The structural characteristics of the fibula, strength, shape, length and limited donor site morbidity make it more suitable for reconstructing long bone defects larger than 6cm in the limbs.
Material and methodsA descriptive study was conducted using a non-probabilistic sample of consecutive cases undergoing on limb reconstruction with free fibular flap in the period from January 2010 to January 2015 in the Mexican Institute of Social Security No. 21, Monterrey, Nuevo Leon.
ResultsThe mean age of the ten cases included was 25 years, with the most common diagnosis being trauma in 4 patients, osteosarcoma in 2, followed by one congenital pseudoarthrosis of the tibia, one non-union fracture, and one gunshot wounds, respectively. The most common location was tibia, followed by humerus, radius, ulna and femur.
ConclusionsThis study has shown that the fibular free flap can be an excellent option for management of long bone defects, regardless of cause of the injury. One or more skin islands can be added for coverage in exposure of deep tissue and osteosynthesis material, thus preserving the septocutaneous perforators.
Las características estructurales del peroné: fuerza, forma, longitud y, morbilidad limitada del sitio donador, lo convierten en un colgajo excelente para la reconstrucción de grandes defectos óseos mayores de 6cm en extremidades.
Material y métodosMediante un muestreo no probabilístico de casos consecutivos se realizó un estudio descriptivo de los pacientes operados de reconstrucción de extremidades con colgajo libre de peroné, en el periodo comprendido entre enero de 2010 a enero de 2015 en la Unidad Médica de Alta especialidad No. 21 del Instituto Mexicano del Seguro Social, Monterrey, Nuevo León.
ResultadosSe obtuvo un total de 10 pacientes, la edad promedio fue de 25 años con un diagnóstico de traumatismo como el más frecuente con 4 pacientes, seguido de osteosarcoma con 2 pacientes, seudoartrosis congénita de tibia, falta de consolidación de fractura y herida por proyectil de arma de fuego con uno respectivamente. La localización más común fue tibia, seguido de húmero, radio, cubito y fémur.
ConclusionesEl colgajo libre de peroné es una excelente opción en reconstrucción de defectos óseos de 6cm o mayores en extremidades superiores e inferiores, independientemente de la causa de lesión. Conservando las perforantes septocutáneas puede agregarse una o más islas de piel para cobertura en exposición de tejidos profundos y material de osteosíntesis.
One of the most significant advances in reconstructive surgery during the last few decades has been the introduction of microsurgical techniques for tissue transfer, subsequently leading to broadening therapeutic options on undertaking more refined and safer procedures both from a functional and aesthetic viewpoint, and thus resolving many complex reconstructive problems.1,2
Limb salvage based on extensive oncological resection and reconstruction combined with free microvascular flaps has become the primary aim for bone tumour treatment. It facilitates vascularisation and the necessary nutrients whilst simultaneously providing a resistant structure and the necessary robustness to preserve function.3–5
The structural characteristics of the fibula, such as strength, shape, length and limited donor site morbidity, make it an excellent tool for reconstructing long bone limb defects. Taylor et al.6 published the first successful free fibular flap report in 1975. In 1983 Yoshimura et al.7 added a skin island for flap vascularity monitoring. In 19798 Gilbert, and in 1980 Tamai et al.9 refined the method for fibula removal with a significant reduction in surgery time. The technique therefore evolved and was made much easier to apply. Since then the free fibula flap has been extensively used in the management of long bone defects larger than 6cm.
Several authors have reported that if the bone defect is under 6cm, a conventional bone graft with clamping plates or fasteners is sufficient. A microvascular fibula flab is also necessary in larger defects or in those with a poor vascular bed or with chronic osteomyelitis.10,11 Revascularisation which occurs on completion of anastomosis preserves the function of the osteoblasts and osteoclasts, with for consolidation and remodelling of fractures being incorporated faster and more efficiently than the bone graft.11,12 Despite the disadvantage this procedure has due to the complexity of the surgical technique, using a short pedicle which may hinder anastomosis in the receptor bed, the risk of obstruction of the peroneal vessels during flap dissection and the need for osteotomies during its obtainment, this procedure is currently considered a flap which enhances safe vascularity, which is also related to the surgeon's experience in microsurgical procedures.13–15
The free fibula flap has been reported in reconstruction of the bony parts of the head and neck, using 1 or 2 skin island and as a simple flap or double barrelled flap. Its versatility has led to it becoming the most frequently used microvascular bone or bone and skin flap today.13–23
Material and methodsThrough a non probabilistic sample of consecutive cases a descriptive and retrospective study was carried out taking as inclusion criteria all cases of inferior and superior limb reconstruction using free fibula microvascularised flaps during the period between January 1, 2010 and January 1, 2015 in the Unidad Médica de Alta Especialidad of the Instituto Mexicano del Seguro Social in Monterrey, Nuevo León, Mexico. Exclusion criteria were those patients which did not have a complete clinical history, and those cases where a free fibula flap was used for reconstruction which did not affect the limbs. All cases were managed by the main author.
Patients with lesions of a limb which was treated with a different type of flap and those for whom a free fibula microvascular flap had been used for lower or upper jaw reconstruction were excluded.
For patients who met the inclusion criteria, the following variables were taken into consideration: age, sex, affected limb, diagnosis, affected side, short term evolution (one postoperative week) and long term (one to 3 years from initial date of surgery).
Bone consolidation criteria was based on radiological outcome reflected by ossification data relating to the bridge between the receptor and donor (fibula) bone.
The clinical files of the patients who participated in the study were analysed, taking into account the before-mentioned variables and the radiologic findings one year after surgery. The results obtained were recorded on a data collection sheet for carrying out descriptive statistical analysis with the SPSS 10.0 programme for Windows.
ResultsDuring the period between January 1, 2010 and January 1, 2015, 220 free microvascular flaps were carried out by the main author. Of these, 14 were free flaps based on the peroneal artery: 3 for lower jaw reconstruction, one for upper jaw and 10 for the reconstruction of limbs. Of the latter, the average age was 25 (SD±16), with an age range between 2 and 54.
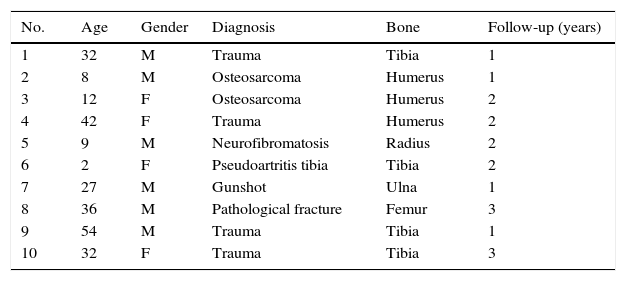
Patient diagnoses taken into account for the study were as follows: secondary to trauma (4 patients), osteosarcoma (2 patients), followed by congenital pseudoarthritis of the tibia (one), neurofibromatosis (one), posterior pathological fracture to resection of a Ewing sarcoma 15 years previously (one) and gunshot wound (one). The data obtained for each patient is shown in Table 1.
Epidemiological profile and patient characteristics of those who participated in the study.
| No. | Age | Gender | Diagnosis | Bone | Follow-up (years) |
|---|---|---|---|---|---|
| 1 | 32 | M | Trauma | Tibia | 1 |
| 2 | 8 | M | Osteosarcoma | Humerus | 1 |
| 3 | 12 | F | Osteosarcoma | Humerus | 2 |
| 4 | 42 | F | Trauma | Humerus | 2 |
| 5 | 9 | M | Neurofibromatosis | Radius | 2 |
| 6 | 2 | F | Pseudoartritis tibia | Tibia | 2 |
| 7 | 27 | M | Gunshot | Ulna | 1 |
| 8 | 36 | M | Pathological fracture | Femur | 3 |
| 9 | 54 | M | Trauma | Tibia | 1 |
| 10 | 32 | F | Trauma | Tibia | 3 |
F: female; M: male.
The most frequently reconstructed bone was the tibia, for 4 patients, followed by the humerus for 3, and radius, ulna and femur for one respectively.
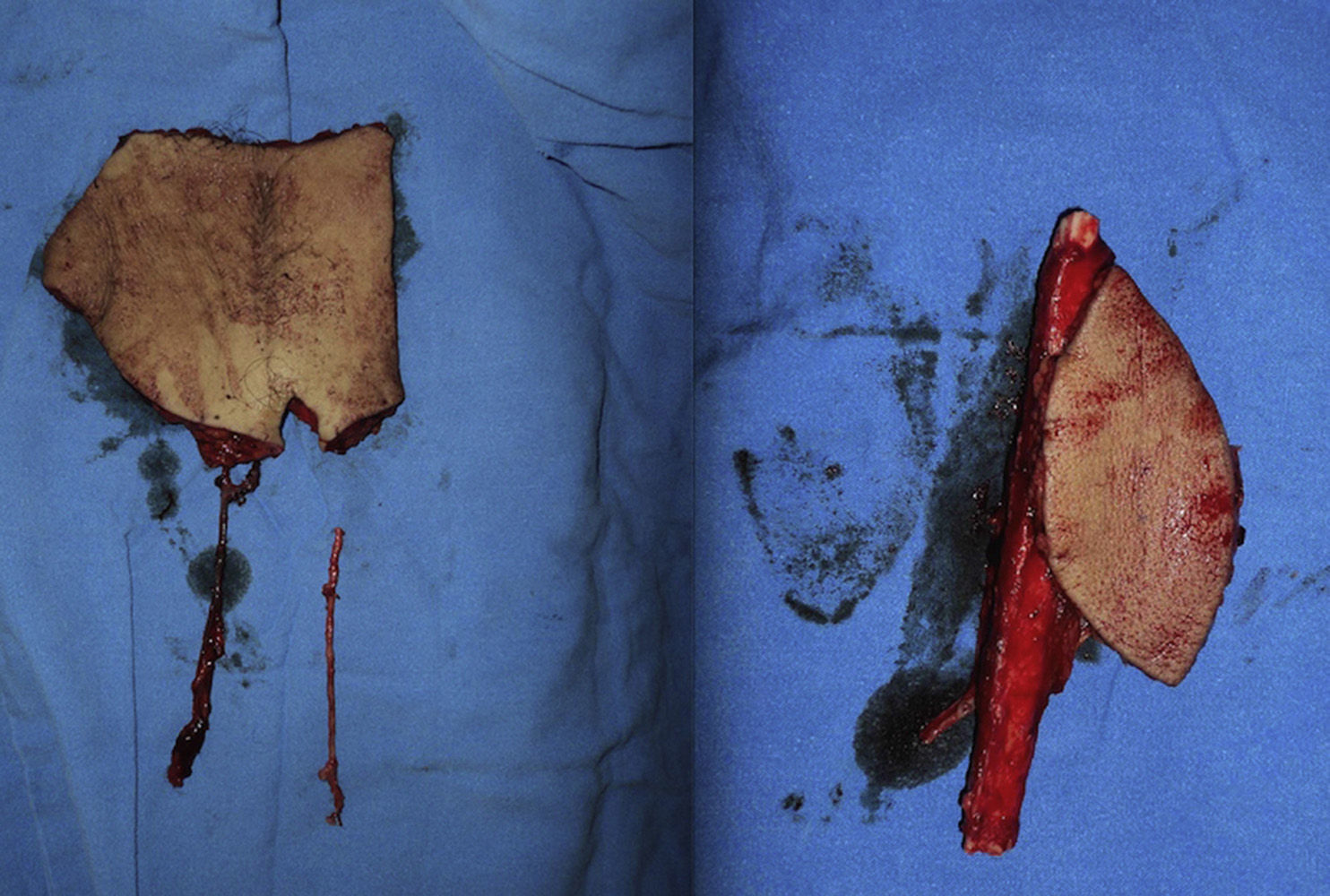
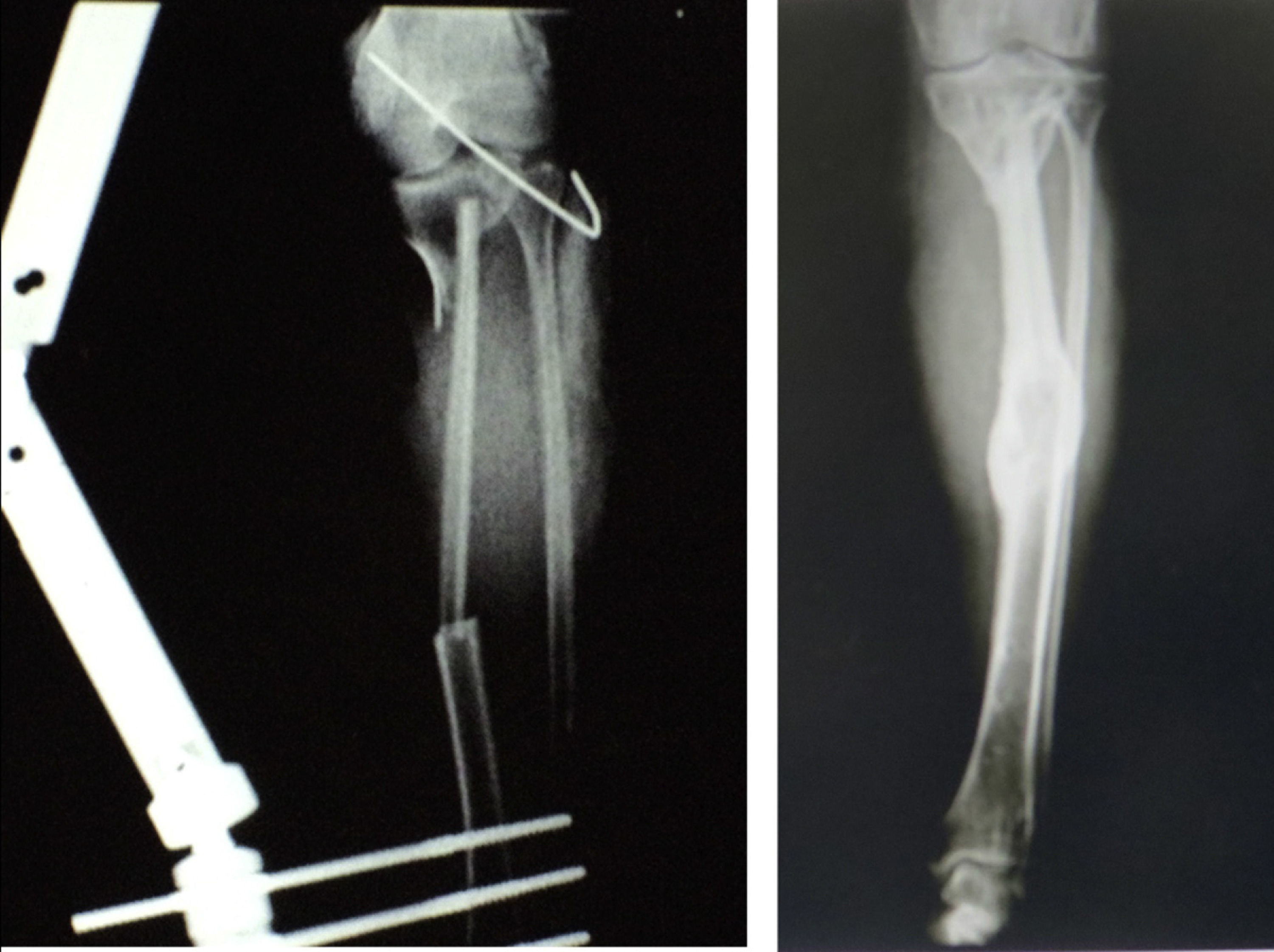
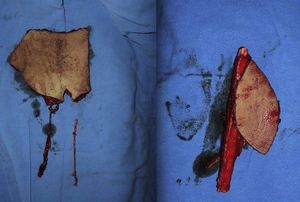
Three flaps were performed as sequential (hip), 2 anastomosed to an anterolateral flap of the thigh and one anastomosed to a deep inferior epigastric artery flap. These were all for reconstruction of the lower leg. The longest bone managed was 22cm, which was used to reconstruct the tibia of a patient with bone loss secondary to a motorcycle accident. Due to the large absence of coverage, a flap of the deep inferior epigastric artery was simultaneously sequentially anastomosed to the fibula flap. The images from this clinical case are shown in Figs. 1 and 2, and its outcome 3 years after surgery (2 patients) in Figs. 3 and 4.
Free flap of the deep (left) inferior epigastric artery and free fibula flap with skin island (right). A saphenous vein graft was used which was proximally anastomosado lateral-end to the superficial femoral artery and distally to the proximal part of the deep inferior epigastric artery of the deep inferior epigastric artery flap. The distal end of the latter was joined to the peroneal artery of the fibula flap (sequential flap).
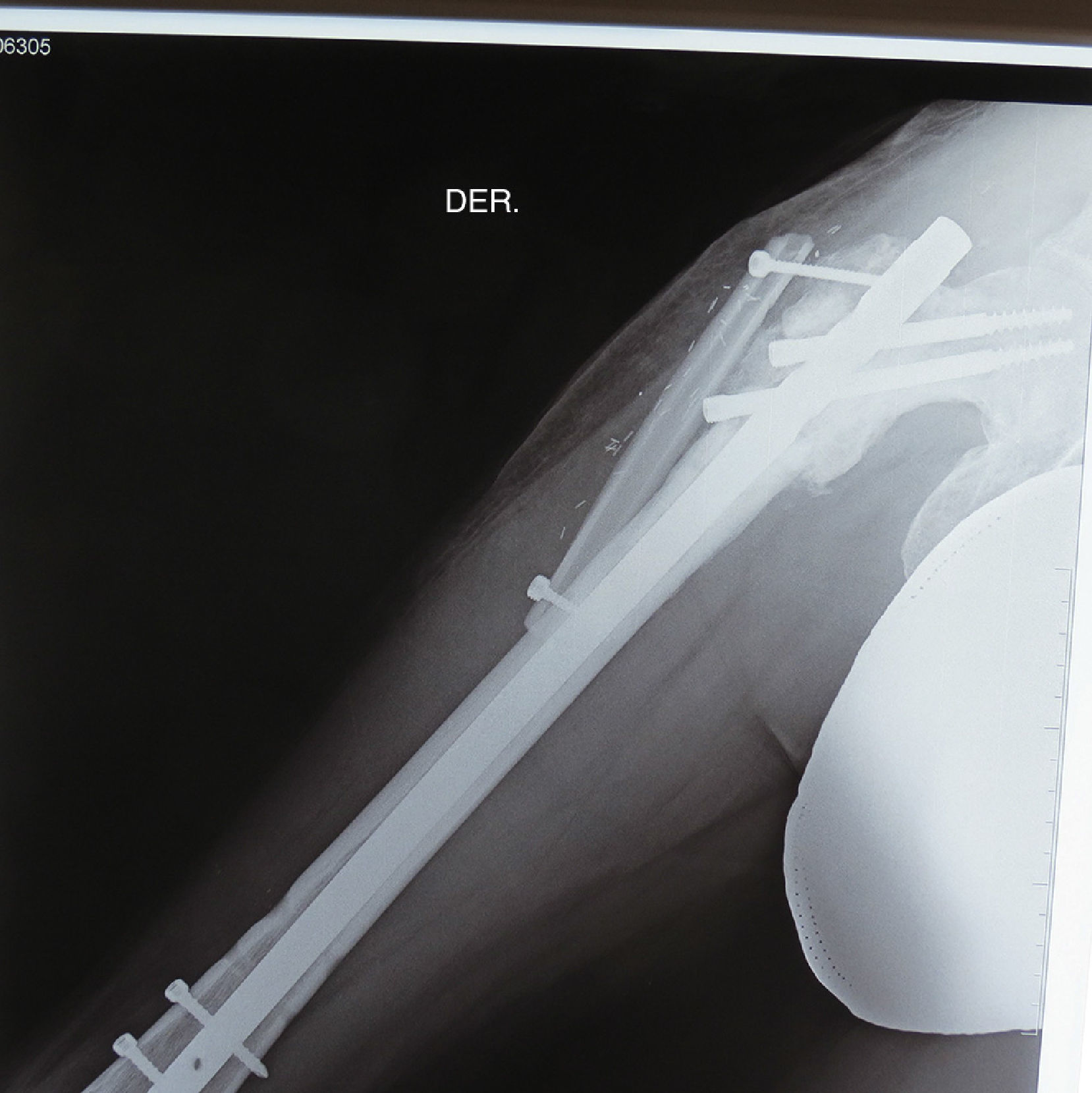
The flaps for reconstruction of the tibia were inserted into the medullary cavity and an external fastener was then attached. In the case of femur reconstruction secondary to a fracture caused by breakage of a centromedullary pin inserted 15 years previously during resection of a Ewing sarcoma, the pathological fracture site was later treated with bicortical screws used as a “splint” (Figs. 5 and 6). The average time in which initial bone consolidation data were observed in the radiologic studies was 6 weeks.
Six of the patients (60%) required an internal saphenous vein graft. All the above mentioned patients presented with good vascular permeability and total flap integration. Two patients had to be reoperated on for complications unconnected to the fibula flap. In one of the humerus sarcoma cases there was rejection of the osteosynthesis (wire) material, at the shoulder level and it had to be removed one month after initial surgery, and in the case of the 2 years old patient, with congenital pseudoarthritis of the tibia, the patient relapsed and a new leg deformity presented. In the control radiography of initial surgery, good integration of the receptor tibia was observed but the remaining tibia presented with new deformity, and it was necessary to perform corrective osteotomies.
The remaining patients did not present with complications in either the donor area or the receptor area in the follow-up carried out from 1 to 3 years.
DiscussionOne of the major challenges of reconstructive surgery is coverage of complex defects in limbs, with exposure of deep tissues and on occasions their absence. From the advent of the microvascular era, perforator flaps have been the treatment of choice in complex reconstructions up to the present time.
Since 1975 when Taylor et al. described the free fibula flap,6 it has been used as the reconstructive option in many hospital of worldwide renown, and has been a useful tool for superior, inferior, pelvis, head and neck bone reconstruction.
During the last 2 decades, general management of limb sarcomas has evolved from amputation to conservative resections combined with chemo and radiotherapy. Although this form of treatment has led to an acceptable rate of control of the disease, limb salvage has been associated with the reduction in its function. Local flaps and bone grafts are options which lead to insufficient reconstruction with a very high rate of complications.15–20 In our study only 2 patients underwent resection of the humerus due to osteosarcoma and immediate reconstruction with free fibula flap. Both patients evolved favourably with no relapses to date.
The function of the arm depends on preservation of the humeral head, which in our study was resected in both cases. However, the function of the hand and elbow was 100% preserved. The shoulder, however, lost its capacity for abduction.
The absence of skin and the need for reconstruction with a chimeric type flap based on septocutaneous perforator vessels of the main femur pedicle is frequently seen in defects secondary to trauma. An average of 92 perforators have been reported for the lower limb, of which 30 correspond to the leg and knee, and of these between 4 and 7 may be used to preserve a skin island with a fibular flap.1,24
In this study, the main cause of the bone and skin defect was due to severe trauma from high speed mechanisms, with the reconstruction in all cases taking place between one and 6 weeks after the initial trauma. In one case, a skin island was used for coverage of the osteosynthesis material and deep tissues. In 3 cases, the defect was too extensive and as a result, to reduce the morbidity of the donor area a secondary sequential flab for skin coverage was used (2 anterolateral thigh flaps and one flap based on the deep inferior epigastric artery respectively); these flaps were anastomosed to the distal fibula branch of the primary flap.
Unlike that reported by Kalra et al.11 there were no differences in the success of our reconstructions both immediate and deferred, with vascular viability presenting in 100% of flaps.
Reconstruction through ipislateral pedicle flap transposition continues to offer excellent possibilities but it is rare for patients to only present with severe trauma fractures without loss of soft tissue. Furthermore, it would also be difficult to carry out on patients whose cause of tibia resection are tumours since it is impossible to perform this technique for the reconstruction of the proximal or distal tibia due to blood flow from the peroneal artery, which penetrates in the middle third at 6 or 7cm from origin, limiting the rotation arc of the transposed fibula.
In centres where microsurgery is not practised, cadaver allografts are a reasonable alternative when there are long bone defects over 6cm. However, some of the disadvantages of the use of these allografts is their associated high morbidity, in addition to failure to consolidate, delay in consolidation, re-absorption and infections which may present in both the bone and the soft tissues, as confirmed by Belt et al.15 In his study complications were found in 48% of patients who had received a cadaver bone allograft and this resulted in its loss.
ConclusionsThe free fibula flap is an excellent option in the reconstruction of bone defects of 6cm or longer, in upper and lower limbs, regardless of the cause of the lesion. Versatility of the same may be assisted by a skin island based on septocutaneous perforators of the peroneal artery, which facilitate coverage of skin defects, with exposure of deep tissues or osteosynthesis material. For major defects skin coverage may be used with a secondary sequential flap. The one most frequently used is the anterolateral thigh flap. The interior flap of the deep inferior epigastric artery is a good option for coverage of larger defects.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: de la Parra-Márquez M, Zorola-Tellez O, Cárdenas-Rodríguez S, Rangel-Flores JM, Sánchez-Terrones G. Versatilidad del colgajo microvascular de peroné en reconstrucción de extremidades. Cirugía y Cirujanos. 2016;84:213–219.