Breast cancer is the leading oncological cause of death in Mexican women over 25 years old. Given the need to improve postoperative cosmetic results in patients with breast cancer, oncoplastic surgery has been developed, which allows larger tumour resections and minor cosmetic alterations.
ObjectiveTo determine the oncological feasibility and cosmetic outcome of oncoplastic surgery at the Instituto de Enfermedades de la Mama, FUCAM, AC.
Material and methodsA review was conducted from January 2010 to July 2013, which included patients with breast cancer diagnosis treated with conventional breast-conserving surgery or with oncoplastic surgery in the Instituto de Enfermedades de la Mama, FUCAM AC. Clinical and histopathological parameters were compared between the two groups, and a questionnaire of cosmetic satisfaction and quality of life was applied.
ResultsOf the 171 patients included, 95 of them were treated with conventional breast-conserving surgery and 76 with oncoplastic surgery. Pathological tumour size was significantly larger in patients treated with oncoplastic surgery (p=0.002). There were no differences found between the groups as regards the number of patients with positive surgical margin, the rate of complications, and cosmetic satisfaction.
ConclusionThis study demonstrates the oncological feasibility and high cosmetic satisfaction of oncoplastic surgery with minimal psycho-social impact on patients.
El cáncer de mama representa la principal causa de muerte de origen oncológico en mujeres mexicanas mayores de 25 años. Ante la necesidad de mejorar los resultados estéticos posquirúrgicos en las pacientes con cáncer de mama, se ha desarrollado la cirugía oncoplástica, la cual permite realizar cirugía conservadora en tumores de mayor tamaño con menor defecto estético.
ObjetivoConocer la factibilidad de la cirugía oncoplástica, su seguridad oncológica, así como el resultado estético en el Instituto de Enfermedades de la Mama, FUCAM A.C.
Materiales y métodosRevisión ambispectiva desde enero del 2010 hasta julio del 2013 en pacientes con diagnóstico de cáncer de mama tratadas con cirugía conservadora convencional o con patrones oncoplásticos en el Instituto de Enfermedades de la Mama, FUCAM A.C. Se compararon entre ambos grupos parámetros clínicos e histopatológicos y se aplicó un cuestionario de satisfacción estética y de calidad de vida.
ResultadosSe incluyó a 171 pacientes, 95 fueron tratadas con cirugía conservadora convencional y 76 utilizando patrones oncoplásticos. El tamaño tumoral determinado por enfermedad fue significativamente mayor en las pacientes tratadas con cirugía oncoplástica (p=0.002), sin diferencias entre ambos grupos con respecto al número de pacientes con borde quirúrgico positivo ni en la tasa de complicaciones. Ambos con un alto grado de satisfacción estética.
ConclusiónEste estudio demuestra la factibilidad y alta satisfacción estética de la cirugía oncoplástica con un mínimo impacto psicosocial en las pacientes.
Breast cancer is the main oncological source cause of death in Mexican women over 25 years of age.1 It is estimated that 12% of women will develop breast cancer during their lifetime.2 In 2014, more than 230,000 new cases of breast cancer were diagnosed in the United States and nearly 40,000 died that year from this cause.2,3
Mastectomy has for a long time been the treatment of choice for breast cancer. Currently, conservative breast surgery with added radiotherapy is fully accepted as treatment for breast cancer in early stages.4 In several studies it has been proven that conservative surgery presents no difference in global survival and the period free from disease as compared to mastectomy.5,6
Despite the increase in the frequency of breast preservation in the treatment of breast cancer, 20–30% of these patients will present an unfavourable aesthetic result, especially if wide excisions are required, mainly above 20% of the total volume of the breast, or tumours located in unfavourable areas, such as the internal quadrants of the breast.7,8
Given the increasing need to improve aesthetic results in patients with breast cancer, several authors have made efforts during the past decades to offset this adverse result without compromising the oncological goals. According to Urban et al. in 1980, Jean-Yves Peitt and Michel Abbes applied plastic surgery techniques in conservative breast surgery. Later, the German Werner Audrescht coined the term oncoplastic surgery, which was popularised by French surgeon Krishna Clough in 2003.8
In these last years, oncoplastic surgery has been used more frequently in the treatment with breast cancer.9 It is an innovative approach which allows larger tumour resections with wide margins and fewer aesthetic consequences.10 It is especially indicated when more than 20% of the breast volume has to be resected, when there is macromasty, ptosis or asymmetry, in tumours with central, medial or inferior location, or when there are prior surgeries in the affected breast.8
Oncoplastic surgery has notably improved the aesthetic result of patients treated for breast cancer, since wider resection margins can be obtained through these techniques as compared to conservative surgery, with a decrease in the recurrence rate and improved survival.10,11
ObjectiveThrough this study, the goal is to explore the feasibility of oncoplastic surgery, its oncological safety, as well as the aesthetic result at the Instituto de Enfermedades de la Mama, FUCAM A.C.
Materials and methodsAn ambispective study was carried out from 1 January 2010 to 31 July 2013. All patients with breast cancer diagnosis treated with conventional conservative surgery or oncoplastic patterns at the Instituto de Enfermedades de la Mama, FUCAM A.C., with a complete clinical file and who answered the aesthetic satisfaction questionnaire, whether in person or via telephone, were included. Those who did not continue their follow-up at the institute were eliminated from the study. Clinical and histopathological parameters were evaluated between both groups, as well as the degree of aesthetic satisfaction and quality of life of the European Organisation for Research and Treatment of Cancer ((EORTC QLQ-C30), FACT-B questionnaire at FACIT.org and Breast-Q through the questionnaire answering “1: none, 2: slightly, 3: regularly, 4: a lot, or 5: full”, as considered, to each question.12 Treatments were established during the tumours session pursuant to the treatment standards of international medical guidelines.
Baseline characteristics of both groups are expressed as means and typical deviation (standard deviation). In the invariable analysis, the means were compared through a non-parametric Mann–Whitney U test or the t-Student test in the case of variables with normal distribution.
Also, proportions with their related 95% confidence intervals were obtained. The result was considered statistically significant if the p value was lower than 0.05.
ResultsFrom January 2010, 278 patients were treated with conservative surgery at Instituto de Enfermedades de la Mama, FUCAM, A.C. Of those, 171 patients were included in this study, who, in addition to having been treated with conservative surgery with or without oncoplastic pattern, had the full file, continued under follow-up at the institute and answered, whether in person or over the phone, the established aesthetic satisfaction questionnaire.
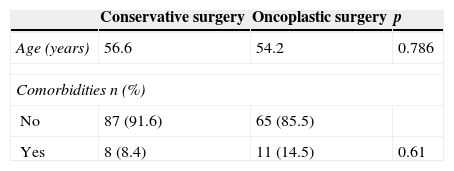
Of the 171 patients included, 95 were treated with conventional conservative surgery and 76 using oncoplastic patterns. No significant differences were found between the groups as regards age, comorbidities, use of tobacco and the body mass index (Table 1). The mean age of patients included in the study was 55.6 years (range of 27–84 years). The mean of follow-up was 19.6 months (range 2–44 months).
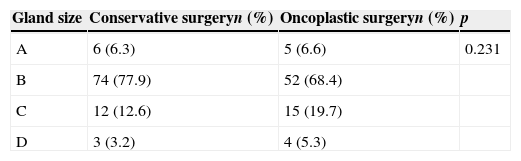
Clinical parametersThe gland size of patients was determined through the bra cup size used, and no significant differences were found between both groups (p=0.231) (Table 2).
Breast regions established to determine tumour location were the following: retroareolar region, super-external quadrant, infero-external quadrant, infero-internal quadrant and supero-internal quadrant. In both groups, the tumour location was homogeneous (p=0.138). The supero-external quadrant was the most common site in both groups.
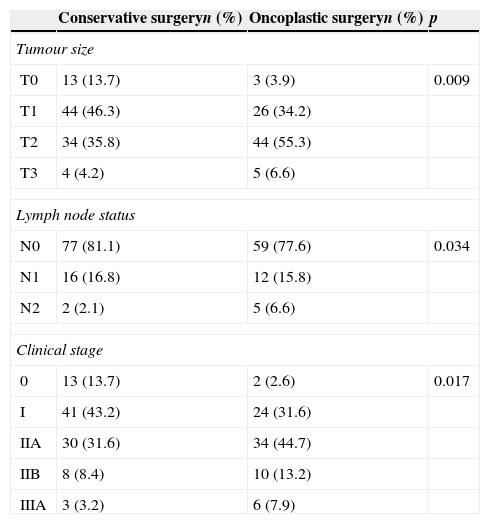
According to the AJCC/TNM classification system, the tumour clinical stage of all patients was determined taking into consideration the tumour size and axillary lymph nodes, in the absence of metastasis.13 It was proved that in the group of oncoplastic surgery, larger tumours were included as compared to the conventional conservative surgery group (p=0.009), but no differences were found between the groups as regards lymph nodes state (p=0.34). Clinical stages were significantly higher in patients with oncoplastic surgery. This was due to the size of the tumour, not the lymph node status (p=0.017) (Table 3).
Clinical stages (TNM).
| Conservative surgeryn (%) | Oncoplastic surgeryn (%) | p | |
|---|---|---|---|
| Tumour size | |||
| T0 | 13 (13.7) | 3 (3.9) | 0.009 |
| T1 | 44 (46.3) | 26 (34.2) | |
| T2 | 34 (35.8) | 44 (55.3) | |
| T3 | 4 (4.2) | 5 (6.6) | |
| Lymph node status | |||
| N0 | 77 (81.1) | 59 (77.6) | 0.034 |
| N1 | 16 (16.8) | 12 (15.8) | |
| N2 | 2 (2.1) | 5 (6.6) | |
| Clinical stage | |||
| 0 | 13 (13.7) | 2 (2.6) | 0.017 |
| I | 41 (43.2) | 24 (31.6) | |
| IIA | 30 (31.6) | 34 (44.7) | |
| IIB | 8 (8.4) | 10 (13.2) | |
| IIIA | 3 (3.2) | 6 (7.9) | |
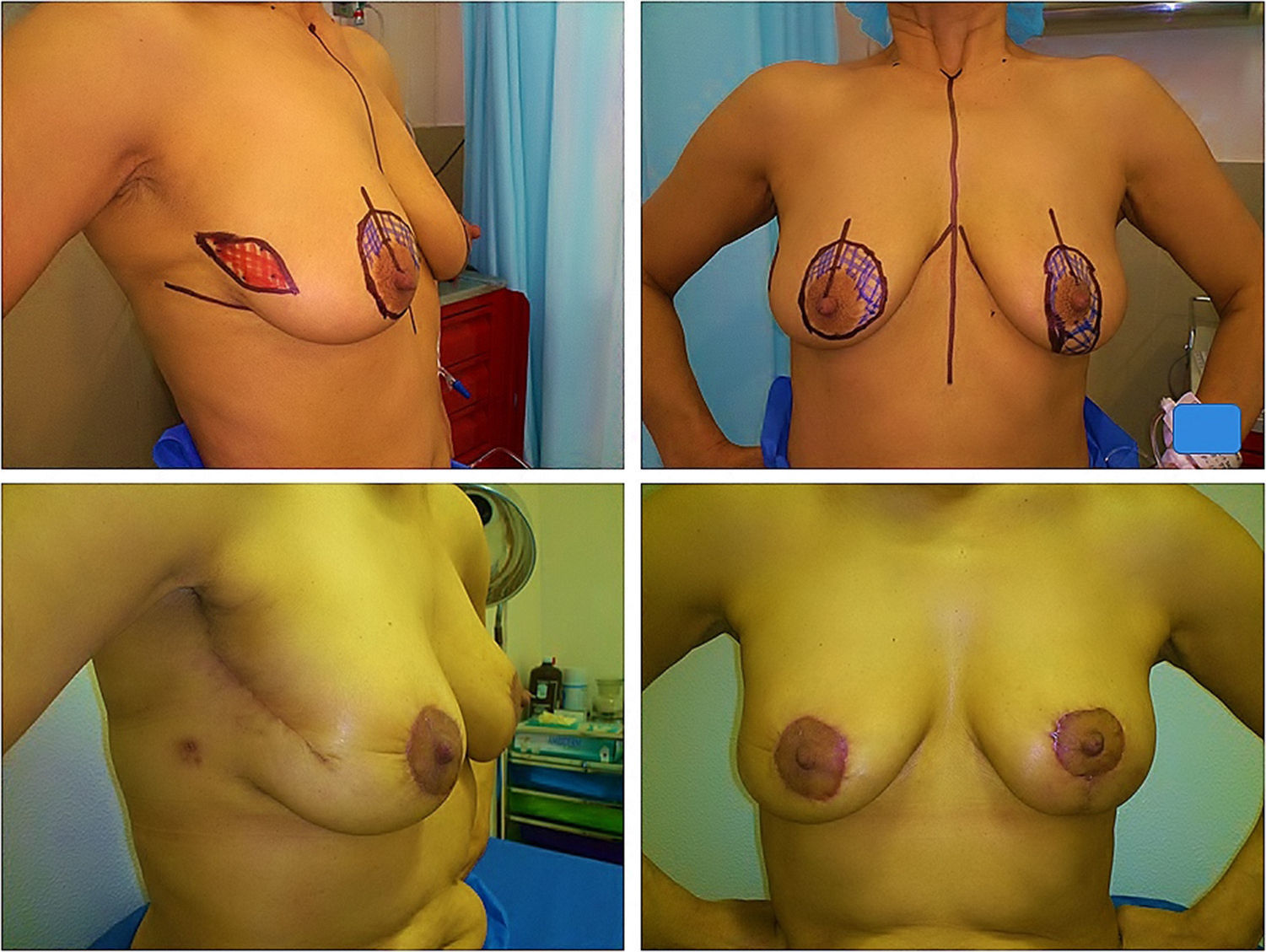
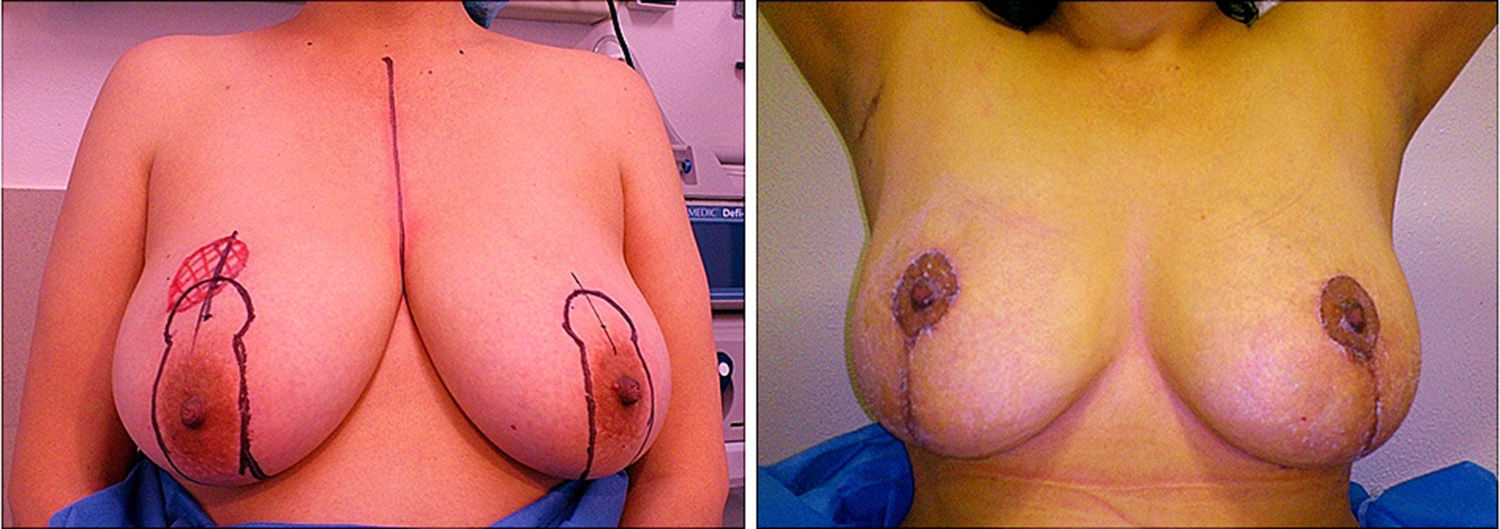
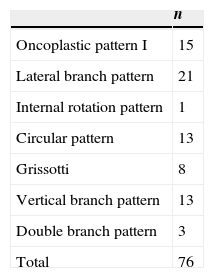
The treatment of each patient was determined during tumour sessions. While 10 patients (10.5%) of the conservative surgery group received neoadjuvant chemotherapy, 31 patients (40.8%) treated with oncoplastic surgery received it (p<0.001). Of the 171 patients included in the study, 95 were treated with conventional conservative surgery and 76 using oncoplastic patterns. 28 of those had a contralateral symmetrisation. Oncoplastic patterns used were determined during the tumours session based on the location of the tumour in the breast14 (Table 4) (Figs. 1 and 2).
Oncoplastic patterns.
| n | |
|---|---|
| Oncoplastic pattern I | 15 |
| Lateral branch pattern | 21 |
| Internal rotation pattern | 1 |
| Circular pattern | 13 |
| Grissotti | 8 |
| Vertical branch pattern | 13 |
| Double branch pattern | 3 |
| Total | 76 |
Regarding adjuvant treatments administered, it was found that 57 patients of the total received adjuvant chemotherapy, 28 patients had tumours with Her-2 overexposure, and therefore received anti-Her-2 therapy with trastuzumab, and 138 patients received hormonal therapy with tamoxifen or aromatase inhibitors, indicated in all patients with positive oestrogen or progesterone receptors, as standard treatment. Out of the total patients included in the study, 169 received radiotherapy, whether externally with increase in the bed, or intraoperatively. In 2 patients, radiotherapy was not considered given the advanced age and favourable clinical and histopathological characteristics.
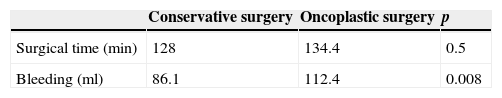
Surgical parametersIt has been determined that patients treated with oncoplastic surgery had a higher operating time with no significant difference with the conservative surgery group (p=0.5). On the other hand, the use of oncoplastic patterns presented more intraoperative bleeding as compared to patients treated with conservative surgery only, but no cases requiring blood transfusion afterwards were recorded (Table 5). The hospital stay was a maximum of one day in 161 patients and 2 days in the rest.
Pathological anatomyThe tumour size determined by pathology was significantly higher in patients treated with oncoplastic surgery (p=0.002). While the mean size in patients treated with conservative surgery was 1.4cm with a maximum size of 4.4cm. In the group with oncoplastic surgery, it was 2cm with a maximum of 6cm resected.
Regarding the mean of the closest surgical margin, it was 9.6mm in patients with conservative surgery with a maximum of 25mm and 7.1mm for patients treated with oncoplastic surgery, but margins of up to 29mm were obtained in this group (p=0.006). On the other hand, only 2 patients of each group presented positive tumour border in the final pathology report, and required broadening of the surgical treatment (p=0.602).
Only one recurrence was found in the group of conservative surgery, while in the group of oncoplastic surgery, none has been detected so far.
ComplicationsSeveral complications were recorded regarding the surgical procedure per se, which will be recorded in the file. These were wound infection, dehiscence, reoperation for positive margins, haematoma, seroma, cutaneous necrosis, AP necrosis, dystrophic scar, severe pain or asymmetry as compared to contralateral breast. In global terms, 16 patients (16.8%) of the conservative surgery group and 14 (18.4%) of the oncoplastic surgery group had some type of complication (p=0.471).
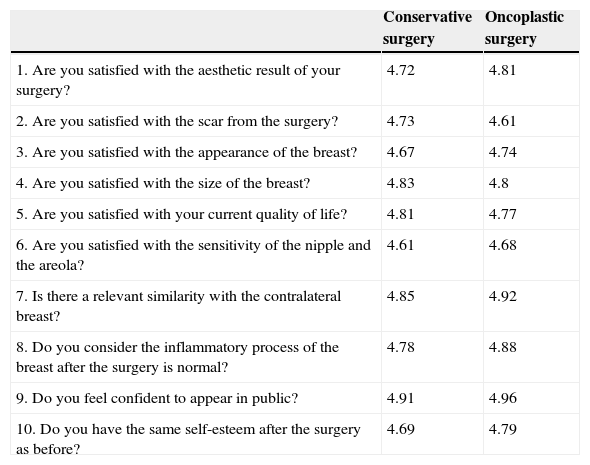
QuestionnaireAs regards the questionnaire, no significant differences were found between both groups (p=0.256), with a high level of aesthetic acceptance and a mild social and psychological affectation of patients (Table 6).
Aesthetic satisfaction and psychosocial impact questionnaire.
| Conservative surgery | Oncoplastic surgery | |
|---|---|---|
| 1. Are you satisfied with the aesthetic result of your surgery? | 4.72 | 4.81 |
| 2. Are you satisfied with the scar from the surgery? | 4.73 | 4.61 |
| 3. Are you satisfied with the appearance of the breast? | 4.67 | 4.74 |
| 4. Are you satisfied with the size of the breast? | 4.83 | 4.8 |
| 5. Are you satisfied with your current quality of life? | 4.81 | 4.77 |
| 6. Are you satisfied with the sensitivity of the nipple and the areola? | 4.61 | 4.68 |
| 7. Is there a relevant similarity with the contralateral breast? | 4.85 | 4.92 |
| 8. Do you consider the inflammatory process of the breast after the surgery is normal? | 4.78 | 4.88 |
| 9. Do you feel confident to appear in public? | 4.91 | 4.96 |
| 10. Do you have the same self-esteem after the surgery as before? | 4.69 | 4.79 |
Oncoplastic surgery techniques have had a major application in the treatment of breast cancer for the purposes of decreasing the incidence of aesthetic defects caused by the mastectomy and the conservative surgery. Up to 20% of cases were reported in patients treated with this method.9
Clough et al.7 have divided or classified oncoplastic surgery in 2 levels, I and II. The first is indicated when the volume to be resected is less than 20% and does not require skin removal or mammoplasty, in cases where there is macromasty, ptosis or asymmetry as compared to contralateral breast. Level II is carried out when 20 to 50% of the breast volume has to be removed and breast remodelling is required.
In this comparative study, with a follow-up mean of 19.6 months, we prove that no significant differences were found between both groups as regards age, comorbidities and the use of tobacco. In addition, there was also no significant difference in the gland size of both groups.
The treatments of each patient were determined during the tumour sessions at the institute. Given the absence of factors contraindicating the conservative surgery, the proper breast-tumour relation was key in determining the possibility of breast preservation.
A higher proportion of patients, nearly 62% in the group of oncoplastic surgery, had T2 and T3 tumours, while only 40% of patients with conservative surgery had this tumour size. Also, although 40.5% of patients treated with oncoplastic surgery received neoadjuvant chemotherapy, the tumour size reported for disease was significantly higher as compared to that in the group of conservative surgery. Therefore, the tumour size was considerably higher, both clinically and pathologically in the group of oncoplastic surgery, regardless of the fact that there was no difference in the gland size reported between both groups. Therefore, through the oncoplastic techniques, the number of patients treated with conservative surgery was increased, larger tumours were resected with no relevant aesthetic defects, and it was proved that neoadjuvant chemotherapy is an extremely useful tool to improve the breast-tumour ratio.
Surgical margins were higher in conservative surgery, although those for the group of oncoplastic surgery are still sufficient for oncology purposes.15 The same positive margins rate exists for both groups, 2 patients for each group, for whom the mastectomy was the applicable treatment. Negative margin rates have been reported for only 81% in oncoplastic surgery, although in this study, a 97.4% rate is proved.11
In oncoplastic surgery, a longer surgical time is expected, and higher operative bleeding due to the surgical techniques used, such as movement of flaps, the areola-nipple complex, or symmetrisation of contralateral breast. Despite this, there were no complications during or after surgery and none of the patients included in this study required blood transfusions.
Also, it is worth noting that, although more complex surgical techniques are used in oncoplastic surgery, no patient had delays in beginning adjuvant chemotherapy or radiotherapy. Likewise, the rate of complications was very similar in both surgical groups (16.8–18.4%), slightly lower than that reported in other studies with rates of up to 24%.7,16
Patients with positive margins in the group of oncoplastic surgery were treated with mastectomy afterwards, but a broadening of margins has been described in 2 more cases, as a feasible treatment in this subgroup of patients.17 It has been stated that the mastectomy rate for positive margins after oncoplastic surgery is between 3 and 16%, while in this study it is 2.6%.18
A recurrence rate after oncoplastic surgery from 2 to 7% has been reported, while in conservative surgery it is 10–14%.9 So far, there were no local recurrences in patients treated with oncoplastic surgery included in the study, and only one in the group of conservative surgery. But, ultimately, a longer follow-up period is recommended.
Consistent with other studies, it has been shown that oncoplastic surgery has a high acceptance rate by patients, derived from its excellent aesthetic result and a low impact in patients’ everyday life. Fitoussi et al.11 report rates with good results as regards aesthetics, close to 93%. We show that patients’ quality of life, their self-esteem and social development are minimally affected after oncoplastic surgical treatment.
As mentioned before, oncoplastic surgery is ideal for patients with some degree of breast ptosis, or breast hypertrophy, since these conditions can be corrected through these patterns, avoiding or relieving back pain derived from these diseases, as well as offering a safe oncologic treatment.19
It is therefore feasible to resect larger tumours with proper oncologic margins, where these could probably not have been resected with conventional conservative surgery without major aesthetic defects.
ConclusionThis study demonstrates the feasibility and high aesthetic satisfaction of oncoplastic surgery with a minimum social and psychological impact on patients. Comparatively, in the group of oncoplastic surgery, larger tumours were resected with oncological satisfactory margins, despite there being no differences in the gland size between both groups. Resection of larger tumours was possible with no major aesthetic defects. The number of patients treated with conservative surgery can be increased with oncoplastic techniques.
It is even possible, through this approach, to treat breast conditions such as hypertrophy or breast ptosis. On the other hand, by carrying out more limited resections in the group of conventional conservative surgery, the aesthetic impact at the breast level should consequently be lower.
Although oncoplastic surgery requires a more challenging surgical technique, operating time was not significantly higher and the rate of complications was similar in both groups. The quality of life, self-esteem and social development of patients with oncoplastic surgery are only slightly affected after the surgery.
Although the follow-up has been nearly 2 years with no recurrences so far in the study group, a longer period is necessary to assess long term-recurrence and survival rates.
Conflict of interestThe authors declare that there are no conflicts of interest.
The Instituto de Enfermedades de la Mama, FUCAM, A.C., all who work there, and especially all patients who generously participated in the study.
Please cite this article as: Sherwell-Cabello S, Maffuz-Aziz A, Villegas-Carlos F, Domínguez-Reyes C, Labastida-Almendaro S, Rodríguez-Cuevas S. Factibilidad y resultado estético de la cirugía oncoplástica en el tratamiento de cáncer de mama. Cir Cir. 2015;83:199–205.