Autologous internal limiting membrane transplantation has allowed some cases of macular holes refractory to conventional surgery techniques to be treated.
The purpose of this study is to describe the anatomical and functional outcomes of a modification of this technique in a case series of naïve macular hole patients.
Material and methodsA consecutive case series study was performed on patients with naïve macular holes with a diameter greater than 600μm. Best corrected visual acuity, clinical features of the macular area, and optical coherence tomography were recorded before the operation and at the end of follow-up in all patients studied. All patients underwent 23Ga core vitrectomy, posterior hyaloid separation, and brilliant-blue assisted internal limiting membrane peeling. A small piece of the internal limiting membrane was peeled off to make a free flap, and this was transplanted and placed inside the macular hole under perfluorocarbon liquids. Air–fluid exchange was performed and SF6 gas was injected at a non-expansile concentration.
ResultsThe study included 5 eyes of 5 patients who underwent internal limiting membrane autograft. The mean age was 50.6 (SD 12.3) years. Four of the 5 cases had macular hole closure. The case where there was no closure of the macular hole was secondary to trauma. There was an improvement in visual acuity in all patients where the closing of the macular hole was achieved at the end of follow-up.
ConclusionsIn this cases series of macular hole patients, the autologous internal limiting membrane transplantation was associated with an anatomical closure of the macular hole and functional improvement in most of the patients studied.
El trasplante autólogo de membrana limitante interna ha permitido tratar algunos casos de agujero macular refractarios a las técnicas convencionales de cirugía.
El propósito de este estudio es describir los resultados anatomofuncionales en una serie de casos tratados mediante una variante de esta técnica quirúrgica.
Material y métodosEstudio de serie de casos consecutivos. Se incluyó a pacientes con agujero macular mayor de 600μ de diámetro sin intervención previa. Se realizó toma de capacidad visual, así como fotografías clínicas y tomografía de coherencia óptica preoperatorias y al final del seguimiento, en todos los pacientes estudiados. Previa vitrectomía calibre 23Ga, con separación de hialoides posterior y limitorrexis empleando azul brillante, se tomó un injerto de membrana de limitante interna y se manipuló desplazándolo bajo líquido perfluorocarbonado, hasta colocarlo dentro del agujero macular para finalmente realizar intercambio líquido-aire y colocación de gas SF6 a concentración no expansible.
ResultadosSe incluyeron 5 ojos de 5 pacientes tratados mediante el autoinjerto de membrana limitante interna. El promedio de edad fue de 50.6 (DE 12.3) años. En 4 de los 5 casos hubo cierre del agujero macular. El caso en donde no hubo cierre fue el secundario a trauma. Hubo mejoría de la capacidad visual en todos los pacientes en quienes se logró el cierre del agujero al final del seguimiento.
ConclusionesEn esta serie de casos de agujero macular, el trasplante autólogo de membrana limitante interna se asoció a un cierre anatómico del agujero macular y mejoría funcional en la mayoría de los pacientes incluidos.
Due to its anatomical and functional outcomes, in recent years macular hole surgery has become one of the most frequently performed vitreoretinal procedures. This is largely due to perfections in vitrectomy techniques, and the advent of small-gauge or minimally invasive surgery.1 Another factor which has had a favourable effect on surgical success is being able to more completely and safely remove the internal limiting membrane around the macular hole due to better visualisation. This is achieved in part with the application of the newly introduced vital stains such as brilliant blue. However, there are still cases that are refractory to conventional surgical techniques and that require alternatives in order to increase the already high rate of macular hole closure.3–9 One of these techniques is autologous transplantation of the internal limiting membrane as described by Morizane et al.,10 who show encouraging outcomes in their case series from both an anatomical and functional perspective.
ObjectiveTo describe a variant of the vitrectomy technique for autologous transplantation of the internal limiting membrane, for the treatment of macular hole, and the experience gained from a series of consecutive cases.
Material and methodsA prospective case series study was undertaken. All the patients were informed of the procedure and their informed consent obtained. The study was approved by the Ethics Committee of the Clínica David Ophthalmology Unit and was performed in line with the Helsinki Declaration guidelines.
The inclusion criteria were: patients with unilateral macular hole, with the presence of a macular hole of more than 600μm in diameter, who underwent 23Ga vitrectomy with autograft of internal limiting membrane and placement of SF6 at 10% as intraocular tamponade, along with a minimum follow-up period of 3 months post surgery. The elimination criteria were non-completion of follow-up or withdrawing from the study for any other reason.
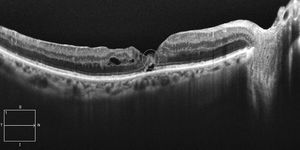
The patients underwent best corrected visual acuity with Snellen notation, subsequently converted to logMAR notation for statistical analysis. They also underwent a complete ophthalmological examination including clinical photography, and high definition spectral domain optical coherence tomography (Cirrus Carl Zeiss Meditec, Inc., Dublin, California, USA, preoperatively and at the end of follow-up).
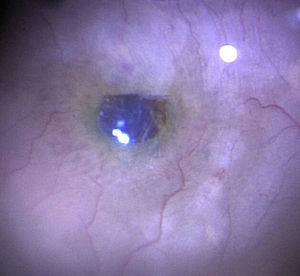
With regard to surgical technique, all the patients included in the study underwent minimally-invasive 23Ga vitrectomy, phacoemulsification and intraocular lens placement with placement of concomitant intraocular lens, after intraocular lens (power) calculation. Triamcinolone was used (ATLC, Laboratorios Grin, Mexico, D.F., Mexico) to impregnate the vitreous and facilitate its visualisation during the vitrectomy procedure. Brilliant-blue G (Brilliant Peel, Geuder, Heidelberg, Germany) was then placed directly on the macular area to stain the limiting membrane. A wide diameter limitorrhexis was performed and immediately afterwards a perfluorocarbon liquid bubble was placed (Perfluoron, Alcon, Fort Worth, Texas, USA).
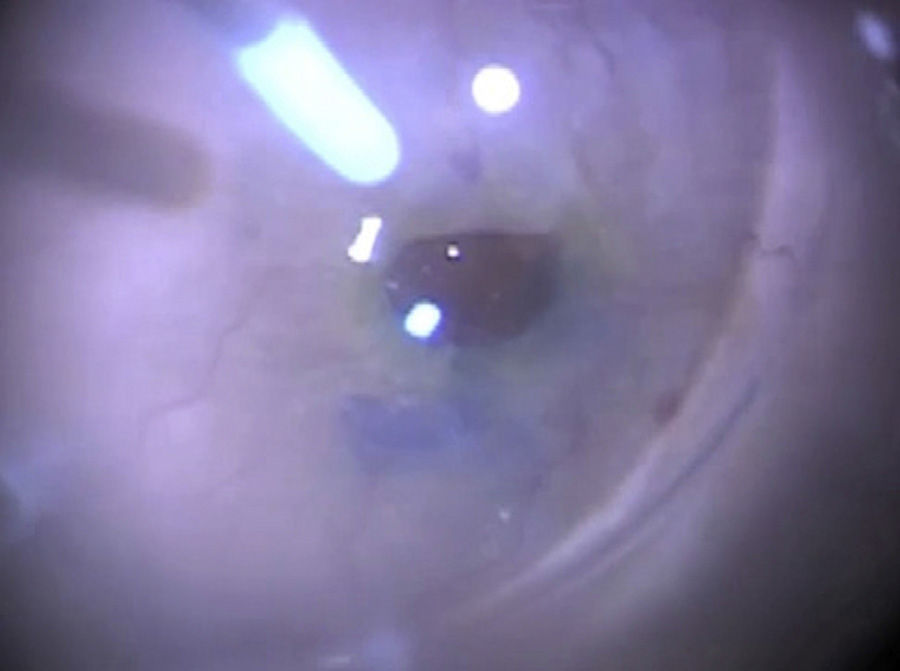
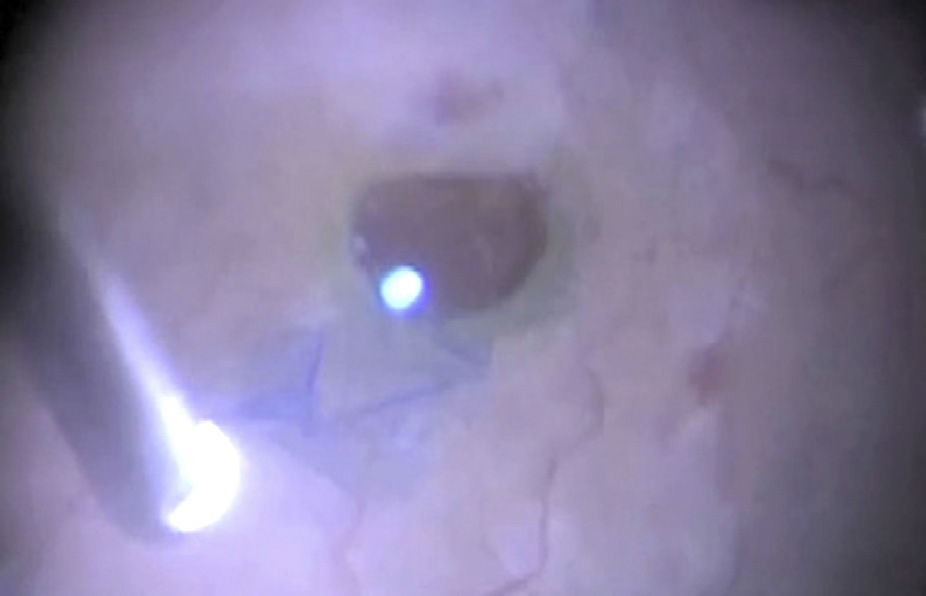
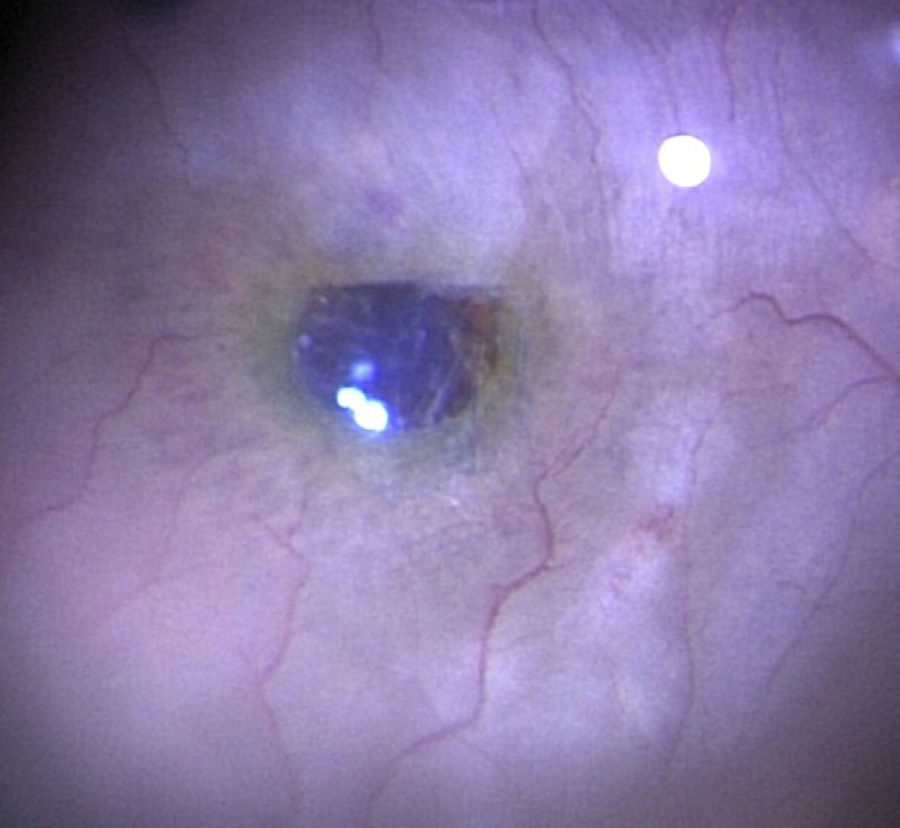
A small flap of internal limiting membrane was peeled off under the perfluorocarbon liquid bubble and dragged to place it inside the macular hole (Figs. 1 and 2). In other cases, the limiting membrane graft was not completely released from the edge of the hole so that it would serve as anchoring (Fig. 3) in order to prevent the graft being lost through the currents generated inside the vitreous cavity. Finally, complete air–fluid exchange was performed to maintain the graft inside the macular hole with surface tension.
A p value <0.05 was considered statistically significant in the statistical analysis. Mann–Whitney U test was used to compare pre and post-operative visual acuity, and SPSS for Windows version 17 (SPSS, Inc., Chicago, Illinois, USA) was the software package used.
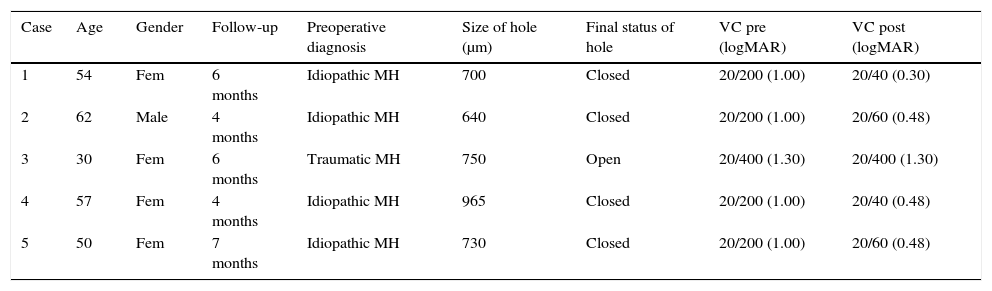
ResultsFive eyes of 5 patients were included. The patient features are shown in Table 1. The mean age of the patients was 50.6 years (SD 12.3), while the mean preoperative diameter of the macular holes was 757μm (SD 123.4).
Features and outcomes of the operated patients.
| Case | Age | Gender | Follow-up | Preoperative diagnosis | Size of hole (μm) | Final status of hole | VC pre (logMAR) | VC post (logMAR) |
|---|---|---|---|---|---|---|---|---|
| 1 | 54 | Fem | 6 months | Idiopathic MH | 700 | Closed | 20/200 (1.00) | 20/40 (0.30) |
| 2 | 62 | Male | 4 months | Idiopathic MH | 640 | Closed | 20/200 (1.00) | 20/60 (0.48) |
| 3 | 30 | Fem | 6 months | Traumatic MH | 750 | Open | 20/400 (1.30) | 20/400 (1.30) |
| 4 | 57 | Fem | 4 months | Idiopathic MH | 965 | Closed | 20/200 (1.00) | 20/40 (0.48) |
| 5 | 50 | Fem | 7 months | Idiopathic MH | 730 | Closed | 20/200 (1.00) | 20/60 (0.48) |
Fem: female; logMAR: logarithm of the minimum angle of resolution; MH: macular hole; VC post: postoperative visual capacity at the end of follow-up; VC pre: preoperative visual capacity.
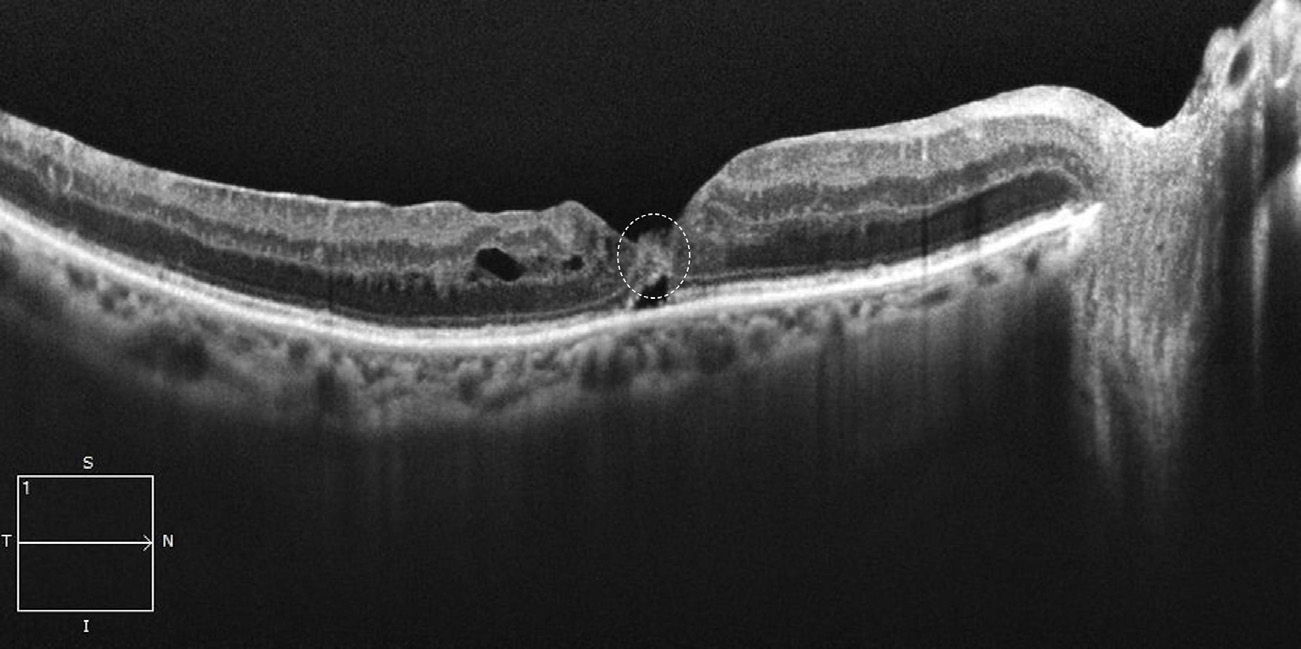
Closure of the macular hole was achieved in 4 out of the 5 patients included in the study (Fig. 4). The exception was the patient with a macular hole secondary to trauma. The change in visual acuity was not significant (p=0.669, Mann–Whitney U test).
DiscussionAccording to Gaudric and Tadayoni1 at the beginning of the nineties in the last century, Wendell and Kelly described their surgical technique for the treatment of macular hole, which represented a watershed in the approach to this disease.
However, some cases remain refractory to the conventional technique which has been refined over the years. Peeling of the internal limiting membrane and the advent of vital stains such as brilliant blue which enable complete visualisation of the internal limiting membrane, and consequently enormously facilitating separation of the retina,2 are outstanding amongst the advances that have resulted in increased anatomical success rates.
Many techniques have been described for refractory cases, including that of Alpatov et al.,8 who propose approaching the edges of the hole mechanically.
Authors such as Michalewska et al.3 have also developed a technique that consists of making a flap with the same limiting membrane to serve as a plug over the macular hole. This concept of peeling the limiting membrane to relieve the tangential traction it exercises on the retina and which is a major factor in the formation of the macular hole, in order to then use it as a “plug” or scaffolding over which the tissue that contributes to the formation of the hole grows, has recently been gaining in popularity. The group of Morizane et al.10 reported a case series where they took a free graft of the limiting membrane from the edge of the area where they had previously performed limitorrhexis and placed it in the macular hole, fixing it with viscoelastic material. They report a high closure rate (90%) which coincides with this study; although we had a lower closure rate in our study (80%).
One of the differences in technique as reported in the study by Morizane et al.10 is that in our study instead of using viscoelastic material to fix the limiting membrane graft, it was handled under perfluorocarbon liquid, displacing it towards the hole, or, in some cases, an end of the limiting membrane was not totally separated from the edge of the hole and served as an anchor, to then place it inside the macular hole as well, as mentioned in the section on material and methods. All of the above was carried out with a view to preventing the graft becoming lost in the currents generated inside the vitreous cavity. Another difference is that patients were included in our study that had not undergone any procedures to close their macular hole.
There was no significant improvement in visual acuity as was reported in Morizane's study,10 perhaps due to the less extensive follow-up of the patients in our case series. It has been reported that in many cases of macular hole surgery, visual capacity continues to improve, even many months after achieving closure of the hole.1
The study by Michalewska et al.3 that describes a variant of the limiting membrane autograft where it is used as an inverted flap over the hole, reports a closure rate of 88%. This figure is slightly higher than ours (80%), although the number of patients included in our study was very much lower (5 vs. 51 patients).
Furthermore, Kuriyama et al.4 achieve a closure rate that was exactly the same as ours (80%). It is important to highlight that Kuriyama's technique4 is similar to that of Michalewska,3 using an inverted limiting membrane flap.
It is interesting to highlight the fact that some nerve elements and fragments of Müller cells11 have been found in remains of the internal limiting membrane. Furthermore, it is indicated that these elements are necessary in many cases in order to produce a proliferation of fibroglial tissue, needed for the appropriate closure of the macular hole after vitrectomy.12 In this regard, internal limiting membrane autograft would provide an adequate amount of this tissue in the autograft itself. This is the case especially in very large holes with major atrophy at their edges.13–15 Macular holes with the latter features are considered to respond poorly to conventional surgical procedures.2
One of the limitations of this study lies in that it is a small case series and this type of study can be more prone to bias, such as statistical error type II; in other words, not finding any statistically significant differences between the variables studies when in reality they exist.
ConclusionsThis study demonstrates that it is possible to close a macular hole anatomically with functional improvement. Larger, randomised studies with a control group are required to establish the real role that this technique might play in the treatment of macular holes, especially in those cases that are refractory to conventional surgery.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestsThe authors have no conflict of interests to declare.
The authors would like to thank the staff at the Ophthalmology Unit of the Clínica David for their collaboration in gathering the case study information of all the patients included in this study.
Please cite this article as: Hernández-da Mota SE, Béjar-Cornejo F. Técnica modificada de trasplante autólogo de membrana limitante interna en agujero macular. Cir Cir. 2016;84:454–458.