Central nervous system tumours comprise a heterogeneous group of neoplasms with great histological diversity. Despite the rising prevalence of these tumours in developing countries, some places like Mexico and Latin America have no representative studies that show the real impact of these tumours in our population.
ObjectiveTo describe the characteristics of the primary and secondary tumours of the central nervous system in the last 20 years in a Mexican institution.
Material and methodsPatients with histopathological diagnosis from 1993 to 2013 in our institution, grouping them according to WHO classification 2007, characterising them by age group, gender, and anatomical location.
ResultsThere were a total of 511 tumours of the central nervous system. Of those, 292 were women and 219 men, with a ratio 1.3:1, and a mean age of 49.3 years. Tumours with higher prevalence were: meningeal tumours, 171 (33%), followed by neuroepithelial, 121 (24%). Astrocytoma had the highest prevalence in paediatric patients, whereas in those older than 20 years it was the meningioma. The supratentorial location was the most involved.
ConclusionThis is the first study of a series of cases in Mexico that is performed by taking into account benign and malignant tumours of the central nervous system, with patients of all age groups with a range of 20 years. While this work only represents a retrospective analysis of an institution, it can be a strong indication of the epidemiology of these tumours in our environment.
Los tumores del sistema nervioso central comprenden un grupo heterogéneo de neoplasias de gran diversidad histológica. Pese a la creciente prevalencia de estas neoplasias en los países en vías de desarrollo, existen pocos trabajos hoy en día, tanto en México como en Latinoamérica, que muestren la realidad de estos en nuestra población.
ObjetivoDescribir las características de los tumores primarios y secundarios de sistema nervioso central en los últimos 20 años en una institución mexicana.
Material y métodosPacientes con diagnóstico histopatológico de neoplasia de sistema nervioso central del año 1993 al 2013 en nuestra institución, agrupándolos conforme a la clasificación de la OMS 2007, es decir, por la caracterización del grupo etario, sexo y localización anatómica.
ResultadosSe presentaron un total de 511: 292 mujeres y 219 hombres con una razón 1.3: 1, con una media de edad de 49.3 años. Los tumores con mayor prevalencia fueron los de meninges 171 (33%), seguido por los neuroepiteliales 121 (24%). En pacientes pediátricos, el astrocitoma fue el tumor más prevalente, mientras que en mayores de 20 años fue el meningioma; la localización supratentorial fue la de mayor involucro.
ConclusiónEsta es la primera serie de casos en México de tumores malignos y benignos del sistema nervioso central que incluye a pacientes de todas las edades, y se realizó en un lapso de 20 años. Si bien este trabajo representa únicamente el análisis retrospectivo de una institución, puede ser un indicio importante de la epidemiología de estos tumores en nuestro medio.
Central nervous system tumours are a heterogeneous group of neoplasms of great histological diversity and are confined to the brain, spinal cord, meninges, cranial and paraspinal nerves.1,2 Large series have been undertaken by different groups throughout the world in order to establish the clinical and epidemiological features. In these studies we can observe that there has been a major increase in recent decades, especially in non-industrialised countries like Mexico.2–4 In 2002, the International Agency for Research on Cancer reported an incidence of 6.3 per 100,000 people in developed countries and 9.9 per 100,000 in developing countries.5 In some series these tumours are the primary cause of cancer-related death in children and highlight that more than 50% of paediatric brain tumour survivors present cognitive function deficits related to the tumour or its treatment.6 Therefore it is important to establish the current features of these tumours in our environment. However, in Mexico as in the majority of Latin American countries, there are few specialist epidemiological registers devoted to this area, and therefore it is important to promote, update, strengthen and continue to provide studies on the behaviour of central nervous system tumours in order to achieve greater scope and impact on public health, with early diagnosis and appropriate treatment towards improving survival and potential subsequent sequelae.
In light of the above, our team's aim in this study is to report the presentation of malignant and non-malignant tumours of the central nervous system in our institution over the past 20 years (1993–2013).
Materials and methodsAn observational, descriptive study, in patients with central nervous system tumours which were treated electively by neurosurgical resection with subsequent diagnosis by histopathological study in the Hospital Español of Mexico city, over a period of 20 years from 1 January 1993 to 31 December 2013.
The study variables were qualitative (histological group, gender, anatomic site affected) and quantitative (age).
Both the group and the histological diagnoses were formed in line with the World Health Organisation's (WHO) 2007 classification of nervous system tumours. In accordance with this classification the patients were divided into 7 groups: neuroepithelial tumours, cranial nerve and paraspinal tumours, tumours arising in the meninges, lymphomas and haematopoietic neoplasms, germinal cell tumours, sellar region and metastatic tumours. We then classified the subgroups by morphological variety.
From January 1993 to July 1997 it was not possible to obtain the patients’ ages, therefore a total of 77 cases were excluded when this variable was analysed. Similarly, we were not able to confirm the anatomic site affected for the total 511 patients; therefore we report a number of 429 under this heading.
This study was performed after approval from the Ethics and Research Committee of the Hospital Español.
Using descriptive statistics, a descriptive analysis was made of frequency, percentage and measures of central tendency. The statistical software package SPSS version 20 for Windows was used.
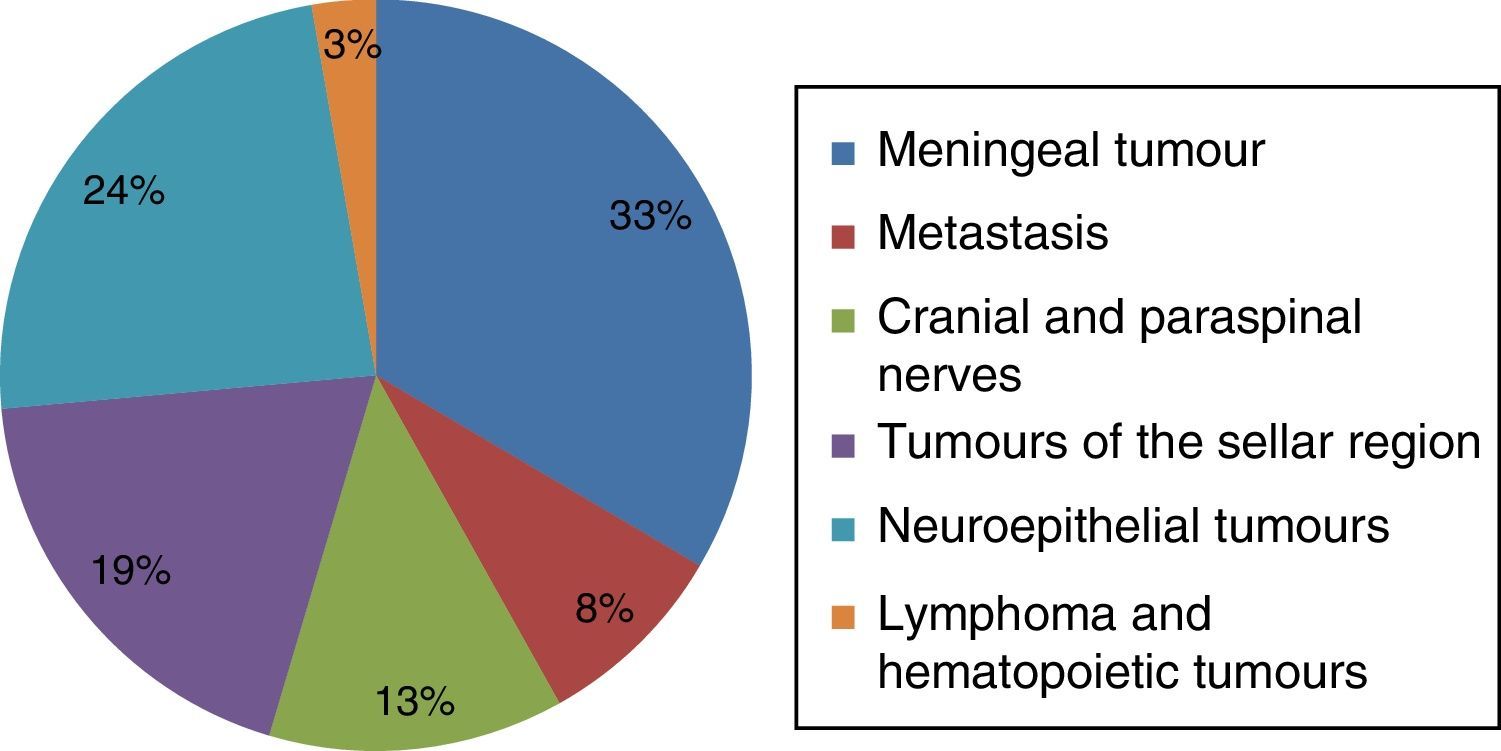
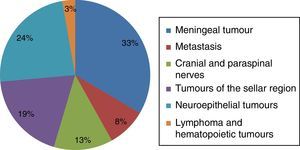
ResultsDuring the period under study, 511 tumours of the central nervous system were diagnosed. The meninges tumour group comprised 33%, followed by neuroepithelial tumours at 24%, tumours of the sellar region 19%, cranial and paraspinal nerve tumours 13%, metastasis 8%, and finally lymphoma and haematopoietic tumours 3% (Fig. 1). A total of 292 cases were female and 219 male, with a mean age of 49.3 years.
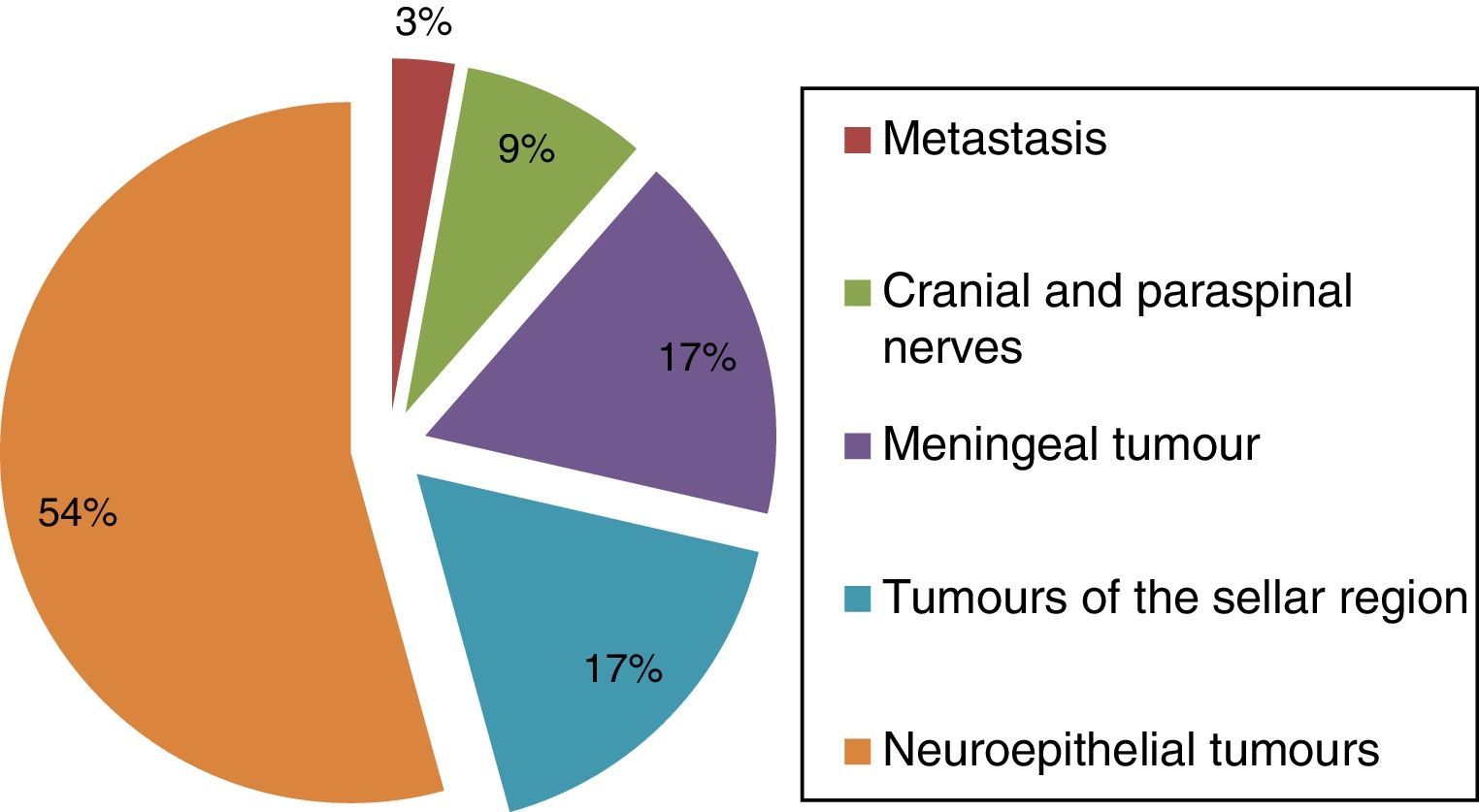
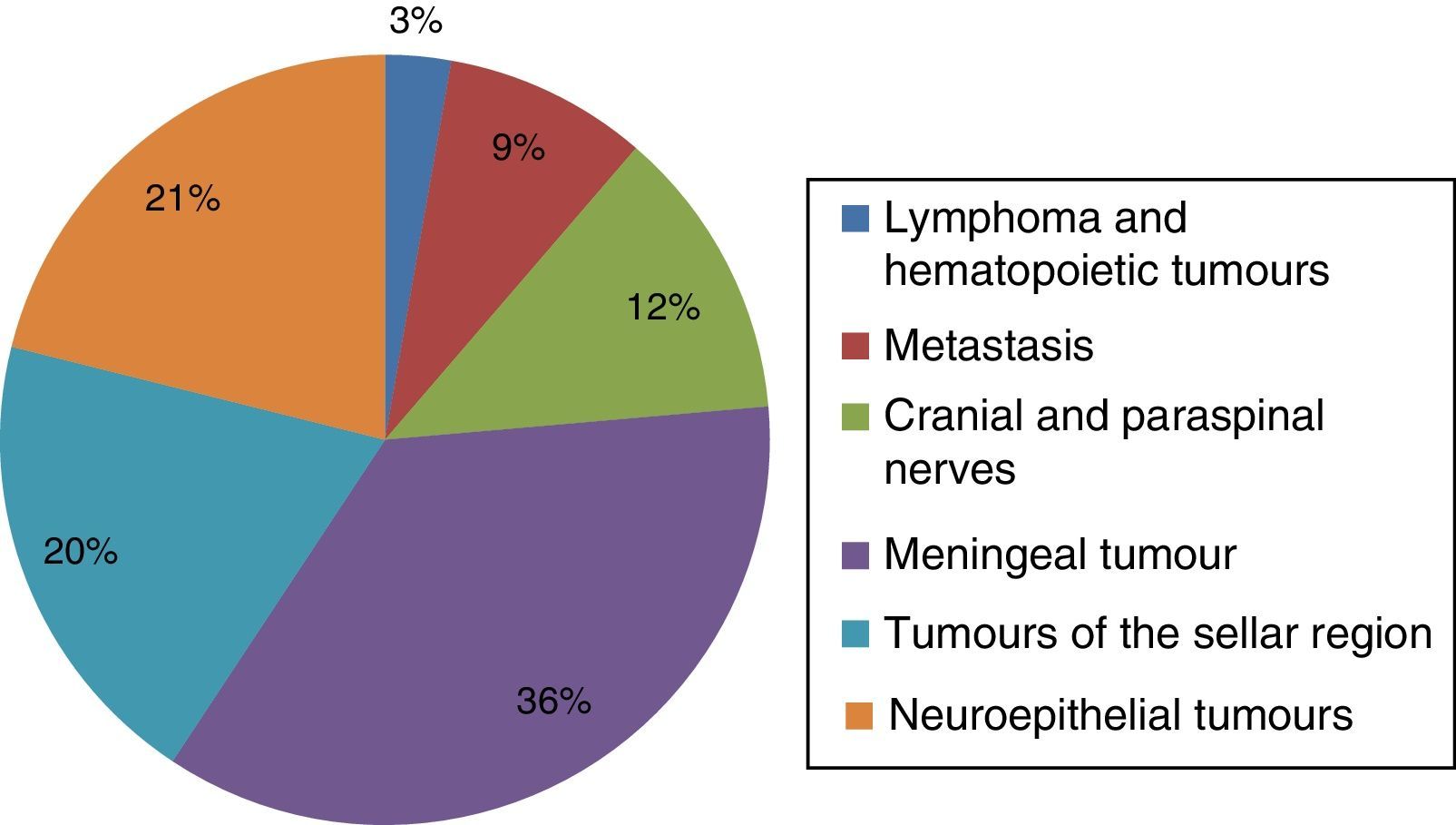
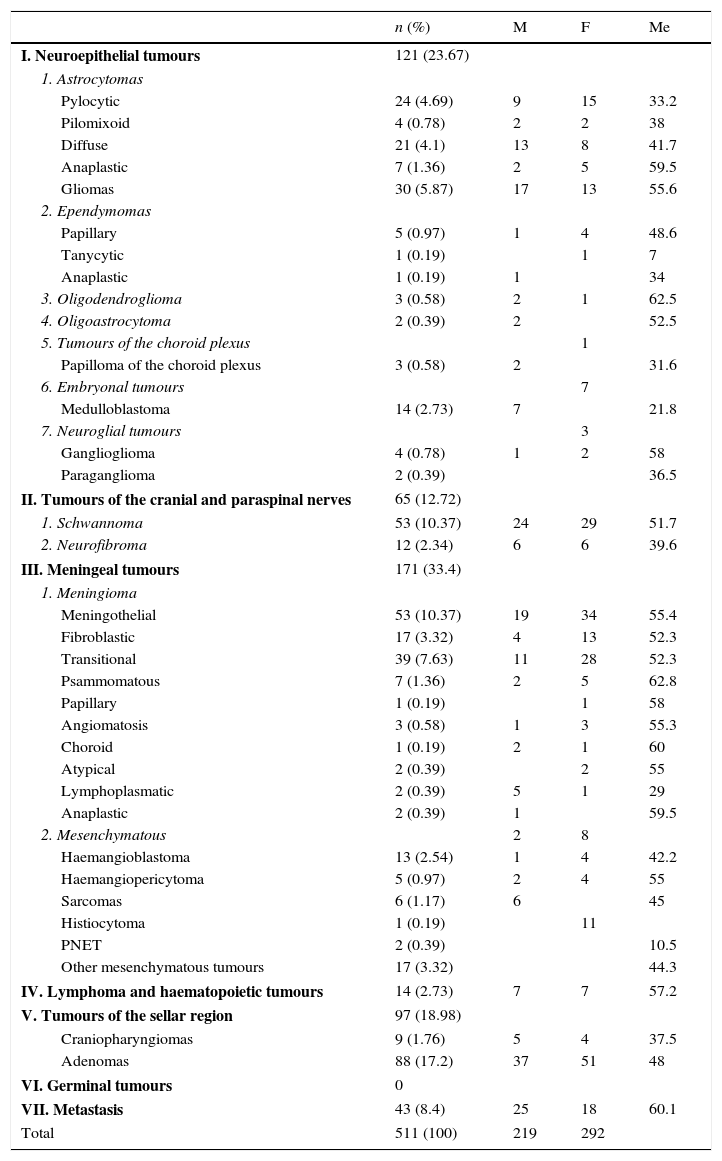
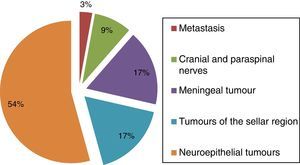
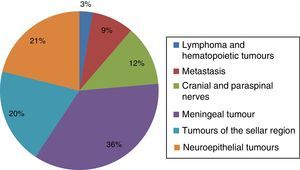
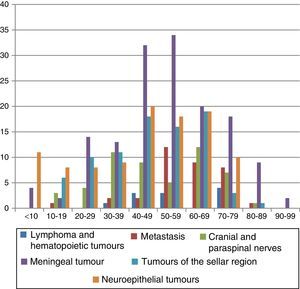
In patients under 19 years of age, the most prevalent tumour was astrocytoma, then neuroblastoma. We observed that the most frequent tumour was meningioma, followed by astrocytoma in the patients aged over 20. The details can be seen in Figs. 2 and 3. Meningioma represented 74% of the meninges tumour group; the remainder were mesenchymatous tumours. Astrocytoma made up 48% and multiform gliobastoma 24% of the neuroepithelial tumours. Within the group of sellar region tumours, hypophysary adenomas were most prevalent at 91% (Table 1, Fig. 4).
Histological features of 511 cases with central nervous system neoplasms over 20 years of experience.
| n (%) | M | F | Me | |
|---|---|---|---|---|
| I. Neuroepithelial tumours | 121 (23.67) | |||
| 1. Astrocytomas | ||||
| Pylocytic | 24 (4.69) | 9 | 15 | 33.2 |
| Pilomixoid | 4 (0.78) | 2 | 2 | 38 |
| Diffuse | 21 (4.1) | 13 | 8 | 41.7 |
| Anaplastic | 7 (1.36) | 2 | 5 | 59.5 |
| Gliomas | 30 (5.87) | 17 | 13 | 55.6 |
| 2. Ependymomas | ||||
| Papillary | 5 (0.97) | 1 | 4 | 48.6 |
| Tanycytic | 1 (0.19) | 1 | 7 | |
| Anaplastic | 1 (0.19) | 1 | 34 | |
| 3. Oligodendroglioma | 3 (0.58) | 2 | 1 | 62.5 |
| 4. Oligoastrocytoma | 2 (0.39) | 2 | 52.5 | |
| 5. Tumours of the choroid plexus | 1 | |||
| Papilloma of the choroid plexus | 3 (0.58) | 2 | 31.6 | |
| 6. Embryonal tumours | 7 | |||
| Medulloblastoma | 14 (2.73) | 7 | 21.8 | |
| 7. Neuroglial tumours | 3 | |||
| Ganglioglioma | 4 (0.78) | 1 | 2 | 58 |
| Paraganglioma | 2 (0.39) | 36.5 | ||
| II. Tumours of the cranial and paraspinal nerves | 65 (12.72) | |||
| 1. Schwannoma | 53 (10.37) | 24 | 29 | 51.7 |
| 2. Neurofibroma | 12 (2.34) | 6 | 6 | 39.6 |
| III. Meningeal tumours | 171 (33.4) | |||
| 1. Meningioma | ||||
| Meningothelial | 53 (10.37) | 19 | 34 | 55.4 |
| Fibroblastic | 17 (3.32) | 4 | 13 | 52.3 |
| Transitional | 39 (7.63) | 11 | 28 | 52.3 |
| Psammomatous | 7 (1.36) | 2 | 5 | 62.8 |
| Papillary | 1 (0.19) | 1 | 58 | |
| Angiomatosis | 3 (0.58) | 1 | 3 | 55.3 |
| Choroid | 1 (0.19) | 2 | 1 | 60 |
| Atypical | 2 (0.39) | 2 | 55 | |
| Lymphoplasmatic | 2 (0.39) | 5 | 1 | 29 |
| Anaplastic | 2 (0.39) | 1 | 59.5 | |
| 2. Mesenchymatous | 2 | 8 | ||
| Haemangioblastoma | 13 (2.54) | 1 | 4 | 42.2 |
| Haemangiopericytoma | 5 (0.97) | 2 | 4 | 55 |
| Sarcomas | 6 (1.17) | 6 | 45 | |
| Histiocytoma | 1 (0.19) | 11 | ||
| PNET | 2 (0.39) | 10.5 | ||
| Other mesenchymatous tumours | 17 (3.32) | 44.3 | ||
| IV. Lymphoma and haematopoietic tumours | 14 (2.73) | 7 | 7 | 57.2 |
| V. Tumours of the sellar region | 97 (18.98) | |||
| Craniopharyngiomas | 9 (1.76) | 5 | 4 | 37.5 |
| Adenomas | 88 (17.2) | 37 | 51 | 48 |
| VI. Germinal tumours | 0 | |||
| VII. Metastasis | 43 (8.4) | 25 | 18 | 60.1 |
| Total | 511 (100) | 219 | 292 | |
M: male; F: female; Me: mean; n: number.
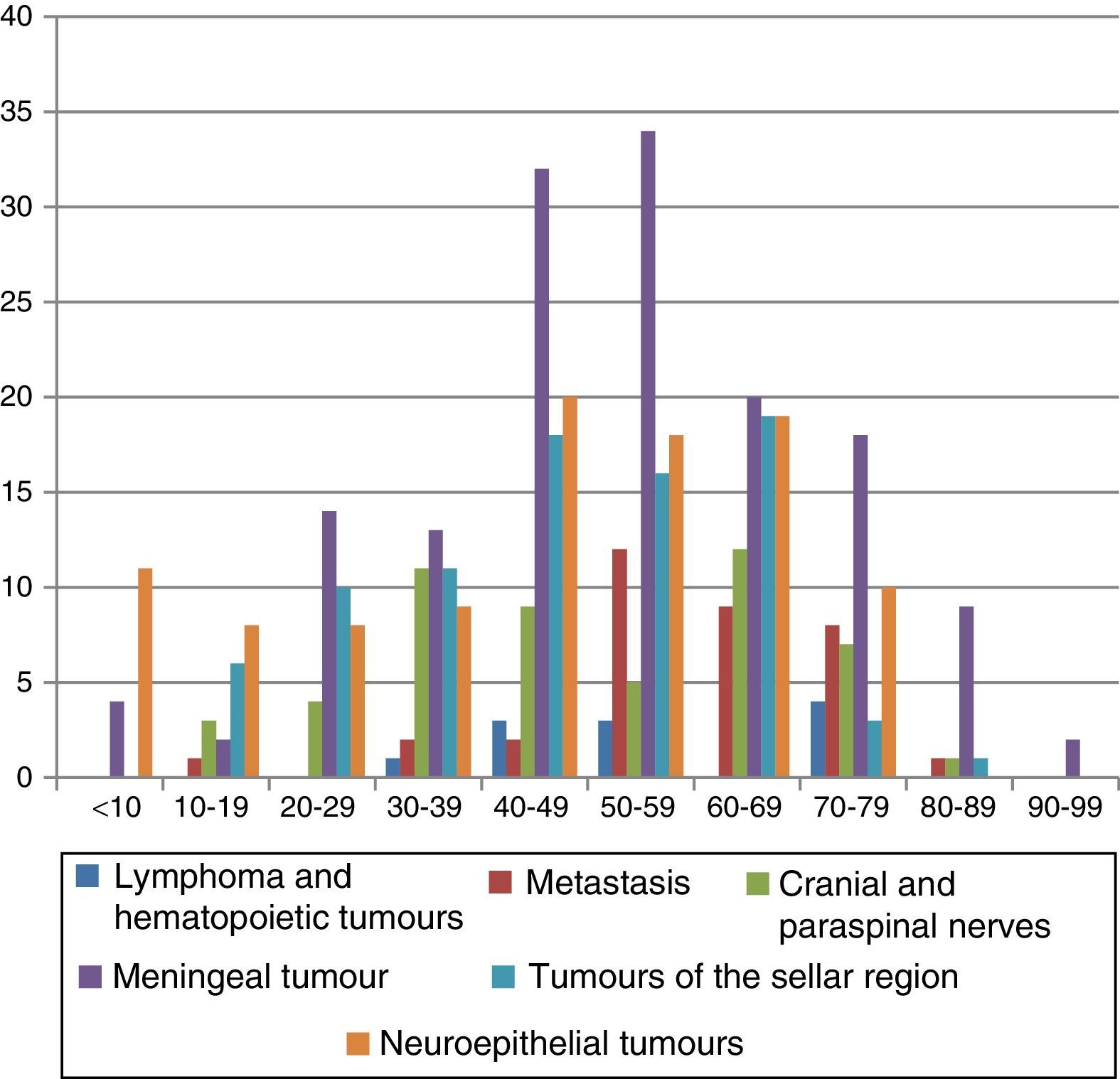
Tumours of the meninges presented in all groups, with a peak in patients aged from 40 to 60 years. Tumours of the neuroepithelium showed a first peak in the first 2 decades of life and a second in patients aged from 40 to 70 years (Fig. 4). Central nervous system tumours were more common in women than men at a ratio of 1.3:1. Very similar behaviour was observed in the different histological groups at a ratio of 1:1 in neuroepithelial tumours and tumours of the central nervous system. The male to female ratio in tumours of the meninges was 2:1; greater prevalence in males was only observed with metastases.
With regard to age group, there was greater prevalence in patients aged between 40 and 60 years. Males in the third decade of life were more affected; there is a clear female predominance in the remaining age groups.
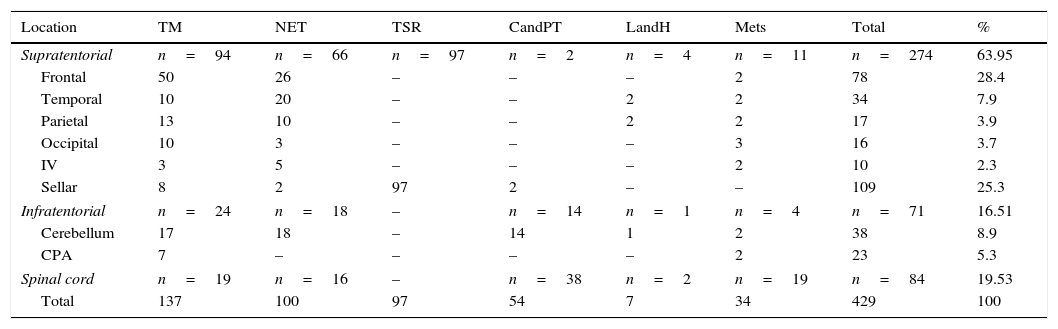
Anatomic location and histologyThe supratentorial region was the most affected area; the majority of the tumours were located in the frontal lobe (Table 2). Seventy-one point seven percent of the tumours of the meninges and 66.6% of the neuroepithelial tumours were located supratentorially. The tumours that presented most frequently supratentorially were tumours of the meninges, the neuroepithelium and the cranial and paraspinal nerves, representing 16.5% of the tumours. Medullary involvement was observed in 19.5% of tumours, where neurinoma clearly predominated, followed by metastasis. Table 2 shows the distribution of cases by histological diagnosis in the anatomic region affected.
Anatomic involvement according to the different histological group.
| Location | TM | NET | TSR | CandPT | LandH | Mets | Total | % |
|---|---|---|---|---|---|---|---|---|
| Supratentorial | n=94 | n=66 | n=97 | n=2 | n=4 | n=11 | n=274 | 63.95 |
| Frontal | 50 | 26 | – | – | – | 2 | 78 | 28.4 |
| Temporal | 10 | 20 | – | – | 2 | 2 | 34 | 7.9 |
| Parietal | 13 | 10 | – | – | 2 | 2 | 17 | 3.9 |
| Occipital | 10 | 3 | – | – | – | 3 | 16 | 3.7 |
| IV | 3 | 5 | – | – | – | 2 | 10 | 2.3 |
| Sellar | 8 | 2 | 97 | 2 | – | – | 109 | 25.3 |
| Infratentorial | n=24 | n=18 | – | n=14 | n=1 | n=4 | n=71 | 16.51 |
| Cerebellum | 17 | 18 | – | 14 | 1 | 2 | 38 | 8.9 |
| CPA | 7 | – | – | – | – | 2 | 23 | 5.3 |
| Spinal cord | n=19 | n=16 | – | n=38 | n=2 | n=19 | n=84 | 19.53 |
| Total | 137 | 100 | 97 | 54 | 7 | 34 | 429 | 100 |
CPA: cerebellopontine angle; IV: intraventricular; LandH: lymphomas and haematopoietic tumours; Mets: metastasis; n: number; CandPT: cranial nerve and paraspinal tumours; MT: meningeal tumours; NET: neuroepithelial tumours; TSR: tumours of the sellar region.
Central nervous system tumours are one of the principal neoplasms in children and in adults it is one of the most frequent reasons for consulting the Neurosurgery Services. Survival can be as poor as 26% at 5 years for tumours of the posterior fossa and 7% when the brain stem is affected.7–9 Neurocognitive sequelae are another great concern, due to the primarily neurosurgical management and the neurotoxicity of chemo and radiotherapy.10,11
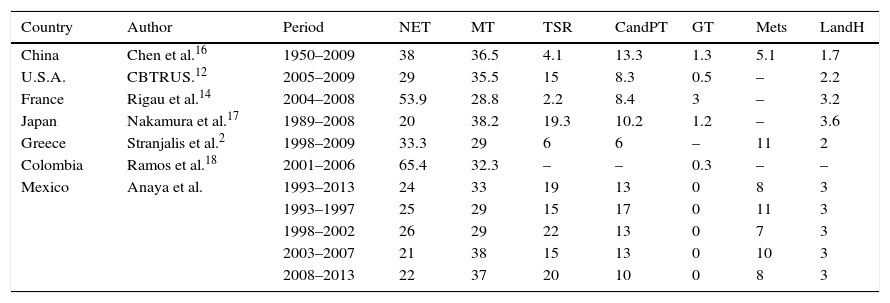
The series reported in Mexico focus either specifically on paediatric or on adult patients, with no publications on a sample that combines both. Studies of different groups that contain large adult populations report differences in terms of histological group and most prevalent tumour; in the United States’ series, tumours of the meninges are more frequent, at 35.5%.12,13 Neuroepithelial tumours are more prevalent in the European series, at 53.9% in France and 33.3% in Greece. In Asia, in the series from China, neuroepithelial tumours represent 38% and tumours of the meninges 36.5%. In Japan, Nakamura et al.17 report a clear prevalence of tumours of the meninges at 38.2%.2,14–17 The only report from Latin America was the study by Ramos Clason et al.18 performed in Colombia, reviewing a total of 390 cases, in which tumours of the meninges were the most prevalent at 50% (Table 3). It is important to mention, and it should be taken into account, that there are differences in the methodology used in each of the different studies, that a few series reported both primary and secondary tumours and that the study period is another important variable, as well as the number of centres participating in each study.
International series on prevalence of central nervous system tumours.
| Country | Author | Period | NET | MT | TSR | CandPT | GT | Mets | LandH |
|---|---|---|---|---|---|---|---|---|---|
| China | Chen et al.16 | 1950–2009 | 38 | 36.5 | 4.1 | 13.3 | 1.3 | 5.1 | 1.7 |
| U.S.A. | CBTRUS.12 | 2005–2009 | 29 | 35.5 | 15 | 8.3 | 0.5 | – | 2.2 |
| France | Rigau et al.14 | 2004–2008 | 53.9 | 28.8 | 2.2 | 8.4 | 3 | – | 3.2 |
| Japan | Nakamura et al.17 | 1989–2008 | 20 | 38.2 | 19.3 | 10.2 | 1.2 | – | 3.6 |
| Greece | Stranjalis et al.2 | 1998–2009 | 33.3 | 29 | 6 | 6 | – | 11 | 2 |
| Colombia | Ramos et al.18 | 2001–2006 | 65.4 | 32.3 | – | – | 0.3 | – | – |
| Mexico | Anaya et al. | 1993–2013 | 24 | 33 | 19 | 13 | 0 | 8 | 3 |
| 1993–1997 | 25 | 29 | 15 | 17 | 0 | 11 | 3 | ||
| 1998–2002 | 26 | 29 | 22 | 13 | 0 | 7 | 3 | ||
| 2003–2007 | 21 | 38 | 15 | 13 | 0 | 10 | 3 | ||
| 2008–2013 | 22 | 37 | 20 | 10 | 0 | 8 | 3 |
Data in percentage.
CPA: cerebellopontine angle; IV: intraventricular; LandH: lymphomas and haematopoietic tumours; Mets: metastasis; n: number; CandPT: cranial nerve and paraspinal tumours; GT: germinal tumours MT: meningeal tumours; NET: neuroepithelial tumours; TSR: tumours of the sellar region.
In Mexican paediatric patients, Chico Ponce et al.19 observed that the male gender, at 55%, was most affected and astrocytoma and meduloblastoma represent 50% of the tumours, and the infratentorial presentation predominated. Torre Mondragón et al.20 report very similar results, with the difference that the tumours presented at supratentorial level in 70% of children aged under 2 years. Intracranial tumours, as mentioned above, represent more than 50% of the neoplasms, in the great majority located in the posterior fossa; we observed this same behaviour when we undertook this study. A lesser percentage of paediatric tumours were confined to the sellar region (craniopharyngioma) and at interventricular level (ependymoma and choroid plexus papilloma).21
Intracranial tumours occur in adults with localised or multilobular involvement. High grade glioma is most frequent of the latter. In this study, involvement of the frontal lobe was the most frequent, which presented a behaviour similar to that published by Zada et al.22 in their study of patients with glioma, where they observed that the glioma most frequently involved the frontal lobe, followed by the temporal lobe. Meningeal neoplasms affect the cerebral convexity most often, compromising the frontal and parietal lobes. Matutes Fabelo et al.23 report that 79.7% presented supratentorially; we found that 71.7% affected this area. The base of the skull is characterised by neurinoma which arises from the cranial nerves. Some reviews mention it as the most frequent tumour of the cerebellopontine angle at up to 90%24,25; it represented 60% of tumours at this level in our study. Deep involvement of the cerebral parenchyma is characteristic of primary cerebral lymphoma of the central nervous system, 85% of which are reported as supratentorial.26 Unlike that published in the scientific literature, we recorded no case with frontal lobe involvement in our study.
Neurinoma is the most frequent spinal cord tumour; typically it presents in an intramedullary location with respect to the spinal cord.27 In our series neurinomas constituted 45% of tumours of the spinal cord. Ependymoma are another major spinal cord neoplasm.28,29 Meningiomas are less common at this level. Some series report a ratio with intracranial tumours of 4:1–20:1.30 In our institution we found an intracranial:spinal ratio of 6:1. Spinal cord involvement is affected by haematogenous, lymphatic and contiguity spread. In a study in 130 patients with metastatic spinal involvement, Gilbert et al.31 observed that 68% were at thoracic level, followed by lumbar involvement.32 Thoracic involvement represented 46% and lumbar 27% in the patients of our study.
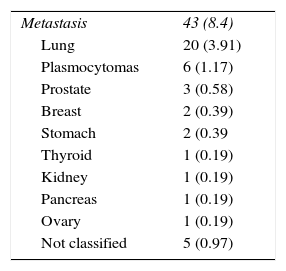
Central nervous system metastases present in approximately 10–30% of patients with malignant tumours and are probably the most common neoplasm. Unfortunately, because they have a poor prognosis and are considered a terminal disease, these lesions are not operated in most centres and, furthermore, are seldom reported.33 Smedby et al.,34 in a study comprising more than 15,517 patients, established that the most common primary tumour is located in the lung, followed by melanoma and breast tumours. In our institution we observed a greater incidence in males, and lung cancer was the primary with the greatest propensity to metastasise at 46.5% (Table 4).
In this study, we sought to gain a perspective on central nervous system tumours in our population. Our study covers a period of 20 years, which we consider significant, as it enabled us to analyse behaviour and possible changes over the years. However, a weakness of the study lies in the total number of patients studied. Despite the fact that we had a relatively large sample, we are convinced that if this number had been greater we would have better represented this environment.
ConclusionThis is the first case series in Mexico to consider malignant and benign central nervous system tumours, involving patients of all age groups over a period of 20 years. Although this study is only a retrospective analysis of one single institution, it can be a strong indication of the epidemiology of these tumours in our environment.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
To the Education and Research Centre of the Hospital Español de la Ciudad de México. To doctor Alejandra Zárate Osorno and the Pathology Laboratory of the Hospital Español de la Ciudad de México for their support.
Please cite this article as: Anaya-Delgadillo G, de Juambelz-Cisneros PP, Fernández-Alvarado B, Pazos-Gómez F, Velasco-Torre A, Revuelta-Gutiérrez R. Prevalencia de tumores del sistema nervioso central y su identificación histológica en pacientes operados: 20 años de experiencia. Cir Cir. 2016;84:447–453.