Skin cancer treatment includes surgical and non-surgical techniques. Among surgical techniques, Mohs micrographic surgery permits a complete evaluation of surgical margins with maximal tissue sparing.
Material and methodsRetrospective review of dermatology database of skin cancer cases treated with Mohs surgery at University Hospital Dr. José Eleuterio González from 1988 to 2015.
ResultsA total of 546 cases were included, of these 289 (52.93%) corresponded to women and 257 (47.07%) to men. Mean age at presentation was 64.3. Most tumours (63.2%) corresponded to infiltrative basal cell carcinoma and the majority were located on the nose and cheek; 9.7% of cases corresponded to recurrent tumours. A mean of 1 Mohs stages was used in 56%, with a mean of 2 sections in 23.6%. Cutaneous flaps were used in 47.7%, representing the predominant reconstruction technique.
ConclusionMohs surgery has emerged in one of the dermatology reference centres in the North of the country as one of the surgical techniques for the treatment of aggressive carcinomas with high risk of recurrence.
La terapéutica del cáncer de piel incluye técnicas quirúrgicas y no quirúrgicas. Dentro de las quirúrgicas, la cirugía micrográfica de Mohs es la técnica mediante la cual se logra revisión completa de los márgenes quirúrgicos con máxima preservación del tejido.
Material y métodosRevisión retrospectiva en la base de datos de dermatología del Hospital Universitario Dr. José Eleuterio González de los casos de cáncer de piel tratados mediante cirugía micrográfica de Mohs de 1988 a 2015.
ResultadosSe encontraron 546 casos; de estos, 289 (52.93%) correspondieron a mujeres y 257 (47.07%) a hombres. La edad media de presentación fue 64.3 años. El 63.2% de tumores correspondió a carcinoma basocelular infiltrante y la mayoría de los casos se ubicaron en nariz y mejilla. El 9.7% eran casos correspondientes a recidivas de tratamientos previos. El 56% de los casos se trataron con un estadio de Mohs. En el 23.6% de los casos se requirieron 2 cortes durante la cirugía de Mohs. El tipo de reconstrucción del defecto posterior a cirugía de Mohs más frecuente fueron los colgajos cutáneos en el 47.4% de los casos.
ConclusiónLa cirugía de Mohs ha emergido en uno de los centros dermatológicos de referencia en el Norte del país como una opción terapéutica para carcinomas de estirpe agresiva con alto riesgo de recidiva local.
Micrographic Mohs surgery (MMS) may have a recovery rate of 99% for primary basal cell carcinoma (BCC) and 97% for primary squamous cell carcinoma (SCC).1
This surgical tool is based on the fact that skin cancer has a continuous growth with microscopic spread beyond clinically identifiable margins. Through removal of the tumour layer by layer and microscopic observation of the margins and surgical site, it is possible to completely remove the tumour.2 This sequential excision of the tumour tissue was designed by Frederick Mohs in 1932, who proposed a method for the fixing of tumour tissue with the use of zinc chloride that led to the preservation of the microscopic architectures of the tissue with subsequent location of the residual tumour, under the name of chemosurgery. After this, in 1970, Tromovitch changed the technique and in 1974, together with Stegman, published the results of follow up to 5 years in a series of 102 patients with BCC and SCC treated with this method, with a recovery rate of 97%. In 1985 the term was changed by the American College of Chemosurgery to MMS, using the fixed fresh tissue technique.2,3
MMS had high rates of recovery for local tumours, whilst minimising the removal of health tissues. The edges were outlined as the tumour was surgically removed in successive stages. The histological study of the three-dimensional edge of the extirpated tissue led to the need for location of the residual tumour for its subsequent excision and the tissue which was not affected to be preserved.3 The advantages of MMS over standard surgery are precise histological control, higher recovery rates, and maximum healthy tissue preservation.4
Indications for Mohs surgery are based on tumour size, histology, topography and prior treatments. With regards to topography, the skin is divided into 3 different areas, based on the risk of recurrence in each of them5:
- -
Zone H: “Mask area” of the face (central face, eyelids, eyebrows, periorbitary area, nose, lips, skin and vermilion, chin, jaw, pre and postauricular skin, temporal region, ears), genitals, hands and feet.
- -
Zone M: cheeks, forehead, hair on head, neck, and pretibial region.
- -
Zone L: trunk and extremities (excluding pretibial region, hands, feet, nails and heels).
Criteria for carrying out MMS are4:
- -
Non melanoma skin cancer (BCC and SCC) over 6mm in high risk areas (area H).
- -
Tumours over 1cm in the face (area M) or over 2cm in the trunk and extremities (area L).
- -
Recurrent tumours and/or incomplete excision.
- -
Tumours with aggressive histological subtypes or badly defined edges (infiltrative BCC, micronodular, morphoic, SCC and BCC with perineural or perivascular invasion).
- -
Tumours in locations with function or cosmetic compromise (genital, anal, hands and feet).
- -
Non melanoma skin cancer in immune-suppressed patients.
- -
Tumours originating in places of chronic inflammation (ulcers, burns, scars).
- -
Genetic conditions which predispose skin cancer (basal cell nevus syndrome, xeroderma pigmentoso and Muir-Torre syndrome).
Compared with the removal with margins in which the pathology makes horizontal, vertical or oblique cuts, where only revision close to 0.1% of the surgical margins is possible, in the MMS horizontal cuts are made with a 100% assessment of the surgical margins, giving place to higher rates of cure.2
MMS have been established as a therapeutic option of first choice in high risk non melanoma skin cancer (NMSC) in Europe, United States and Oceania. In Australia, a multicentre study between 1993 and 2002 reported the use of MMS for treatment of BCC in a 9 year period in 11,127 patients, where the predominant histological subtype was infiltrative (30.7%) and the majority of cases affected women (47%), in the head and neck (98.3%).6
This review aims at retrospective and demographic analysis of the NMSC cases treated with MMS in a dermatological centre in the North East of Mexico.
Material and methodsThe clinical medical files and Mohs surgery records of all patients with NMSC treated by MMS in the Dermatology Department of the University Hospital Dr. José Eleuterio González, Monterrey, Nuevo León, Mexico were studied, from November 1988 to November 2015. The information was collected retrospectively from a standardised data base from 1988 where data from patients who underwent surgery with MMS were collected prospectively. The following parameters were taken into considerations: age, gender, histopathological diagnosis of the tumour observed in the MMS, if the tumour was primary or relapse, location on the body, number of stages, incision made and type of reconstruction.
ResultsA total of 546 cases of NMSC were treated by MMS between November 1988 and November 2015, of which 289 (52.93%) corresponded to women and 257 (47.07%) to men.
Out of the total cases, 9.7% corresponded to recurrent tumours and the remaining 90.3% represented primary tumours. The average age of patients was 64.3 (range between 21 and 94 years of age).
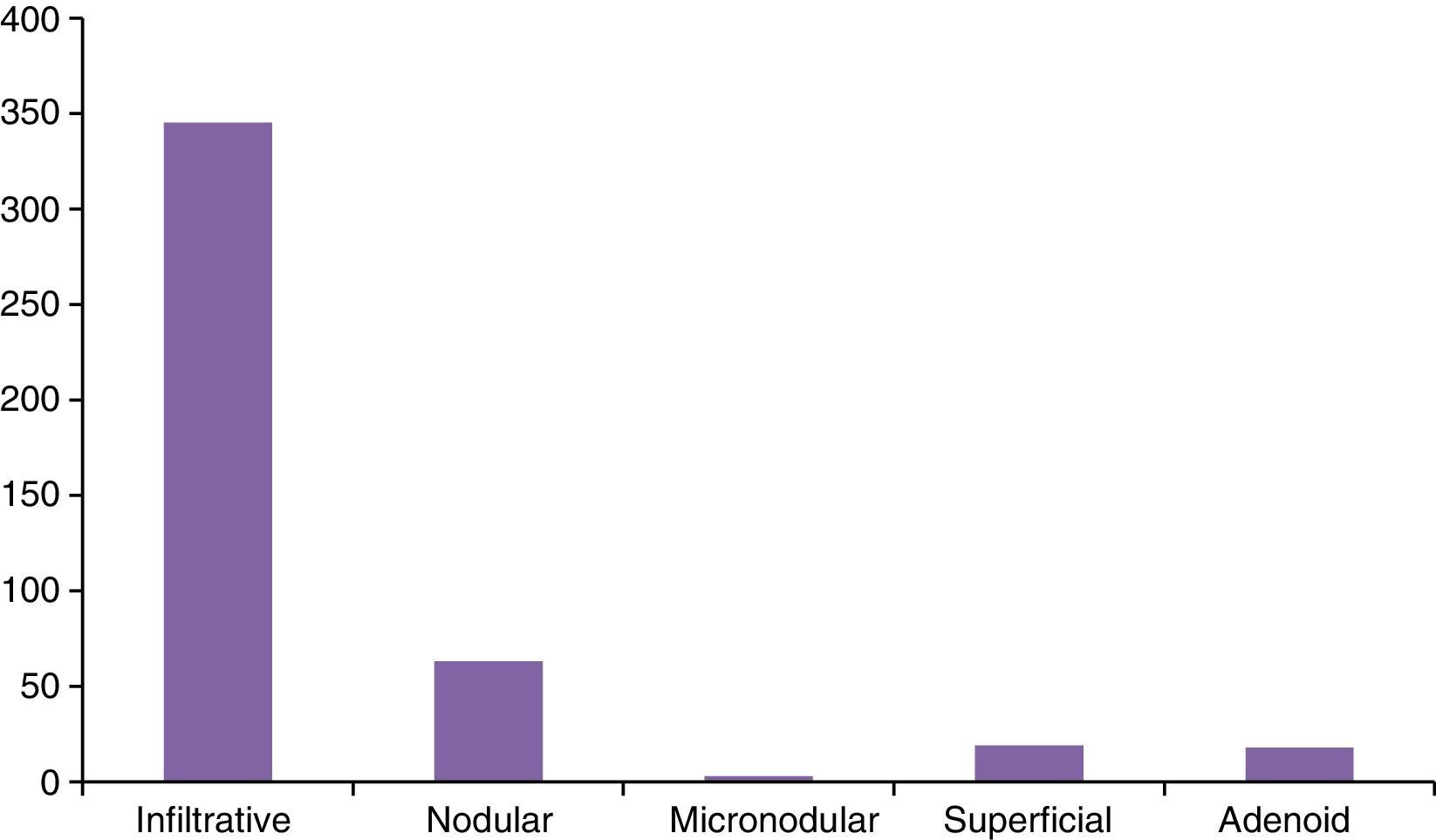
The most frequent histological subtype corresponded to the infiltrative BCC, with 345 (63.2%) cases, followed by nodular BCC, with 63 (11.5%) cases (Fig. 1). Fifty-five (10.0%) cases corresponded to SCC, of which 32 (5.9%) were well differentiated carcinomas, 21 (3.8%) moderately differentiated carcinomas and 2 (0.4%) badly differentiated.
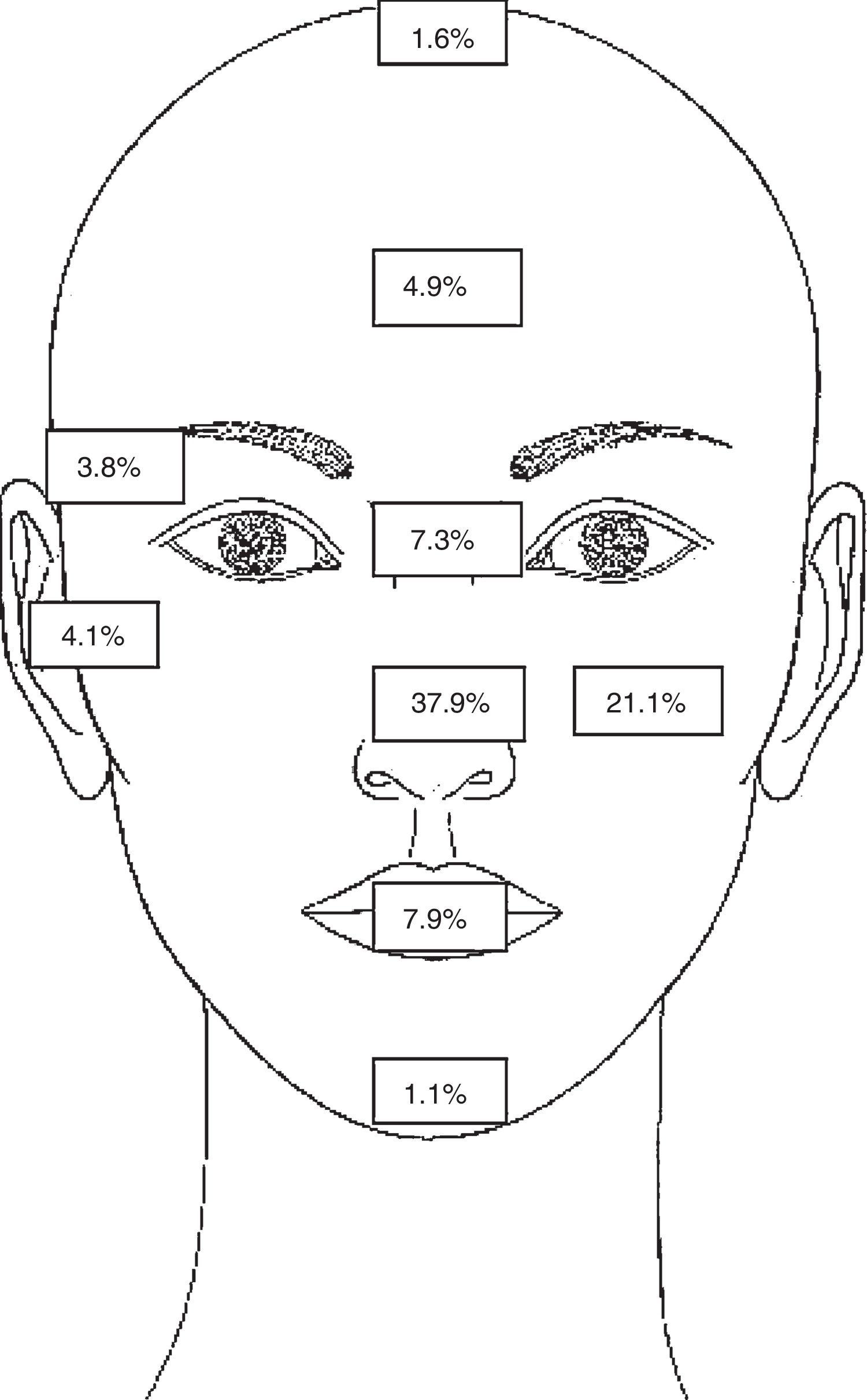
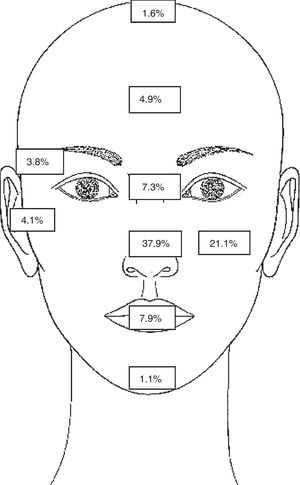
The predominant location in the cases analysed were the nose in 207 (37.9%) cases — tumour distribution was: dorsal nasal in 96 (46.3%) cases, nasal ala in 78 (37.6%) cases and tip of nose in 33 (15.9%) cases; in second place the cheek was the most commonly affected areas in 115 (21.1%) cases (Fig. 2).
They most common type of preoperative biopsy was punch biopsy in 89.1% of cases, followed by spindle cell biopsy 9.3% and shave biopsy in 0.18% of cases.
The number of studies required in each MMS was from 1 to 9. In the majority of cases 1or 2 studies were performed (56% and 32%, respectively). The number of incisions made in each surgical procedure was from 1 to 36. The number of most common incisions was from 2 in 128 cases (23.6%), followed by 4 in 102 cases (18.8%).
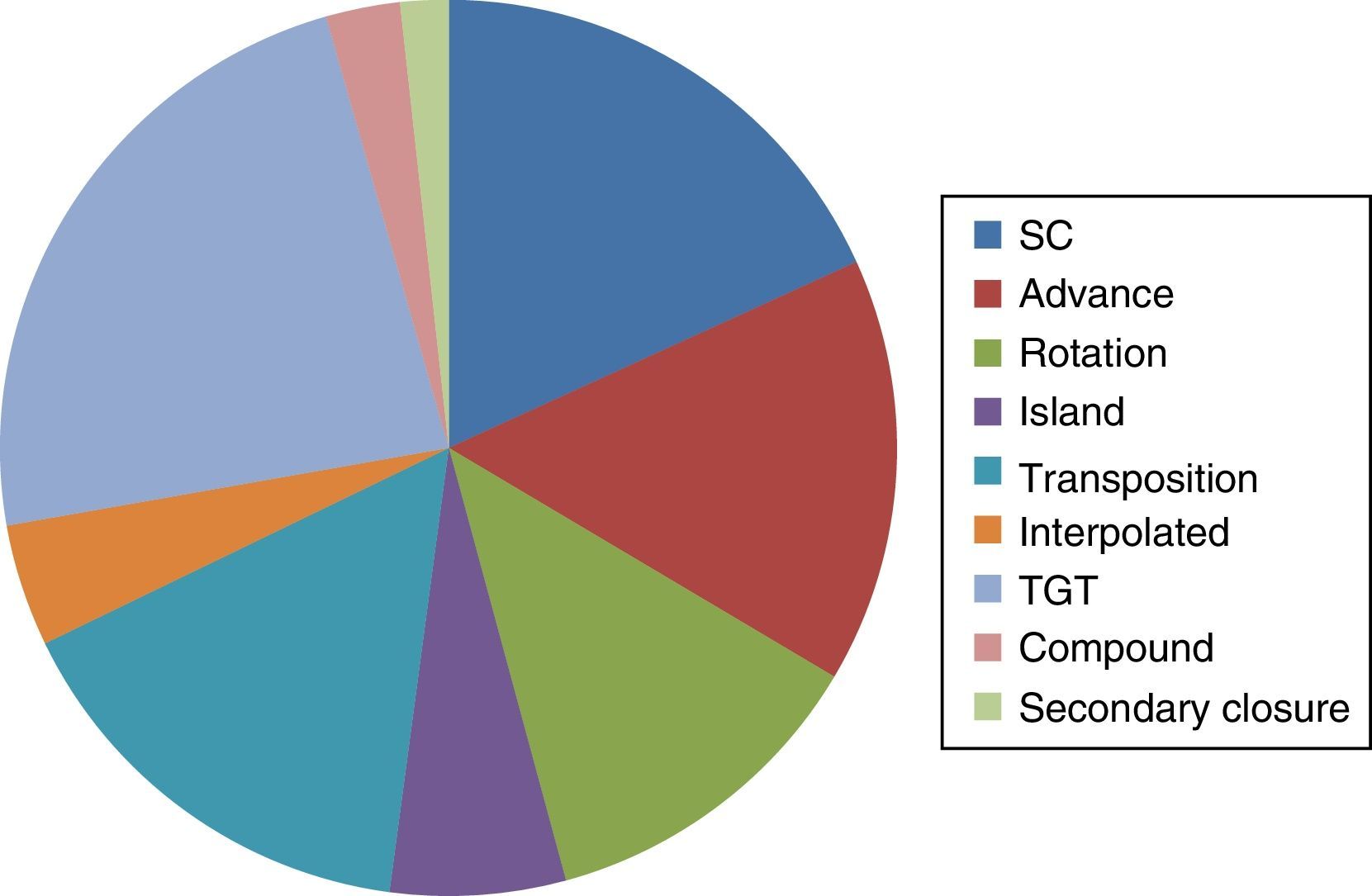
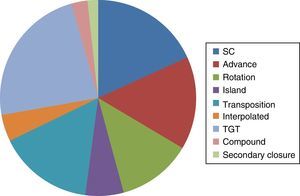
Reconstruction of the subsequent defects to removal of the tumour via MMS was carried out in the dermatological unit. The reconstruction techniques most commonly used included local flaps (advance, rotation, transposition and interpolated) in 259 (47.4%) cases, grafts of a total thickness in 122 (22.3%) cases, primary closure in 95 (17.3%) cases, and secondary closure in 9 (1.6%) cases, and other types of reconstruction (island and compound flaps) in 61 (11.1%) cases (Fig. 3).
From 2014 onwards we observed an increase in the number of MMS performed for NMSC. In 2008 there were 12 cases and in 2015 there were 92, which represented a substantial increase in the number of cases treated using this technique.
DiscussionNMSC is one of the most common reasons for consultation with the dermatologist. In Mexico there are several epidemiological data in the National Register of Neoplasms. In 1999, out of 90,605 malignant tumours, 13,361 corresponded to skin cancer (14.7%). In 2011 1454 deaths associated with melanoma and other malignant skin tumours were reported in Mexico.7 In 2010, in the Hospital Regional de Nuevo León del Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado (ISSSTE) a retrospective 10-year study was carried out which reported 591 patients diagnosed with skin cancer; BCC represented 65% of cases, followed by SCC, with 23%.8 In 2005 a 10-year retrospective study conducted in the Centro Dermatológico Pascua, in Mexico City reported 2320 patients with a confirmed diagnosis for malignant tumours. Out of these, 75% were BCC and 19%, were epidermoid carcinomas.9
There are few dermatological centres in Latin American which implement MMS for the treatment of NMSC. In Argentina, Galimberti et al.10 treated 2412 cases of BCC by MMS between October 2003 and June 2009. In Puerto Rico, in a comparative cohort study 38 patients were treated by MMS in 2000 and 55 in 2010.11 As far as we know there is no national register of MMS in Mexico and epidemiological data of cases treated through this technique are unknown, preventing the comparisons of our findings with previous national trends.
The increase in the number of MMS performed in the department of dermatology is much higher than that reported in other countries of Latin American in the last few years; Sosa et al.11 reported an increase of 44% in the number of cases treated with this technique between 2000 and 2010. This may be explained by the use of criteria for MMS. On the other hand, the increase in awareness campaigns for skin cancer has led to a greater number of people seeking dermatological healthcare.
The most common topography of NMSC in our study is for head and neck, the most areas most affected being: nose (37.9%) and cheek (21.1%). In the Galimberti et al.10 study the forehead and periorbitary region corresponded to the places found most frequently for BCC. The study by Sosa et al.11 however, reported predominance of tumours in the nose (52.3%) and cheek (13.16%).
In this study the histological subtype most commonly operated on using MMS corresponded to infiltrative BCC. This and the fact that the predominant topography corresponded to the H zone of the face, could reflect the implementation of criteria proposed by the national Institute of Cancer for the employment of MMS in our service.
The number of stages in MMS for prolonging free margins corresponded to 1% in the 56%. The average number of stages in the Galimberti et al.10 was 1.76, and was also 1 in the Sosa et al. study.11 This could be related to the early reference of tumours which were small despite the fact that in this study size was not reported. Moreover, use of local flaps as a predominant technique in this study reflects the decisive advances gained by dermatological surgery in the centres where it is carried out.
Our study limitations are associated with not having conducted the study in a single centre. The practice tendencies of this technique in the country are not reflected. However, they open the range of skin cancer treatment options up, especially for tumours with aggressive histological subtypes located in risk areas. This study reflects the need to introduce a national register to assess the use of this technique more objectively in other centres and to determine the behaviour of NMSC in Mexico.
ConclusionThis study describes the characteristics of the skin cancer cases treated with MMS. The follow-up of skin cancer treatment criteria is reflected in the selection of cases of aggressive histological origin and in topography which represents a high risk of relapse. The methodology of the technique used was based on the observation of 100% surgical margins in-depth and on the surface. This procedure ensures maximum complete tumour extirpation and favours maximum preservation of tissue, which optimises the posterior reconstruction of the surgical defect.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Cortés-Peralta EC, Garza-Rodríguez V, Vázquez-Martínez OT, Gutiérrez-Villarreal IM, Ocampo-Candiani J. Cirugía micrográfica de Mohs: 27 años de experiencia en el Noreste de México. Cir Cir. 2017;85:279–283.