The presence of fibrous membranes that encompass the intestines, forming a sort of butterfly cocoon, is a very rare cause of intestinal obstruction in our setting.
It affects young and adolescent girls in tropical and subtropical countries. Symptoms are nonspecific and preoperative diagnosis is extremely difficult. Surgery is essential to take membrane samples that confirm the diagnosis for treatment.
We present the case of a 14-year-old patient who came to the Emergency Department with colic abdominal pain located in the hypogastrium and bilious vomiting. She reported having lost 7kg in 2 months. During abdominal examination, a hard, painful mass was palpated in the hypogastrium, which occupied the entire lower hemiabdomen. The patient, who was from Pakistan, had been in our country for 4 days.
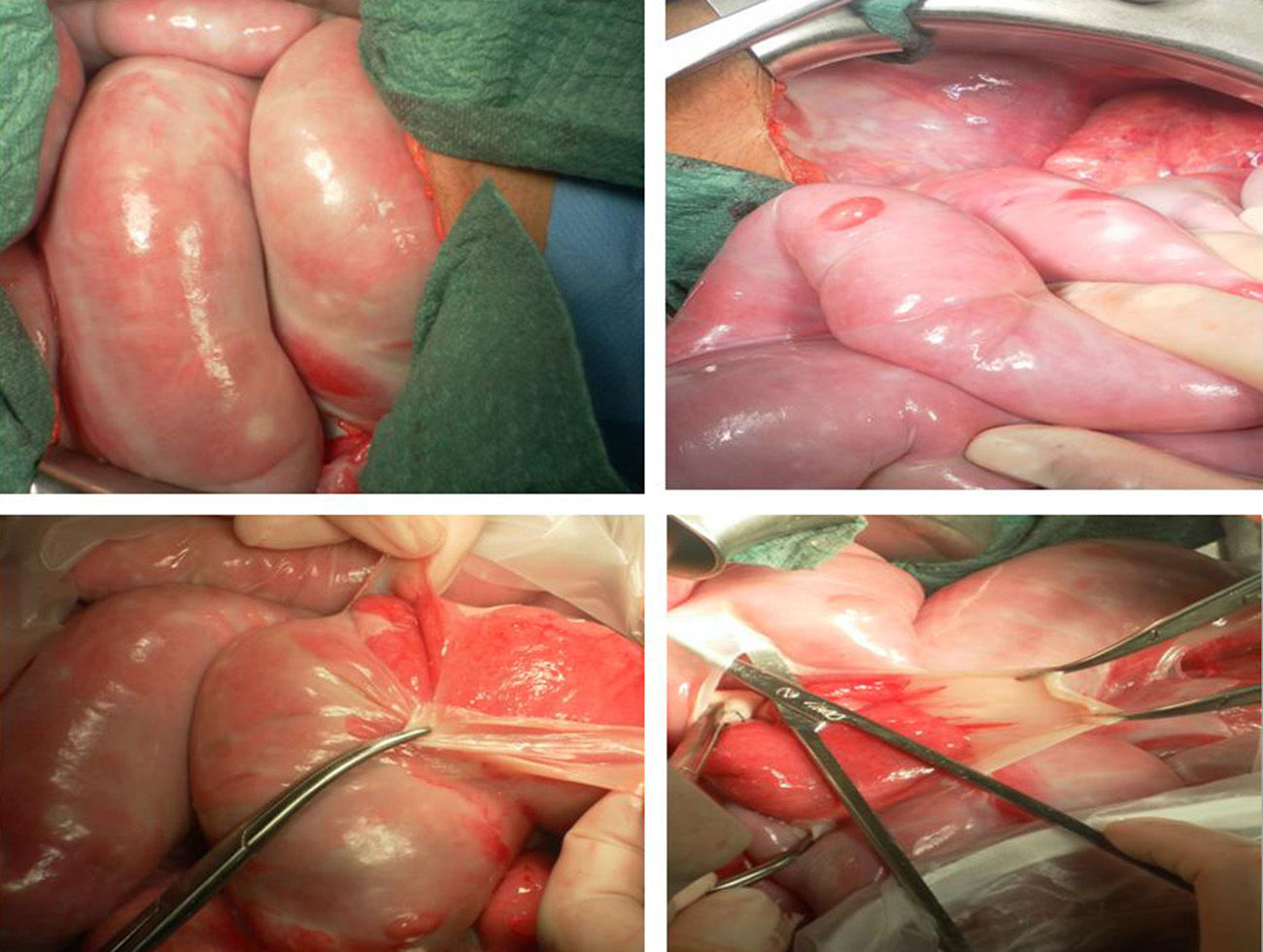
Given the presence of an abdominal mass with a possible tumour origin, ultrasound and abdominal-pelvic CT scan were ordered (Fig. 1). In both examinations, dilatation of the small bowel loops was observed in the same location as the mass, and adjacent structures had been displaced. The diagnosis was partial small-bowel obstruction, although no apparent extrinsic cause was able to be identified.
Lab work-up, including blood tests and biochemistry, were normal. PPD was negative.
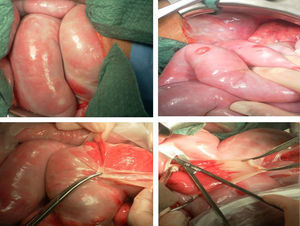
The patient underwent exploratory midline laparotomy. We observed that the mass was made up of intestinal loops that moved within a whitish fibrous sheath that was elastic, drawn back and adhered to itself, which is described in the literature as a “cocoon” (Fig. 2). We dealt with the sheath, which was able to be separated by blunt dissection from the intestinal wall, which was normal in appearance, completely releasing the small bowel and adherences with no need for intestinal resection. Biopsies were taken and samples of the membranes were sent for culture. The pathology study reported whitish-grey membranes comprised of a fibrous tissue with a moderate amount of capillaries that were densely collagenised and the occasional presence of epithelial tubular structures of probable embryonic origin, with no evidence of intestinal muscle cells.
The culture results were negative for virus, bacteria and mycobacteria.
The postoperative progress was favourable, and the patient received parenteral nutrition for 5 days with a very good results.
Two months later, she had recovered her usual weight. One year after surgery, a gastrointestinal transit study showed that the distribution of the intestinal loops was normal.
Abdominal cocoon, or “primary sclerosing encapsulating peritonitis”, is a rare disease of unknown aetiology reported in subtropical and tropical countries, in which the intestine is covered by membranes that cause intestinal obstruction.1 The first report of this condition dates from 1868, and since then scarcely 50 cases have been reported. Its idiopathic type affects girls and teens.2
There have been descriptions of cases secondary to chronic inflammatory processes and in association with continuous ambulatory peritoneal dialysis, abdominal tuberculosis, treatment with beta blockers, recurrent peritonitis, liver transplantation, ventriculoperitoneal shunts, etc. It has also been found in 38% of autopsies done in cirrhotic patients with peritoneovenous shunts.
In primary or idiopathic abdominal cocoons,3 diverse hypotheses have been proposed to explain the possible aetiology, including retrograde menstruation, viral infection, or cell-mediated immunological response. There is even a possible congenital aetiology,4 as in some cases it is accompanied by hypoplasia of the greater omentum or altered development due to the continuous growth of the intestinal loops contained in an accessory peritoneal membrane.
Although this pathology is extremely rare in our setting, the importance of knowing about it is relevant due to the consequences that may arise without a correct diagnosis and treatment.
This condition should be considered in girls and young adolescent females who are from tropical and subtropical countries5 (mainly Pakistan, China and India) who present with partial obstruction, and in whom an abdominal mass is palpated with no apparent identifiable cause of the obstruction using standard complementary studies (ultrasound, tomography or magnetic resonance). Identification of the membranes prior to surgery is very difficult. Treatment is essentially surgical and is key for favourable patient progress. Intestinal resection of the mass is not necessary. Surgical treatment should be limited to releasing the trapped bowel by dividing and resecting the membranes, which are easily separated from the normal intestinal wall.
Please cite this article as: Abad Calvo P, de Diego Suárez M, Isnard Blanchar RM, Ojanguren Sabán I, Castellví Gil A. Cocoon abdominal: reto diagnóstico y tratamiento. A propósito de un caso. Cir Esp. 2015;93:e61–e62.
Parts of this case report were presented in poster format at the Annual Meeting of the Catalonian Society of Pediatrics in Figueras, Spain, 2012.