Popliteal artery aneurysms (PAAs) are a common peripheral vascular disease with a high risk of complications. While surgical bypass is the mainstay of treatment, graft infection is a devastating complication often leading to limb loss. This case report presents a successful application of a bovine pericardium graft for popliteal artery reconstruction following synthetic graft infection. Traditional management strategies, such as graft explantation and prosthetic replacement, often result in high rates of limb loss and recurrent infection. The patient in this case presented with a PAA, which was initially treated with synthetic graft bypass. Subsequently, a graft infection developed, necessitating surgical intervention. Given the limitations of other options, a bovine pericardium graft was used for reconstruction. The patient demonstrated successful outcomes with the bovine pericardium graft, achieving patency without complications or reinfection. Although preliminary, this case highlights the potential benefits of bovine pericardium grafts in this challenging clinical scenario. Further research is warranted to evaluate the long-term efficacy and safety of this technique.
Los aneurismas de la arteria poplítea (AAP) son una afección vascular periférica con alto riesgo de complicaciones. El bypass quirúrgico es el tratamiento estándar, pero la infección del injerto es una complicación grave. Este reporte de caso presenta un nuevo enfoque utilizando un injerto de pericardio bovino para reconstruir la arteria poplítea tras la infección de un injerto sintético. Las estrategias de manejo tradicionales, como la extracción del injerto y el reemplazo protésico, suelen resultar en altas tasas de pérdida de extremidades y reinfección. El paciente de este caso presentó un AAP, inicialmente tratado con bypass de injerto sintético. Posteriormente, desarrolló una infección del injerto, requiriendo intervención quirúrgica. Dadas las limitaciones de otras opciones, se utilizó un injerto de pericardio bovino para la reconstrucción. El paciente mostró resultados exitosos con el injerto de pericardio bovino, alcanzando permeabilidad sin complicaciones ni reinfección. Aunque preliminar, este caso destaca el potencial de los injertos de pericardio bovino como una valiosa alternativa para el manejo de casos complejos de infección de injerto de arteria poplítea. Se justifica realizar más investigaciones para evaluar la eficacia y la seguridad a largo plazo de esta técnica.
Popliteal artery aneurysms (PAAs) are the most prevalent peripheral arterial aneurysms, accounting for approximately 70% of all cases, with an estimated prevalence of 1%.1 Clinical presentations can range from intermittent claudication to critical limb ischemia, including rest pain, blue toe syndrome, or acral necrosis.1 Untreated PAAs carry a significant risk of limb loss, with up to 30% of patients experiencing acute thrombosis and distal embolization, leading to amputation in 20% and rupture in 2%.2
Open surgical bypass using either autogenous vein or prosthetic grafts remains the mainstay of PAA treatment, boasting high limb salvage rates (86–99%) and acceptable primary patency rates (66–86%) over 5 years.2 However, a major concern following bypass surgery is vascular graft infection (VGI), a complication with significant morbidity and mortality. Occurring in up to 3% of peripheral graft infections, VGI can necessitate amputation in up to 40% of cases.3
Total excision of the infected graft is currently the preferred approach to minimize reinfection.4 This is often followed by debridement and reconstruction with either in situ or extra-anatomical prosthetic bypass. Unfortunately, this strategy is associated with unacceptably high rates of limb loss, mortality, and recurrent infection.5,6 Therefore, novel strategies are urgently needed to improve outcomes following VGI in the popliteal artery.
Bovine pericardium offers a cost-effective and adaptable solution for vascular graft replacement due to its availability and biocompatibility. Retrospective studies suggest its suitability for patient adapted in situ reconstruction of infected aortic grafts. Previous research has documented encouraging outcomes, including graft durability, resistance to reinfection at 24 months and reduced need for revision surgery. Furthermore, studies report 100% patency rates at 2 years, with minimal readmissions for limb ischemia and freedom from reinfection rates ranging from 80% at 5 years to 75% at 10 years.7
This case report presents the potential application of bovine pericardium grafts for reconstruction following popliteal artery synthetic graft infection. We present a successful case utilizing this technique, previously established for aortic graft infections, applied to peripheral synthetic graft infections, to broaden its application in managing infected reconstructions.
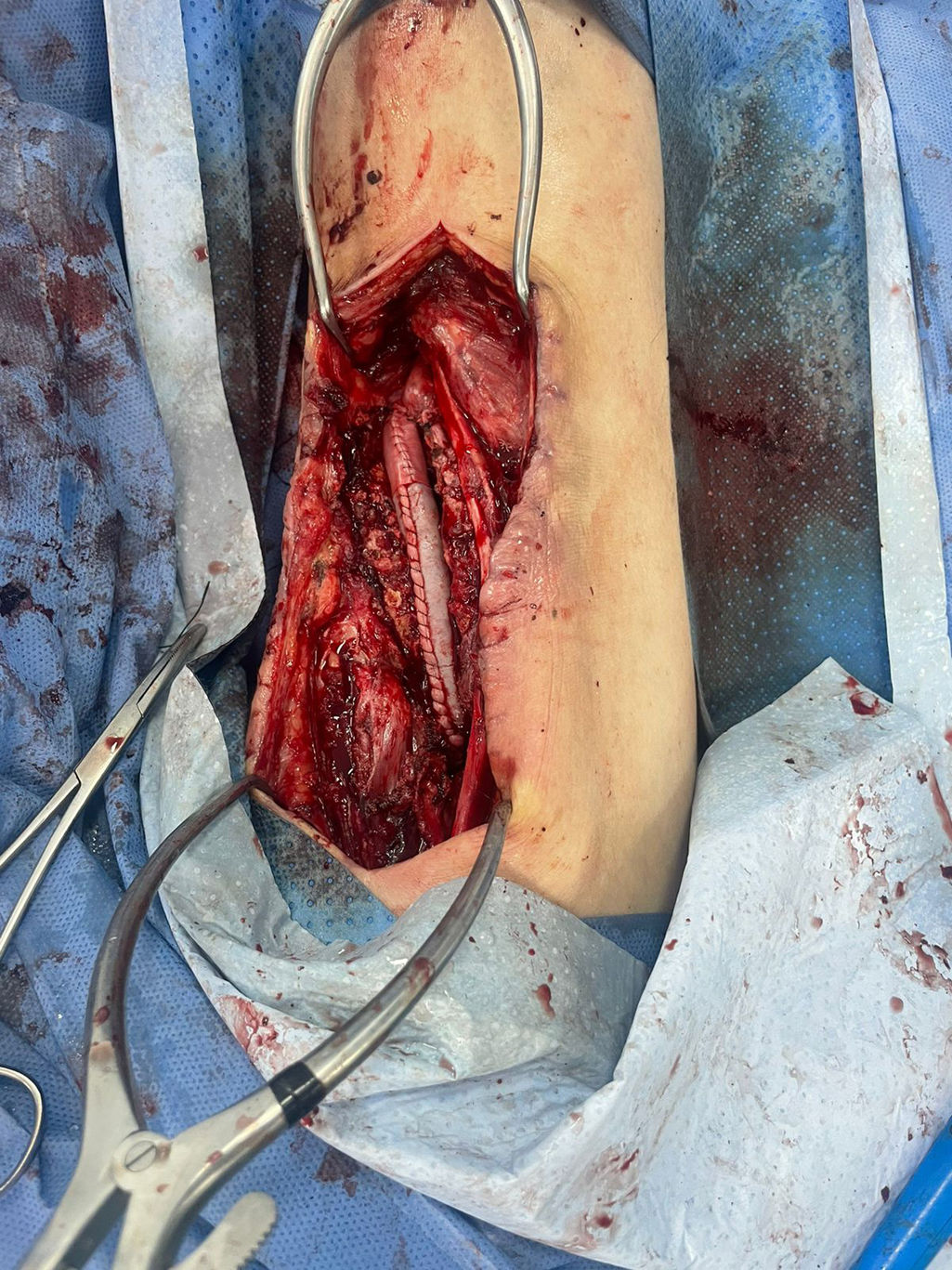
Case reportA 68-year-old male with a 20-year history of smoking with cessation 15 years prior presented with a 4.5cm×4.5cm left popliteal aneurysm containing an intramural thrombus in the P2 segment. Surgical intervention involved resection of the aneurysm and bypass grafting with a 9-mm diameter Dacron graft via a posterior popliteal fossa approach, without intraoperative complications. The postoperative course was uneventful, and the patient was discharged on day 3 without clinical signs of local or systemic inflammation, stigmata of infection, or wound dehiscence. However, the patient re-presented on postoperative day 18 with a one-day history of purulent discharge, erythema, and swelling at the surgical site, suggestive of surgical site infection. Laboratory tests revealed leukocytosis (18,543) with neutrophilia. CT angiography demonstrated a collection with periprosthetic fluid levels but without graft blowout. Additionally, a PET-CT scan showed hyperactivity exceeding 25 units at the lesion, confirming graft infection. Given the patient's history of C3 venous insufficiency requiring bilateral saphenectomy 14 years prior, saphenous vein grafting was not feasible. Therefore, a surgical plan was devised for explantation of the infected P2 popliteal synthetic graft and reconstruction using on-table fashioned bovine pericardium tube graft with a 6-0 polypropylene suture for terminal anastomosis (Fig. 1). An active Jackson-Pratt drain was placed. The patient required a two-day stay in the intensive care unit and four days on the general surgery floor. The drain was removed on day 5, and the patient was discharged with outpatient antibiotic therapy due to the absence of early postoperative complications.
DiscussionThis case report describes the successful application of a bovine pericardial graft for popliteal artery reconstruction following synthetic graft infection. This approach is unprecedented for peripheral interventions but represents a potentially valuable strategy in specific circumstances. In this case, the patient's prior non-biological graft infection significantly increased morbidity and mortality risks. A risk–benefit assessment favored bovine pericardial grafting as a means to potentially reduce surgical site infections, limb amputation, and long-term complications.
Endovascular management was initially ruled out due to the infected Dacron graft, necessitating surgical excision.4 Autologous saphenous vein grafting was also deemed unsuitable due to the patient's history of chronic venous insufficiency. Another promising option, cryopreserved grafts pre-treated with rifampicin, demonstrated success in femoral artery graft infections.8 However, limited availability and high cost ultimately led to the selection of bovine pericardial grafting.
The use of bovine pericardium for reconstructive surgery following graft infection primarily centers on aortic, iliac, and femoral locations, with limited data on peripheral applications. While in situ reconstruction has demonstrated long-term patency advantages, it carries increased perioperative risks due to extended operative times and invasiveness.9 A cohort presented by McMillan et al., encompassed 51 cases, which included three popliteal graft reconstructions, highlighting the scarcity of such procedures. Notably, one patient experienced an acute popliteal arterectomy rupture, necessitating above-knee amputation, emphasizing the potential challenges associated with this technique in the peripheral vasculature.10
Several studies including aortoiliac and femoral applications of this technique, have reported high freedom from reinfection and patency rates, with Kubota et al. and Lutz et al. achieving 100% patency at follow-ups of 13–61 and 1–27 months, respectively. However, these studies were limited by small sample sizes and short follow-up periods.7,11 Additionally, Almasi-Sperling et al. reported a comparable 100% freedom from reinfection rate at six months, although two cases experienced graft occlusion.9 Zientara et al. compared bovine pericardial grafts to other graft types, demonstrating a 100% freedom from reinfection rate at 17 months for the bovine pericardial group.12
Despite encouraging outcomes, the limited data on bovine pericardial grafts in peripheral vascular reconstruction, particularly in the popliteal region, warrants further investigation. Prospective studies with larger cohorts and longer follow-up periods are needed to establish the long-term efficacy and safety of this approach.
There are limitations to this approach. First, data on bovine pericardial grafts specifically for popliteal artery reconstruction following synthetic graft infection are scarce. Second, most existing reports are retrospective, have small sample sizes, and involve short-term follow-up. Finally, there is no clear consensus on optimal pre- and postoperative antibiotic regimens for this specific intervention.
Future research should focus on prospective studies with larger patient cohorts to define the long-term efficacy and safety of bovine pericardial grafts in managing infected peripheral arterial grafts. Additionally, establishing standardized antibiotic protocols for this approach would be beneficial.
ConclusionPopliteal artery aneurysms (PAAs) pose a significant threat to limb viability, and managing infected bypass grafts in this location remains a challenge. Traditional approaches involving graft explantation and in situ reconstruction with prosthetic grafts are associated with high complication rates, including limb loss and recurrent infection. This case report demonstrates the potential application of bovine pericardium grafts as a novel strategy for popliteal artery reconstruction following synthetic graft infection, proving great patency, minimal complications and freedom of reinfection.
Ethical considerationsThis case report meticulously protected both data and patient privacy throughout the study. The Ethics Committee reviewed our rigorous safeguards and determined that the research posed minimal ethical concerns. As a result, our study was granted ethical approval without requiring additional review.
FundingNone declared.
Conflict of interestNone were declared by the authors.