Chylopericardium is a rare occurrence in children. The most common causes are associated with cardiac surgery, malformations of the lymphatic system, idiopathic reasons, among others.
ObjectiveThe case is presented of a patient with traumatic chylopericardium, the diagnostic methodology, and in particular, its successful resolution by surgical means.
Clinical caseMale patient of 6 years old, previous accident of fall from patient's height. Chest X-ray showed evidence of cardiomegaly. An echocardiogram with pericardial effusion was performed. Pericardial puncture was performed with drainage of milky material, confirming chylous liquid. Treatment included pericardial catheterisation, total parenteral nutrition, octreotide, and diet with medium chain triglycerides, with persistent increased pericardial fluid. Lymphatic abnormalities were ruled out by MRI. He underwent surgical treatment due to failure of prior treatment. A thoracoscopic approach was adopted with a favourable outcome.
ConclusionsChylopericardium occurs in children in most cases after cardiovascular surgery. The case presented here was classified as idiopathic. Patients with this condition may present with severe symptoms, such as tamponade, or can be asymptomatic as in the case presented. If medical treatment fails, it should be resolved by surgery; the best choice is minimally invasive treatment with its well-known advantages.
El quilopericardio es una entidad rara en pediatría. Las causas más frecuentes están asociadas a cirugía cardiaca, malformaciones del sistema linfático o idiopáticas.
ObjetivoPresentar el caso de un paciente con quilopericardio traumático, su metodología diagnóstica así como su resolución quirúrgica.
Caso clínicoPaciente varón de 6 años de edad, con antecedente de caída desde su propia altura. Radiografía de tórax con evidencia de cardiomegalia. Ecocardiograma con presencia de derrame pericárdico. Se realizó punción pericárdica, con drenaje de líquido de aspecto lechoso, similar al quilo. El tratamiento fue mediante colocación de sonda pericárdica y NPT, octeótrido y dieta con triglicéridos de cadena media persistiendo el drenaje. Se descartaron anomalías linfáticas por resonancia magnética. Se sometió a tratamiento quirúrgico mediante un abordaje toracoscópico, por falla en la respuesta al manejo conservador, con resultado favorable.
ConclusionesEl quilopericardio en niños se presenta en la mayoría de los casos después de una cirugía cardiovascular. El caso aquí presentado ha sido catalogado como traumático. Los pacientes con este padecimiento pueden cursar con síntomas graves de tamponade o asintomáticos como el caso aquí reportado. Cuando hay falla al tratamiento médico se debe resolver con cirugía de mínima invasión, con las ventajas ya conocidas de estos abordajes.
Chylopericardium is the accumulation of chyle in the pericardial space. It is a rare disorder in children.1,2 The most frequent causes are associated with cardiac surgery or malformations of the lymphatic system, lymphangiomas or even mediastinal tumours.3–5 It is not always possible to establish its aetiology and these cases are referred to as idiopathic.6–9 Most reports refer to adult patients.1 The few publications regarding children refer to patients who have undergone some form of cardiovascular surgery, there are very few reports on spontaneous chylopericardium in children.6–11
Initial treatment should be medical, using parenteral nutrition, diets with medium chain triglycerides, and in some cases the use of octreotide has been recommended. When medical treatment has failed, if the initial symptoms are serious or there is a high volume of drainage, surgical treatment should be considered, which consists of ligating the thoracic duct.10–14
The objective of this study is to present the case of a child who developed a chylopericardium seemingly as a consequence of a fall, its diagnostic methodology and its successful resolution by means of minimally invasive surgery.
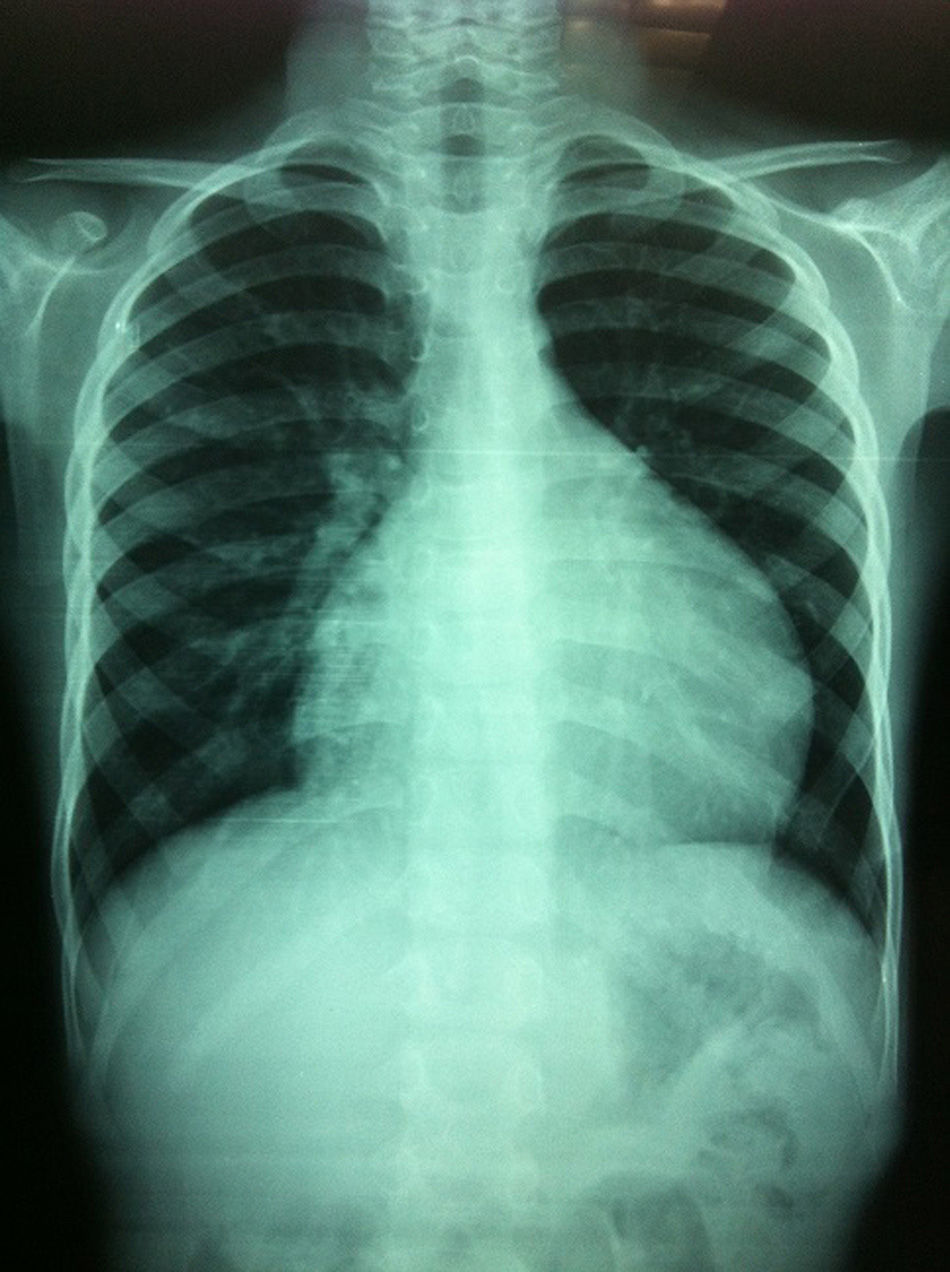
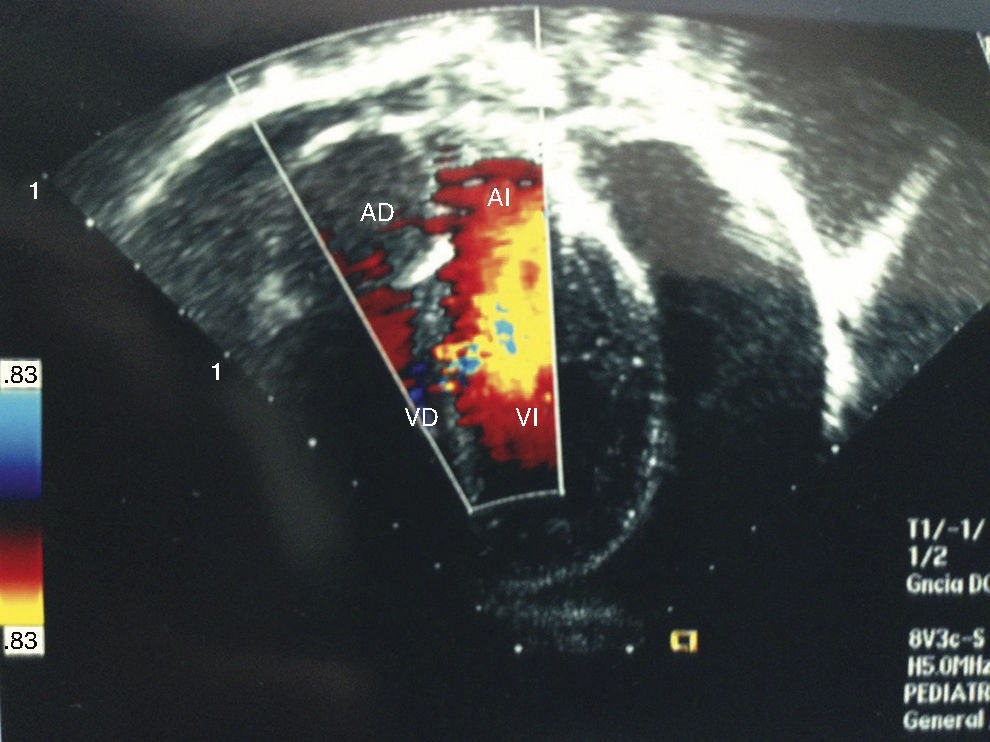
Clinical caseA 6-year-old male patient, with no history of significance, onset of the disorder was 3 weeks before his admission when he fell from his own height, presenting pain in the cervical and lumbar region. Chest pain started after 2 weeks, and a chest X-ray was requested which showed cardiomegaly (Fig. 1). It was evaluated by paediatric cardiology, who found reduced cardiac tone, with no signs of tamponade or heart failure. An electrocardiogram was performed which showed a drop in voltage in all branches, and an echocardiogram was undertaken which showed the presence of pericardial effusion, which was quantified at 500ml (Fig. 2).
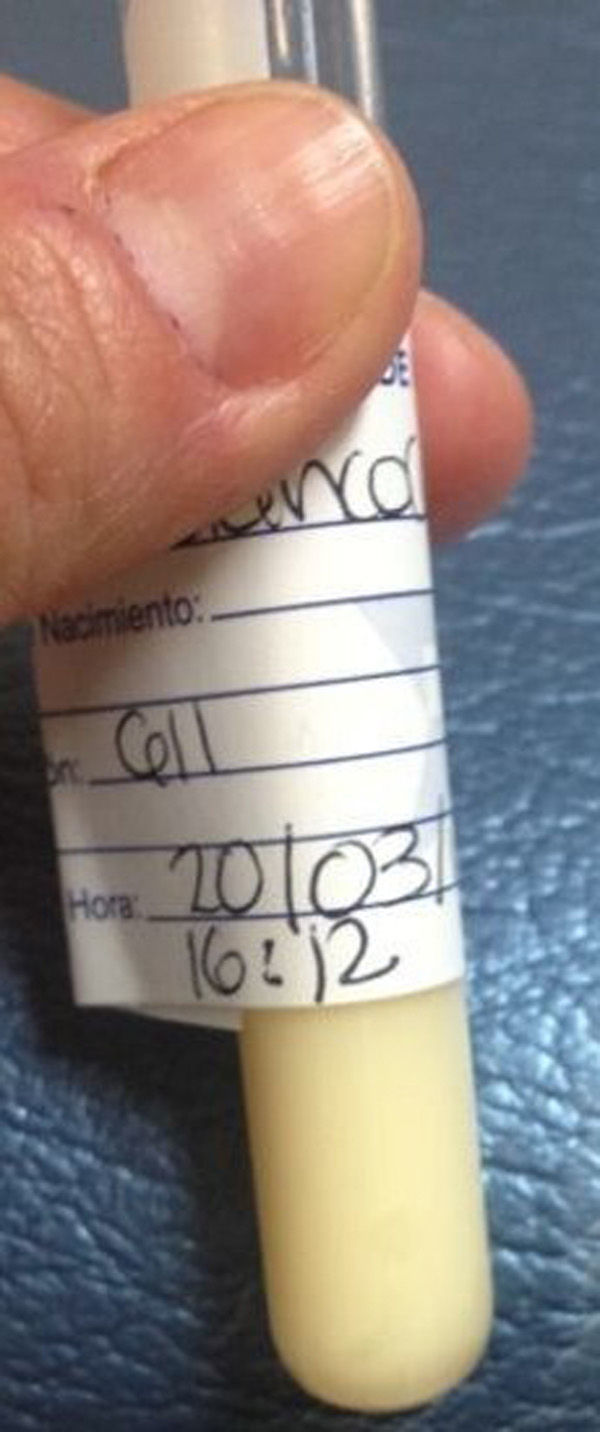
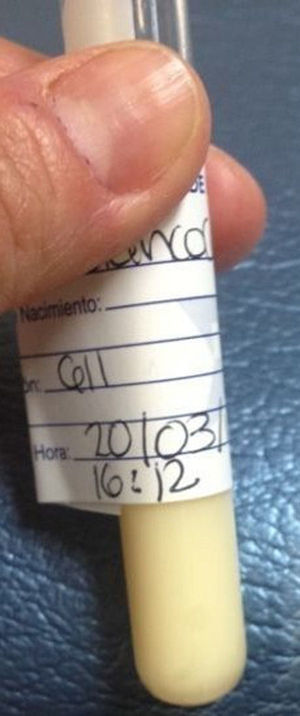
Given these findings, a pericardial puncture was undertaken, and 300ml of a milky fluid was obtained (Fig. 3), and an anterior pericardial tube was placed. Cytochemistry of the aspirated fluid reported: triglycerides 1910mg/dl and 80mg/dl cholesterol. Electrophoresis of the pericardial fluid showed: beta lipoproteins 13.6mg/dl, pre beta lipoproteins 64.1mg/dl, alpha lipoproteins 1mg/dl, chylomicrons 21.3mg/dl. Magnetic resonance was performed in order to rule out any lymphatic malformation or mediastinal tumour, and was normal.
Treatment was started with fasting, total parenteral nutrition and octreotide at a dose of 100mcg/m2, administered subcutaneously. Chyle loss through the drain on the first day was 0.3ml/kg/h, which increased to 1ml/kg/h, and therefore as medical treatment had failed, the option of surgical treatment was considered since, rather than reducing the loss, with medical treatment it had significantly increased.
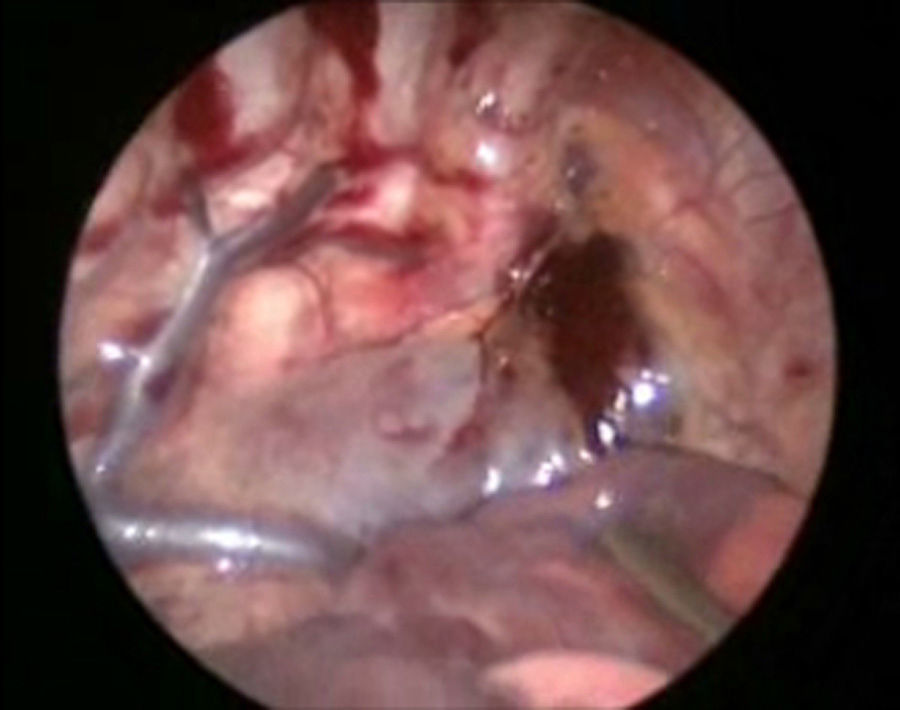
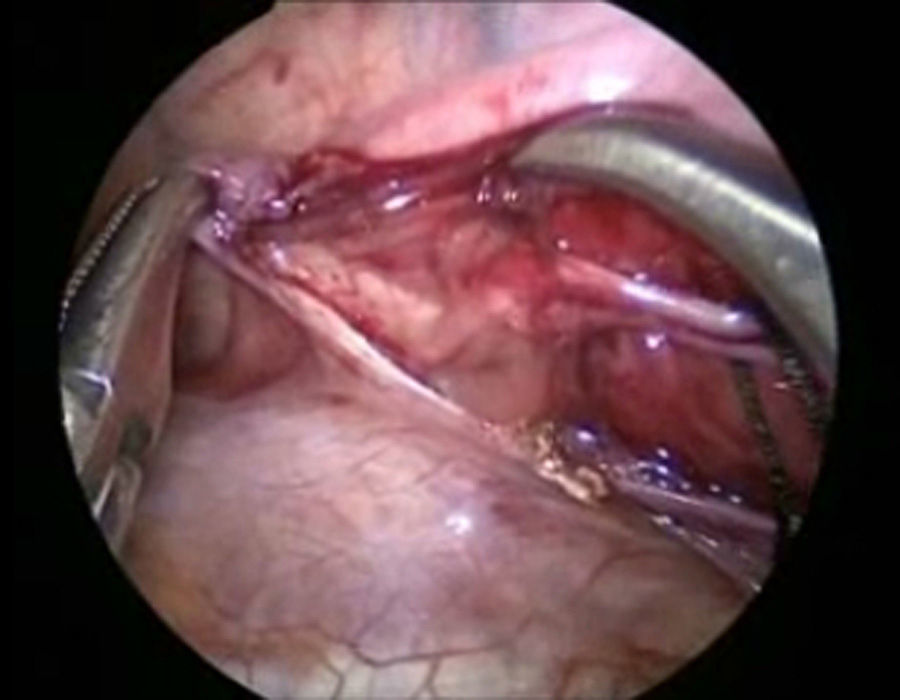
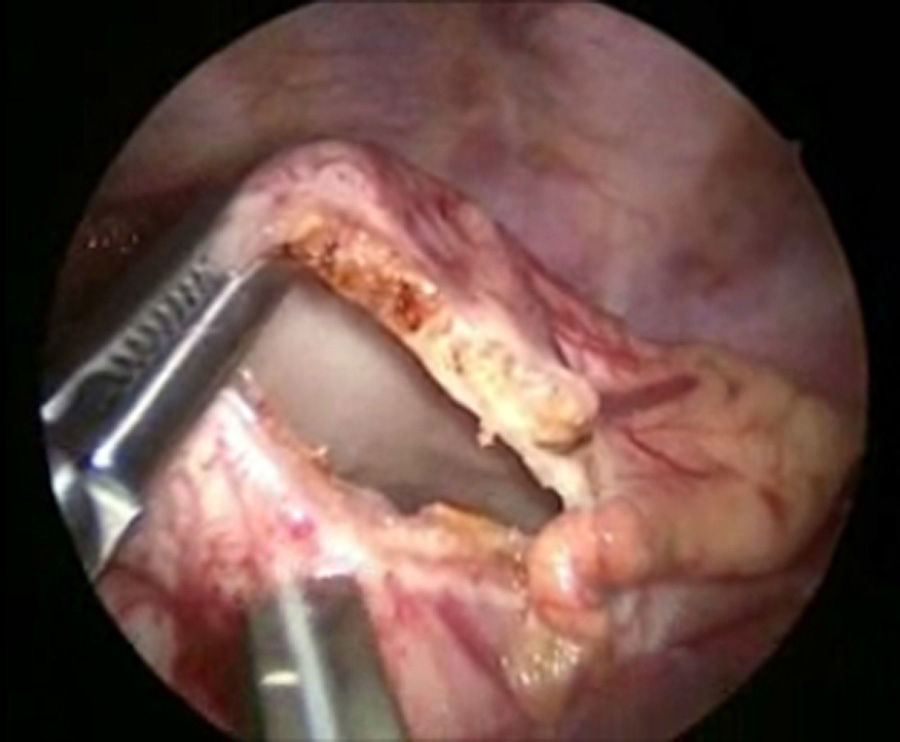
The patient underwent surgery using a right-sided thoracoscopic approach; with patient in the left lateral position, 3.5mm ports were inserted, the first 1cm below the scapula for the 30° optic and 5mm, insufflated at 5mm Hg, and flow at 1l/min. Then 2.5mm ports were inserted in the anterior axillary line in the 4th and 7th intercostal space. The initial exploration revealed a haematoma in the mediastinum (Fig. 4). The thoracic duct was dissected at its inlet to the chest, and 3 silk ligatures 2-0 were placed (fig. 5). Then 2.5mm ports were inserted in the posterior axillary line in the 4th and 7th intercostal space, the phrenic nerve was identified and above it the pericardium was incised, to create a window from the diaphragm to the union of the superior vena cava and the auricle and an enlarged pericardium was found (Fig. 6). A water seal chest drain was inserted, and the approaches were closed with 3 and 4-0 absorbable suture. Surgical time was 50min, without incident or complications.
A normal oral diet was started 24h post surgery, loss through the chest drain on the first post-operative day was 0.1ml/kg/h until practically nil after 72h, and therefore the drain was removed. The patient was discharged on the fourth postoperative day with no complications. Current follow-up is 12 months with no recurrence, with normal ultrasound and radiological monitoring.
DiscussionChylopericardium is a very rare disorder in children, which almost always presents after cardiovascular surgery or associated with lymphatic malformations or thoracic tumours.1–3,14–17 It is most likely that this case was associated with the traumatic event as this marked the onset of symptoms, for which a chest X-ray was necessary which revealed cardiomegaly, and because a haematoma was found in the upper part of the posterior mediastinum on thorascopic exploration. Regardless of the volume of accumulated fluid, and for some reason that we do not know, patients with this disorder can either have serious symptoms of tamponade or very few symptoms, as in the case we report here.1–3 This disorder's physiopathology of an accumulation of fluid in the pericardium1–6 and not in the pleural space is not well understood; it is believed that it might be a leak at the site where the thoracic duct enters the superior vena cava, and hence the build-up of chyle in the pericardial space. Once a diagnosis of chylopericardium has been made, and depending on the severity of symptoms, if the initial presentation is not severe medical treatment should be attempted, with fasting, parenteral nutrition, the use of diets with medium chain triglycerides and even the administration of drugs such as octreotide,15 which in some cases reduces the production of chyle. But if it remains raised or if rather than decreasing it increases, or if the initial symptoms are severe, as with tamponade, surgical treatment is necessary. There are various surgical options, which might be to establish a communication of the pericardium towards the peritoneum, inserting a Denver valve, or establishing a communication towards the pleura with a wide pericardial window, or thoracic duct ligation.1,5,10 We opted for the latter option, along with construction of a wide pericardial window, which was performed with minimal invasion. This alternative enabled the leakage of chyle to be controlled, and the patient recovered rapidly due to the advantages of minimally invasive surgery.
ConclusionDue to all of the above, we consider that thoracic duct ligation along with the creation of a pericardial window by thoracoscopy is a useful and safe alternative for the treatment of these patients.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: García-Hernández C, Carvajal-Figueroa L, Calderón-Urrieta A, Lechuga-Tosqui A, Landa-Juárez S. Tratamiento por mínima invasión del quilopericardio traumático. Reporte de un caso pediátrico. Cir Cir. 2016;84:45–49.