Introducción: La aplasia pulmonar es un raro trastorno del desarrollo pulmonar. Se caracteriza por la presencia de un bronquio principal rudimentario en ausencia de pulmón y arteria pulmonar. Generalmente se asocia con otros defectos congénitos, y debe sospecharse ante la opacidad del hemitórax.
Casos clínicos: Se describen dos casos de pacientes con aplasia pulmonar diagnosticados en el Hospital Infantil de México Federico Gómez en los últimos 5 años. La primera paciente presentó dificultad respiratoria desde el nacimiento. Se observó radiopacidad total del hemitórax izquierdo, y se completó el diagnóstico de aplasia pulmonar con gammagrafía pulmonar y broncoscopia. La evolución ha sido insidiosa, con sintomatología respiratoria crónica, dependencia de oxígeno y neumonías recurrentes. La segunda paciente, de 5 años de edad, permaneció asintomática durante los primeros 2 años de vida. Fue hospitalizada por gastroenteritis infecciosa, y la radiografía sugirió hernia diafragmática derecha. Se intervino y se encontró eventración diafragmática derecha y ausencia de pulmón ipsilateral. Se completó el diagnóstico con broncoscopia que mostró bronquio principal derecho con saco ciego terminal.
Conclusiones: La aplasia pulmonar es una entidad infrecuente. Debido a la variabilidad en la presentación clínica debe tenerse un alto índice de sospecha ante el hallazgo de la radiopacidad total del hemitórax. Los métodos diagnósticos que se utilizan son radiografía, tomografía y gammagrafía. Para confirmar el diagnóstico se requiere realizar broncoscopia. La escisión del muñón y la traslocación diafragmática se han descrito como opciones quirúrgicas de tratamiento.
Background: Pulmonary aplasia is a rare disorder of lung development characterized by the presence of a rudimentary main bronchus in the absence of lung and pulmonary artery. It is generally associated with other congenital defects and must be suspected in the presence of a total radiopaque hemithorax.
Case reports: We describe two cases of pulmonary aplasia diagnosed in the Hospital Infantil de México “Federico Gómez” in the last 5 years. The first case was a female who presented respiratory distress from birth with a radiopaque hemithorax in which the diagnosis of pulmonary aplasia was completed with bronchoscopy and lung scan. Her evolution has been insidious, characterized by chronic respiratory symptoms, oxygen dependence and pneumonias.
The second case is a 5-year-old asymptomatic female who remained healthy during her first 2 years of life. At the time of her hospitalization for gastroenteritis she underwent chest X- rays with findings suspicious of right diaphragmatic hernia. She was then transferred to our hospital. She underwent surgery at which time diaphragmatic eventration and no ipsilateral lung were found. The diagnosis was completed with a blind bottom main right bronchus in bronchoscopy.
Conclusions: Pulmonary aplasia is an uncommon pathology. Due to great variability in clinical presentation, there must be a high index of suspicion in the presence of a fully radiopaque hemithorax. Among the diagnostic methods, chest X-rays, tomography and lung scan are useful. Bronchoscopy is required for diagnostic confirmation. Surgical removal of the stump and translocation of the diaphragm have been proposed as surgical options.
1. Introduction
Pulmonary aplasia is a rare disorder in the development of the lung. It is characterized by the presence of a rudimentary main bronchus in the absence of the lung and ipsilateral pulmonary artery1. From 1762 there have been ~200 cases reported2. It is generally associated with other genetic defects and should be suspected when there is total radio-opacity of the hemithorax. Due to the few cases reported there is no consensus with regards to its evolution, prognosis and treatment. There are only case reports in the literature.
2. Case reports
2.1. Case 1
We present the case of a 2-year-old female patient who was the product of a twin pregnancy. The infant was delivered via cesarean section due to premature rupture of membranes at 32 weeks gestation. She received good Apgar scores at birth and weighed 1640 g. Her twin sister was born with anencephaly and died a few hours after birth.
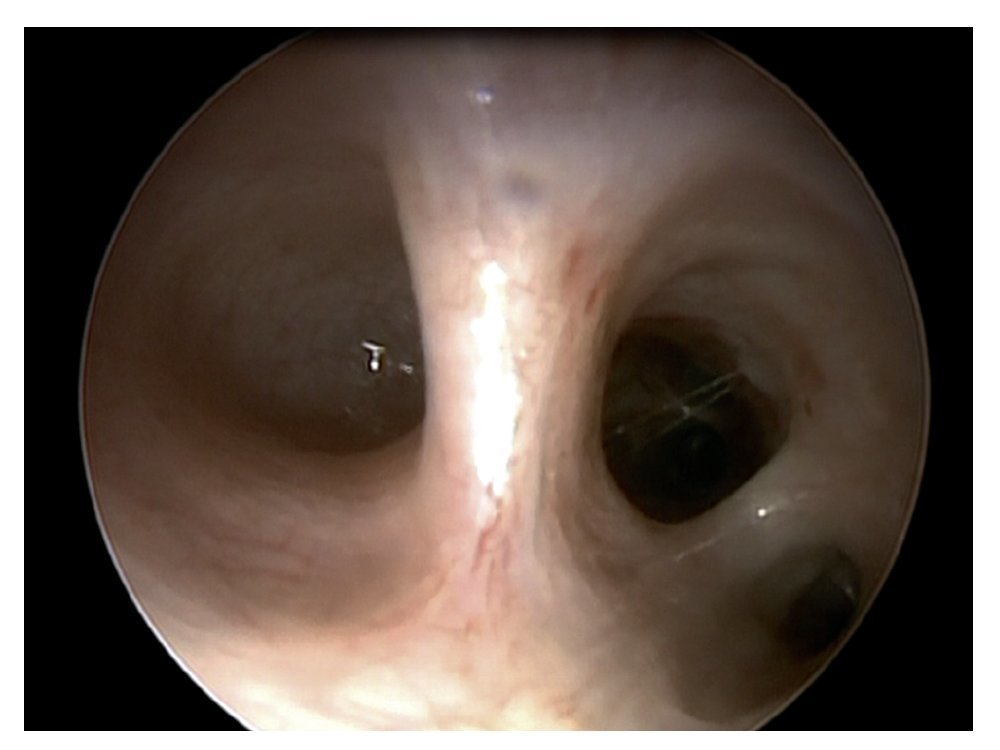
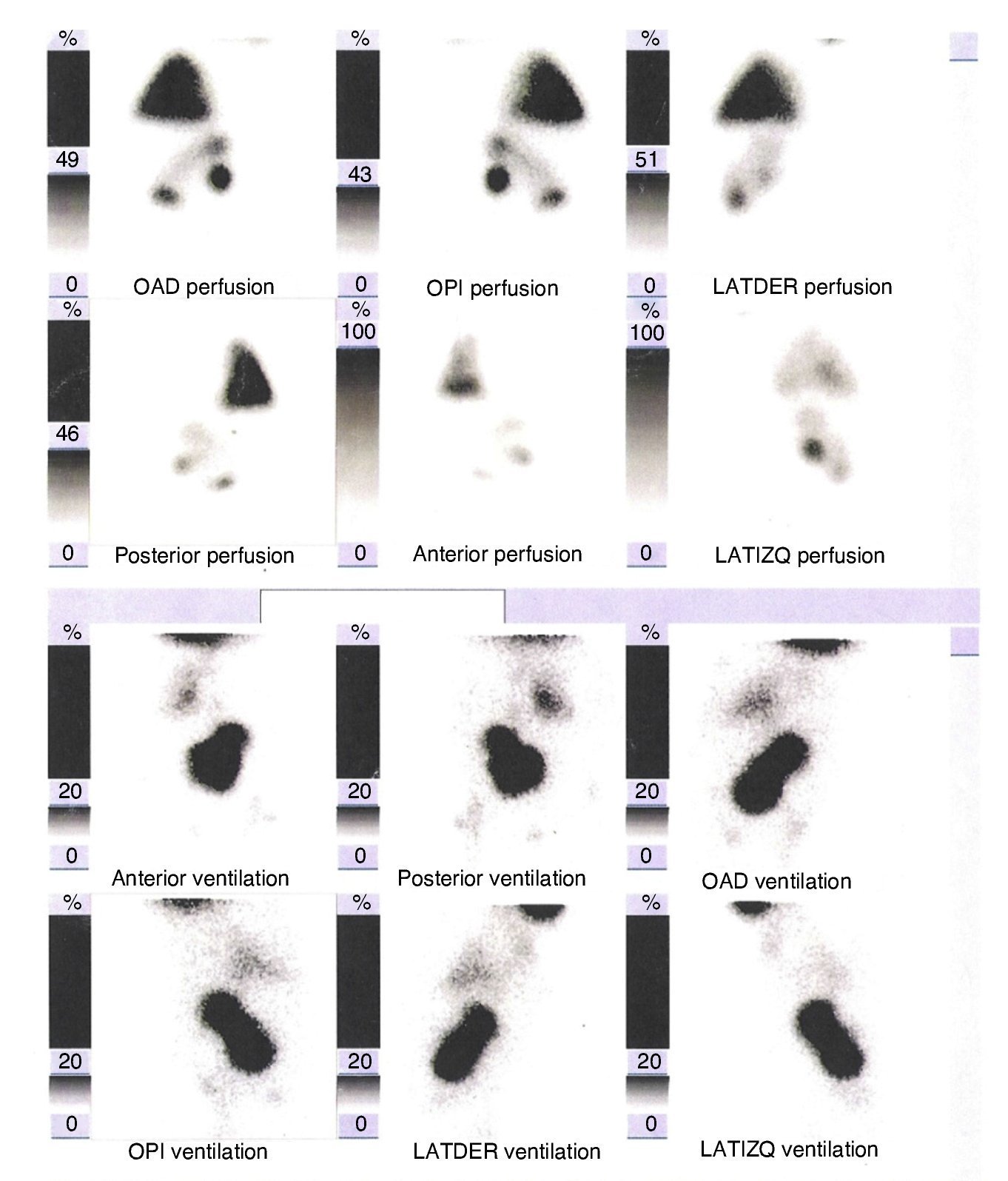
She had respiratory difficulty syndrome from the time of birth requiring noninvasive ventilation for 1 month and antibiotic treatment for neonatal pneumonia. Chest x-ray was done and showed total opacity of the left hemithorax with mediastinal displacement toward the same side. Bronchoscopy was performed at 35 days of life and showed the presence of the carina with left main bronchus ending in a blind pouch (Figure 1). At 42 days of life, ventilation/perfusion scan was done and showed absence of perfusion and ventilation of the left hemithorax (Figure 2), completing the diagnosis of left pulmonary aplasia.
Figure 1 Bronchoscopy where the main carina and the left main bronchus ending in blind cul-de-sac can be appreciated. The right main bronchus is normal. The right upper lobar bronchus and intermediate bronchus can be appreciated
Figure 2 Ventilation/perfusion scan showing lack of uptake of the radiotracer in ventilatory and perfusion phase, which demonstrates absence of the left lung.
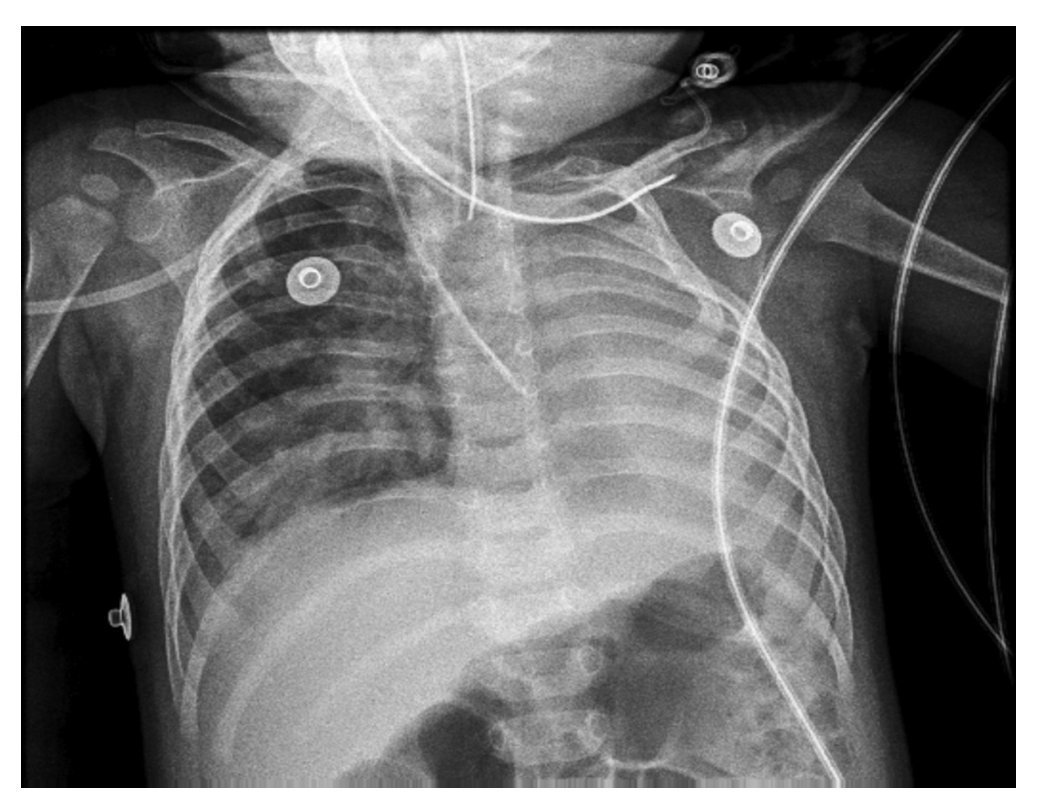
The patient was discharged from the neonatal intensive care unit (NICU) with supplemental oxygen support. The patient has had four occurrences of pneumonia, one of them of viral etiology (PCR positive parainfluenza 2 virus and rhinovirus) requiring mechanical ventilation. At 10 months of age she was diagnosed with small permeable foramen ovale by transthoracic echocardiogram. She has been under continuous surveillance by pulmonary, cardiology and rehabilitation services. She has progressed with chronic cough and was diagnosed with fusion of the second and third left ribs (Figure 3) and right ventricular outflow pressure (PSVD) of 56 mm in her last echocardiogram at 23 months of age. She currently has normal nutritional status, with continuous oxygen supplementation and treatment for pulmonary arterial hypertension with diuretics and sildenafil. Physical examination does not show major disorders other than left hypoventilation with presence of rhonchi and mild thoracic asymmetry due to decreased anteroposterior diameter of the left hemithorax.
Figure 3 Chest x-ray in anteroposterior projection done at 12 months of life during the course of pneumonia. The fusion between two of the first ribs on the left side can be seen as well as total radiopacity of the left hemithorax with ipsilateral mediastinal displacement. The healthy lung is shown to be overdistended with herniation towards the left with alveolar infiltrate.
2.2. Case 2
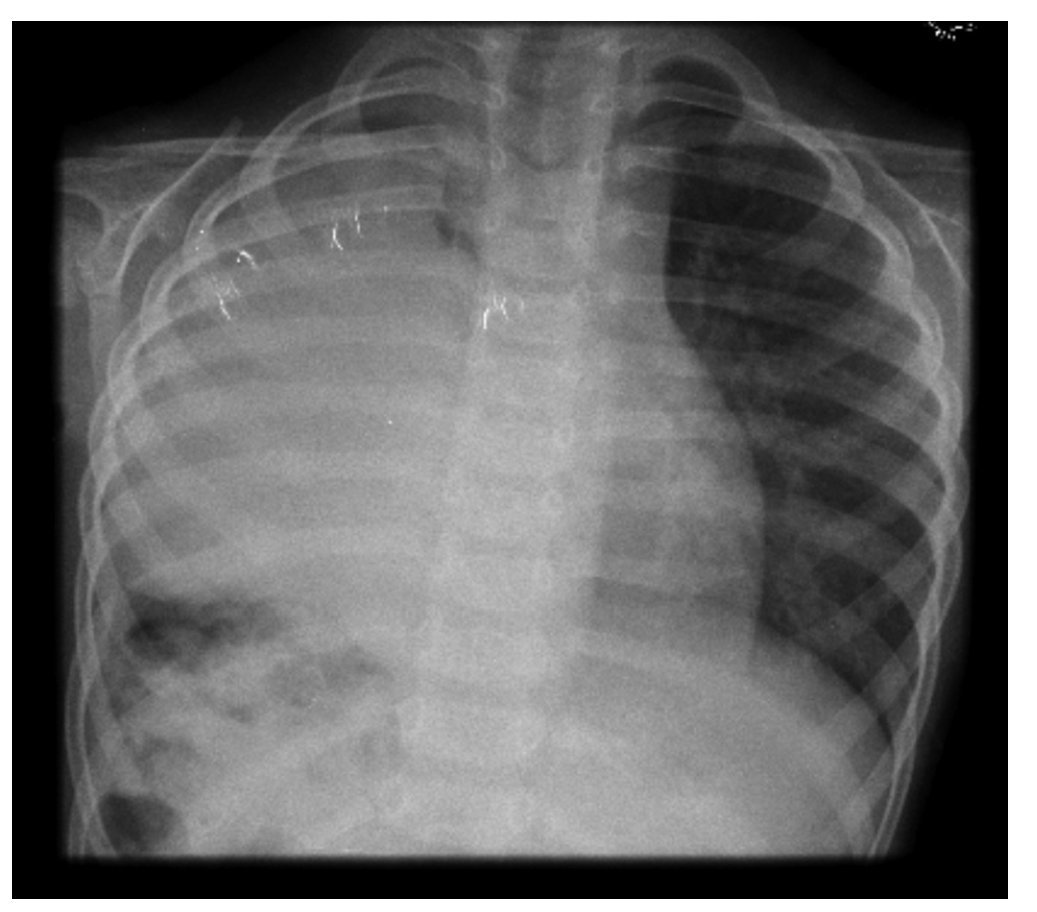
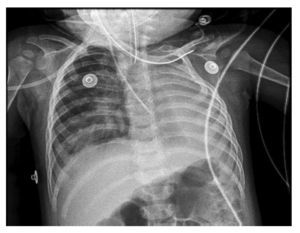
We present a female patient who is currently 5 years 7 months of age. She is the offspring of healthy, non-consangineous parents who are both smokers. She is the product of a managed pregnancy complicated by vaginal and urinary tract infections. She remained healthy until the age of 2 years 7 months when she was admitted to the local hospital due to acute diarrhea. Thoracoabdominal x-ray was done due to abdominal pain and showed elevation of the right hemidiaphragm and apparent intestinal loops within the right hemithorax with suspicion of right hemidiaphragmatic hernia. For this reason, the patient was transferred to this hospital to continue treatment. She had chest x-ray on admission where a right diaphragmatic hernia was suspected (Figure 4) and consequently underwent right thoracotomy. The findings were that of an eventrated right diaphragm, liver below the diaphragm in the thorax, and absence of a lung. A diaphragmatic plication was carried out. The patient showed good postoperative progress. On the sixth day, bronchoscopy was done and showed the right main bronchus ending in a blind pouch (Figure 5). Based on these findings she was diagnosed with pulmonary aplasia. An echocardiogram was done and resulted in a RVSP of 40 mmHg. No structural heart defects were observed. She presented mild psychomotor delay, which has already been corrected. She had a brain MRI and EEG with normal results. The patient continues to be followed at this center. She does not use supplemental oxygen and remains asymptomatic with no major findings on physical examination with the exception of hypoventilation in the right hemithorax.
Figure 4 Chest x-ray showing radiopacity of right hemithorax, trachea and heart in normal position. The main carina and right main bronchus can be appreciated.
Figure 5 Bronchoscopy showing the right main bronchus ending in a in a blind sac.
3. Discussion
Pulmonary aplasia is a rare congenital pathology included among the disorders of pulmonary development. It is defined by the presence of a rudimentary main bronchus that ends in a blind pouch, added to the total absence of the lung and ipsilateral pulmonary artery1. This disorder was first reported in 1762, when it was described by Morgagni. Since then, about 200 cases have been mentioned in the literature2. The combined incidence of aplasia and pulmonary agenesis is estimated to be from 0.0034-0.0097%3. The mortality is from 33% during the first year of life and from 50% in the first 5 years2. However, if a patient survives the first 5 years of life, a normal life without major complications can be expected4. The underlying etiology is unknown although mechanical, teratogenic and genetic factors are involved. In half of the cases, pulmonary aplasia is found to be associated with other congenital malformations, mainly skeletal, genitourinary and gastrointestinal5.
Unlike agenesis where there is no main bronchus, this rudimentary bronchus in aplasia acts as a reservoir for infected secretions that can pass to the contralateral airway, causing recurrent infections and worsening the prognosis4.
Age and manner of presentation are variable. The majority of patients initiate with symptoms during the first year of life. There have been reports of recurrent respiratory infections, dyspnea, cough, stridor, and weight deficit2. On the other hand, there are reports of diagnosis in adults without respiratory symptoms6 or postmortem diagnosis. Radiological studies show similar data, both in pulmonary aplasia as well as agenesis, except for the presence of rudimentary main bronchus in aplasia.
Chest x-ray demonstrates diffuse opacity of all the affected hemithorax with mediastinal shift and elevation of the ipsilateral hemidiaphragm1,7. The healthy lung generally shows over-distention and herniation towards the contralateral hemithorax. Computed tomography (CT) helps demonstrate the absence of parenchyma and pulmonary artery7 as well as the presence of a rudimentary bronchus. Bronchoscopy shows the presence of a main bronchus ending in a blind pouch, confirming the diagnosis. Other studies such as perfusion/ventilation lung scan are useful to distinguish absence of the lung. However, this study does not differentiate between aplasia and agenesis.
Prognosis depends on multiple factors including coexisting congenital malformations, infection of the single lung, pulmonary arterial hypertension, and kinking of the large vessels due to mediastinal displacement. Right lung aplasia translates into a poor prognosis because of the greater rotation of the trachea, heart and large vessels. Pulmonary hypertension in these patients is due to normal blood volume flow through a reduced pulmonary vascular bed. Hypoxemia (potent pulmonary vasoconstrictor) or a heart defect with left to right shunt (increasing the flow to the single pulmonary artery present) would increase the value of the pulmonary pressure with the possibility of evolving towards irreversible pulmonary vascular disease8.
Treatment consists of supportive measures such as oxygen therapy, rehabilitation (to improve clearing of secretions), prevention and early treatment of infections. In some cases, surgical elevation of the ipsilateral hemidiaphragm to the defect has shown good results. In the case of torpid evolution, surgical excision of the stump should be carried out3.
Conflict of interest
The authors declare that there are no conflicts of interest.
Funding
No external funding sources were used.
Received for publication: 12-11-14;
Accepted for publication: 2-2-15
http://dx.doi.org/10.1016/j.bmhimx.2015.02.004
Correspondence:
Dr. Augusto Ignacio Siegert Olivares
E-mail: augustosiegert@gmail.com