Introducción: La cetoacidosis diabética (CAD) es una de las complicaciones más graves de la diabetes mellitus (DM). El objetivo de este trabajo fue destacar la importancia clínica y de laboratorio en el tratamiento de pacientes con CAD, atendidos en el Hospital Infantil del Estado de Sonora (HIES) durante un periodo de 15 años.
Métodos: Se revisaron en forma retrospectiva 140 pacientes con episodios de CAD para informar el seguimiento clínico, de laboratorio y mortalidad con el Protocolo HIES.
Resultados: La mortalidad fue de 0%, y mediante estadística descriptiva se observaron mínimas complicaciones hidroelectrolíticas sin secuelas neurológicas en tres pacientes con edema cerebral.
Conclusiones: El Protocolo HIES es práctico y efectivo para el tratamiento hidroelectrolítico y ácido-base de la CAD con un mínimo de complicaciones.
Background: Diabetic ketoacidosis (DKA) is one of the major complications of diabetes mellitus (DM). The objective of this report was to highlight the clinical and laboratory importance in the treatment of patients with DKA during a 15-year period at the Hospital Infantil del Estado de Sonora (HIES).
Methods: We retrospectively reviewed 140 patients with episodes of DKA to report clinical and laboratory features, mortality, and treatment withthe HIES protocol.
Results: Mortality was 0%. Using descriptive statistics we observed minimal complications without neurologic sequelae in three patients with cerebral edema.
Conclusions: The HIES protocol is a practical and effective electrolyte and acid-base treatment for DKA.
1. Introduction
Diabetic ketoacidosis (DKA) is one of the most serious complications of diabetes mellitus (DM). It occurs more frequently in type 1 DM, which is the main acute cause of morbidity and mortality1 as a result of the insufficient relative or absolute insulin secretion.
There are different guidelines for the approach and treatment of DKA such as those published by Wolfsdorf2 where a systemized protocol for rehydration in 48 h is proposed and a mortality rate from 0.15-0.30% is mentioned. Other studies report a mortality from 4-18.2%.3 The Hospital Infantil del Estado de Sonora protocol (HIES protocol) recommends rehydration in 24 h and takes into account the additional losses of osmotic uresis and the imperceptible losses in Kussmaul respiration in the first 8 h. Reported mortality is zero. The present study is a cross-sectional study of 140 children treated using treatment guidelines (HIES protocol, currently in force) during a period of 15 years (Table 1).4 The goal of this work was to describe the clinical aspects and laboratory findings as well as the results in mortality and morbidity during the management of DKA in patients treated in the emergency service of the HIES.
2. Methods
Clinical files of minors 1–18 years of age who were admitted to the emergency service with diagnosis of DKA during the period from 2000–2014 were retrospectively analyzed. DKA was defined as the presence of hyperglycemia ≥300 mg/dl, metabolic acidosis pH <7.3, HCO3<15 and ketonemia with ketonuria>3 mmol/l.3 Of 210 cases, 140 were selected who met the criteria for DKA. They were treated with the permanent guideline “protocol HIES” for the approach and treatment of DKA (established since 2000).4 Ketoacidosis was classified by arterial blood gases according to the severity of the acidosis: mild (pH 7.30-7.25), moderate (pH 7.25-7.1) and severe (pH <7.1). Degree of dehydration was evaluated according to the estimated percentage of body water loss: 5%, 7% and 10%, respectively.5 The rest of the continuous variables such as age, gender, blood counts, serum electrolytes, glycemia, hospital stay, socioeconomic status, family history, pH values and precipitating factors were analyzed using descriptive statistics.
To study the correlation between the time (in years) with the well-known and newly detected cases in the HIES, the proportion of known cases is represented with the ratio between the known cases and the annual admissions to the emergency department. Thus, the proportion of new cases was represented with the ratio between the new cases and annual income. Cases expressed in terms of ratios were studied using regression analysis to corroborate the possible presence of linear or quadratic tendencies, calculating the p value for each model and coefficient of determination adjusted to study the correlation. Data were analyzed with the statistical software JMP/SAS 11.0PRO®.
3. Results
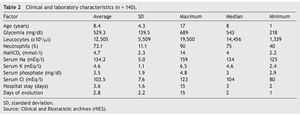
Of the 140 children, 73 were females (52%) and 67 males (48%). Average age was 8.4 ± 4.3 years with a maximum of 17 years and a minimum of 1 year. Glycemia was 529.3 ± 139.5 mg/dl, leukocytes 12,505 ± 5,509 x 103/μl, with a predominance of segments (73.1%). Sodium bicarbonate (NaHCO3) was 4.7 ± 2.3 mmol/l, serum sodium (Na) 134.2 ± 5 mEq/l, serum potassium (K) 4.6 ± 1.1 mEq/l, serum phosphorus 3.5 ± 1.9 mg/dl, serum chloride (Cl) 103.5 ± 7.6 mEq/l.
Hospital stay was 3.6 ± 1.6 days. Days of evolution of the clinical manifestations or DKA prior to hospitalization (abdominal pain, nausea, vomiting, polyuria, polydipsia, fatigue, and respiratory difficulty) was 2.8 ± 2.2 days, with a maximum of 15 days and a minimum of 1 day (Table 2).
With respect to the socioeconomic level and family history, the proportions were significant. Severity of the cases was distributed in the following manner: mild in 40 (29%), moderate in 61 (43%) and severe in 39 cases (28%). Precipitating factors were infections with 57 cases (41%); failure to give insulin in 46 cases (33%); and dietary indiscretion in 37 cases (26%). Known diabetic patients represented 49 cases (35%) and there were 91 newly diagnosed cases (65%) (Table 3). Proportion of admission of known cases of DM with DKA remained relatively stable during these 15 years. This was not so for the proportion of new cases of DKA, which has increased from 2008 to 2015 (Figure 1).
Figure 1 Patients newly diagnosed according to year. DKA: diabetic ketoacidosis. Source: Clinical and Biostatistic Archives (HIES).
Clinical and electrolyte complications on admission and during rehydration were totally present in 41 cases (29%): hypokalemia in 13 (9%), hyperkalemia in 4 (3%), hyperchloremic acidosis in 4 (3%), hyponatremia in 5 (4%) and hyper-natremia in 4 (3%). There was acute pulmonary edema in 4 cases (3%), refractory metabolic acidosis in 4 cases (3%) and cerebral edema in 3 (2%) (Table 4). Mortality was 0%.
4. Discussion
Currently, there are different protocols where there is agreement with other authors on fluid replacement in 24 h6,7 and avoidance of the routine use of bicarbonate (only in situations of severe acidosis pH ≤6.9). However, in contrast to the HIES protocol, in the electrolyte replacement no other additional losses are contemplated such as osmotic uresis and imperceptible losses (Kussmaul respiration), fundamental characteristics in the physiology of DKA. They should be taken into account as the free water losses by uresis could reach ranges from 100-150 ml/kg, and of sodium 70 mEq/l8, and the imperceptible losses of fluids in conditions of important polypnea such as Kussmaul respiration, figures from 0.5-1.5 ml/kg/h.9
On the other hand, initial management of insulin to infusion (0.1 U/kg/h) and avoidance of insulin boluses is agreed upon. This is considered unnecessary because of the risk of complications such as hypoglycemia, hypokalemia, and cerebral edema, which were presented in percentages similar to those reported in the literature as shown in the results.10,11 Leukocytes were observed with left deviation in DKA and is similar to what has been reported previously.12
For replenishment of electrolytes, the HIES protocol proposes to manage hypotonic or isotonic solutions, depending on the serum sodium, using as a cut-off point 150 mEq/l. With minimal alterations in sodium figures, three patients had serum Na of 125 mEq/l and one case with serum Na of 159 mEq/l, which were resolved without complications during replacement.
With respect to serum K, replacements were done when uresis was established. Wolfsdorf et al. proposed 40 mEq/l (half potassium chloride and half potassium phosphate) and mention that the replacements should be based according to serum K but do not clearly define how much the replacements would be in cases of hypokalemia.13 The HIES protocol proposes ranges up to 70 mEq/l, which would correspond to the maximum rate of substitution of 0.5 mmol/kg/h. If the serum K is from 3.5-5.5, 40-50 mEq/l will be given; if it is in the ranges of 2.5-3.5, 60-70 mEq/l will be given.14 None of the cases studies had anion decompensation such as EKG changes or arrhythmias with hemodynamic changes.15,16
With regard to serum phosphate, levels were replaced according to the current criteria (ISPAD Clinical Practice Consensus Guidelines 2014), half potassium chloride and half potassium phosphate.13 No case presented hypophosphatemia.
Some authors recommend not exceeding from 1.5 to 2 times the maintenance fluids.3,13 It is important to note that as with the HIES protocol, this limitation in rehydration avoids fluid overload with its inherent complications. In a manner similar to other authors,17,18 the HIES protocol clearly defines not surpassing as maximum the 4 l/m2 SC/day. It is proposed that the calculated deficit and replacements be for the ideal weight and not the actual weight (common error that should be avoided) because in obese patients the circulating volume is less with respect to body weight because of the excess of fatty tissue.19
With respect to the days of evolution prior to hospitalization, Wattes and Edge reported onset of symptoms suggestive of DKA up to 2 weeks prior.20 These results are similar to those observed 15 days before in patients studied, which shows that the evolution of DKA is not so acute. Prompt recognition is the key for preventing severe episodes.
Three bioclinical categories were observed (mild, moderate and severe) without large differences in their proportions. Other publications have observed an increase in the frequency of DM1 and with it the appearance of more new cases per year, which describes a 4% increase in cases per year.21,22 The results described here, similar to what is reported by other authors, show progressive increases per year. A relatively stable trend has been observed up to the year 2008. From there, the frequency of DKA has increased as a consequence of a larger number of cases of DM1. These researchers propose carrying out campaigns in the detection of DM in the first level of care and consequently in the prevention of severe episodes of DKA.23 The average hospital stay was 3.6 days; however, length of stay >15 days corresponded to new patients.
The precipitating factors did not show any relevant information, similar as to what was previously reported.24 Infections were found in first place and in second place omission in giving insulin. This occurs mainly in adolescents and is associated with psychological factors of denying the disease and consequentlypoor adherence to taking insulin.
With regard to family history, other publications report a frequency of 54% of family history of DM2.25,26 The results obtained are similar, with 58% of cases positive for DM2, followed by 36% without history and only 6% (eight cases) with family history of DM1.
Socioeconomic status did not show differences with respect to what has already been published.27 The group most affected was that of low socioeconomic status with 101 cases (72%); with respect to the high socioeconomic status there were two cases (1%).
As far as complications, there was acute pulmonary edema in 3% of the patients and 2% had clinical signs of cerebral edema (headache, irritability and altered states of consciousness), one required orotracheal intubation. All were treated according to the HIES protocol, which contemplates administering half of the calculated replacements plus mannitol at a dose of 1-2 g/kg weight every 6 h.
With regard to mortality, recent publications mention different percentages: in the U.S. as low as 0.15-0.30%3,28; other developing countries such as ours, from 4 and up to 18.2%.29,30 Until now, in contrast with these results, patients treated with the HIES protocol have had zero mortality. As far as morbidity of the patients who had clinical presentation of cerebral edema (there was no CT of the skull done), none of the patients had neurological sequelae.
Based on these results, it can be concluded that the HIES protocol is practical and effective for the treatment of electrolytes and acid-base of DKA. An increase has been noted both in DM as well as in its most serious complication, DKA. Therefore, preventive measures are required from the first level of care.
Ethical disclosure
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of data. The authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consent. The authors must have obtained the informed consent of the patients and /or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Conflict of interest
The authors declare no conflict of interest of any nature.
Received 13 August 2015;
accepted 13 September 2015
* Corresponding author.
E-mail:gomez_rivera@yahoo.com.mx (N. Gómez Rivera).
☆ Please cite this article as: Gómez Rivera N, García Zárate MG, Fonseca Chon I, Gómez Figueroa CO, Gómez Jiménez IA, Villalobos García. Cetoacidosis diabética en niños: experiencia hospitalaria. Estudio retrospectivo de 15 años. Bol Med Hosp Infant Mex. 2015. http://dx.doi.org/10.1016/j.bmhimx.2015.09.0022444-3409/