digital technology have assisted safe practice during the pandemic, but the best use of these technologies is now also a major policy priority. We need to assess clinical accuracy and effectiveness with different ways of consulting. Another challenge is more effective population care and community level intervention. Not just to address smoking or air pollution or exercise, but also the emotional and personal costs of the pandemic. GPs need to work with local government, employers, and community resources to make sure we help meet these challenges before they end up with even more people needing mental health treatments. And finally, there is a need to advocate for better funding and less bureaucracy for the health service, especially for primary care.
There have been specific pieces of work to try to enable the GPs in training31 to overcome gaps in experience. For example, in England a recent statement by Health Education England headlined additional funding, flexibility and opportunity for trainees to compensate for lost clinical contact. The RCGP also had to move its entire clinical qualifying exam into an online model and allowed GPs to qualify as planned and to enter the UK workforce at a crucial time. The other challenge is our own wellbeing and that of colleagues; many Continuing Professional Development (CPD) resources have been created, and NHS Wellbeing Hubs32 have been set up across the country. Simply reminding people that they need and deserve a break can be valuable in itself at a time when people have worked continuously for many months in anxiety-provoking settings. And this is also something that can help us to help colleagues too.
To summarise, no one was prepared for the pandemic, but previous experiences and a strong health service, with devoted family doctors at the heart of it, has enabled great care to be given under very challenging and rapidly changing circumstances. National and local GP leadership through evidence, education, and advocacy has supported GPs and their teams to do the right thing wherever possible. Many have commented on the increased team spirit in primary care, and the gratitude of patients. But there is much to learn about the things that could have been done better across the system as a whole.
ConclusionsWe need to shorten the knowledge translation gap and ensure that the lessons from pandemics regarding the role of PC, such as COVID-19, are embedded in ongoing and future pandemic responses.
As we can see from the perspectives of both our contributors, management of a pandemic is a crucial element of a strong PC structure. PCT should be trained in both pandemic risk management and in supporting communities to face major risks. Our experiences show that training PCT needs to include some essential learnings: planning for rapid scaling-up of services in response to risks; preparing guidelines and tools within PC for timely diagnostic activities in the population, in social and health care residences; defining clearly how to guarantee the case isolation, contact cases quarantine and follow-up of mild to moderate cases; and, at the same time, providing continuing clinical support for patients presenting with the usual array of signs and symptoms. Building respectful, informed, relationships between primary and secondary care providers will ensure effective communication channels to convey unequivocal messages to citizens. Finally, the relationship between PC and PH needs a more comprehensive approach to allow for a speedy response to emerging issues. This is best done by using up to date accurate information, which is not currently routinely available from PC settings. The PC contribution during the pandemic has been immense: we now know what we can do to make our PC national responses even better.
Since the outset of the pandemic, each country, each region, adopted systems which best met the needs of their populations. Those with well-defined and well-disseminated disaster risk reduction programmes were thought to be able to respond quicker and, possibly, more effectively, in the earlier stages of their pandemic experiences. Those with close working relationships between PC and PH were able to respond quicker than others. We look forward to a time in the short-term future, where PC, PH and secondary care can work much more collaboratively, using information which reflects the realities of the different inputs made by all to improving and protecting the health of the world.
Conflict of interestThe authors declare that they have no conflict of interest