Acute appendicitis is one of the most common causes of acute abdomen and one of the most frequent indications of urgent abdominal surgery. Obstruction of the ileocecal appendix has been proposed as the main etiology of this disease, although it is not always identified, which is why some authors consider that obstruction is the result and not the cause of inflammation.1–3 There is no single theory that explains all cases of acute appendicitis, and the etiology of inflammation varies depending on patient age. Infections and follicular lymphoid hyperplasia are more frequent in young people, while in adults we can find fibrosis, fecaliths or neoplasms.2,4 Parasite infection is a rare cause of acute appendicitis.1 These parasitoses include Enterobius, Ascaris, Giardia and Entamoeba histolytica.2 We present a clinical case demonstrating the presence of Enterobius vermicularis (E. vermicularis) during an appendectomy.
We present the case of a 20-year-old male who came to the Emergency Room 3 times due to abdominal pain that had been progressing over the course of 10 day located in the right iliac fossa (RIF) accompanied by nausea, with no other notable symptoms. On his first visit to the emergency room, systematic testing showed mild hematuria and mild leukocytosis. An abdominal ultrasound was performed, although the ileocecal appendix could not be identified, so the patient was discharged with suspected urinary infection and treated with broad-spectrum antibiotic therapy. Due to the persistence of the symptoms, the patient returned to the emergency department again, where there was notable abdominal pain in the RIF and a positive Blumberg sign. At this time, blood work showed no evidence of leukocytosis and eosinophilia of 9.7%. Due to the persisting symptoms and the non-visualization of the appendix on ultrasound, an abdominal CT scan was ordered, which identified a retrocecal appendix whose diameter was at the upper limit of normal.
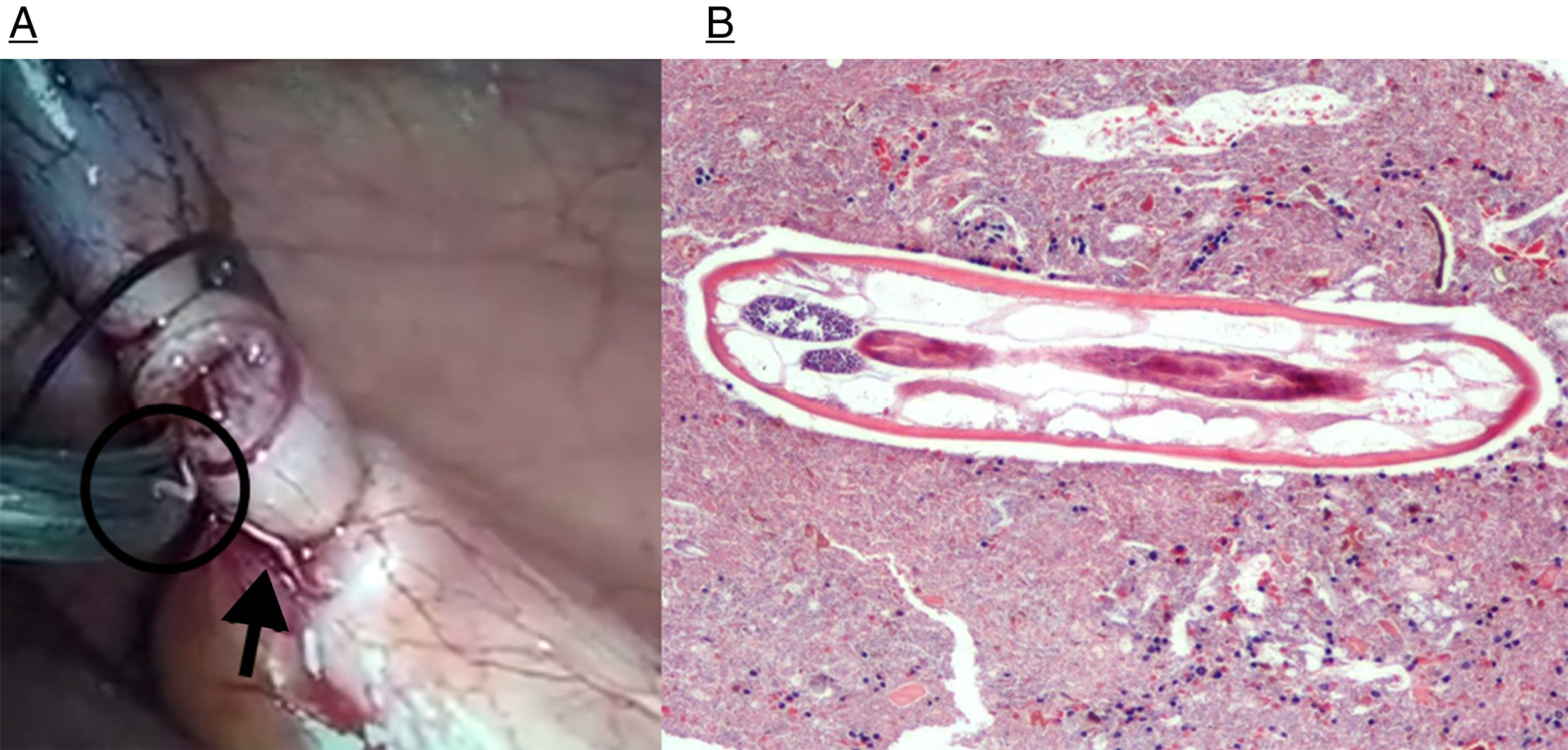
Given these findings, the patient was operated on using laparoscopic appendectomy. When the base of the appendix was cut, 2 millimetric parasites were seen entering the abdominal cavity (Fig. 1A). After the intervention, the patient's symptoms improved and then disappeared. The surgical piece was sent for pathology study, and the infestation was treated with oral albendazole while a stool sample was studied for parasites. The fecal study was positive for E. vermicularis. The pathology study of the surgical piece reported the presence of parasites (E. vermicularis) and vascular congestion of the appendiceal mucosa (Figs. 1B and 2), with no other findings of interest.
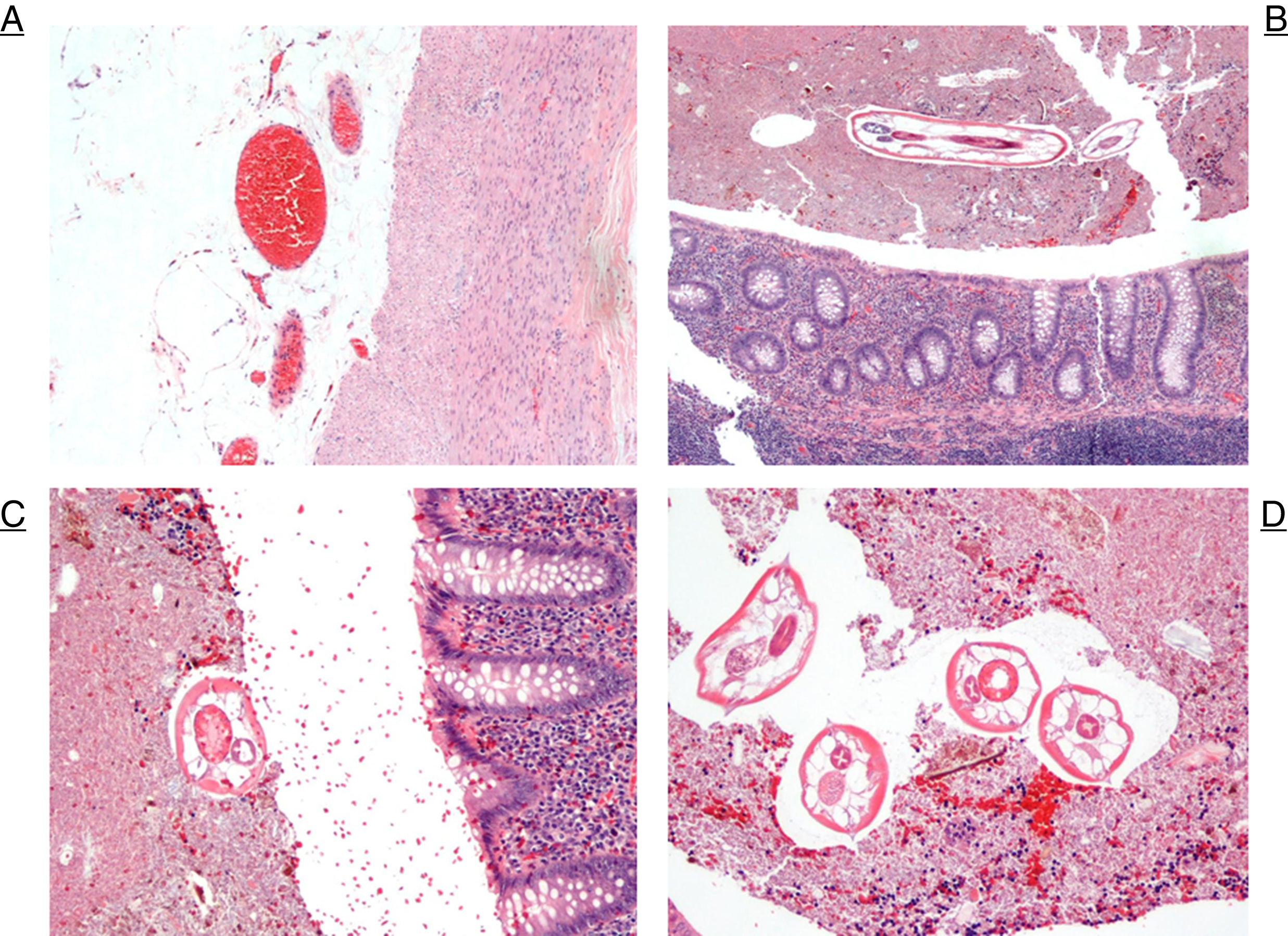
(A) The external appendicular wall is seen with the fat of the serosa, showing congestive vessels and the muscular layers on the right (H&E ×10); (B) low magnification image of the appendix. Towards the top, observe the body of the parasite between fecaloid material. At the bottom, the appendiceal mucosa can be seen without apparent changes in inflammatory type (H&E ×4); (C) at higher magnification, a section of the parasite and the upper margin of the appendiceal mucosa (H&E ×20); (D) several sections of the parasites between fecaloid material (H&E ×20).
E. vermicularis is a species of parasite of the phylum nematodes that affects humans and is commonly known as pinworms. It is the most frequent nematode infection worldwide; however, there are considerable geographical variations.5,6 The greater prevalence of infection occurs in children and adolescents, especially when hospitalized.2 The main host is the human being, and transmission is fecal-oral.3 After the ingestion of the eggs, these later hatch in the duodenum. The larvae migrate to the cecum and to the areas of the adjacent intestine (including the appendix), where they mature and become adults.3,6,7
E. vermicularis infestations may present as multiple clinical manifestations, including acute appendicitis. They have been isolated in appendectomy pieces from all continents and age ranges.8 The presence of pinworms in resected appendices ranges from 0.6% to 13%; however, the ability of these parasites to damage the mucosa of the appendix is controversial.2 Some authors state that the inflammation surrounding E. vermicularis in the pathology pieces occurs after appendectomy in order to escape the decrease in oxygen concentration.2 In the pieces studied for suspected acute appendicitis and with infestation by these parasites, it is more common to find appendices with normal histology and less frequently associated with the histological changes typical of acute appendicitis.1
Due to these histological findings, the role of E. vermicularis infection as a cause of acute appendicitis is still very controversial.5 However, it is well known that they can simulate a clinic compatible with acute appendicitis.3 There are certain pathophysiological mechanisms that produce these symptoms: one is the inflammation of the mucosa due to the simple presence of the parasites and their eggs; another is the obstruction of the appendix. Obstruction by pinworms is similar to that caused by fecaliths, causing localized pain in the RIF but rarely leading to inflammation.5,7 It should not be forgotten that E. vermicularis is a parasitic infection that affects other anatomical areas besides the appendix and that appendectomy does not resolve the infestation. It is also necessary to administer further treatment with antiparasitic agents (albendazole or mebendazole).6 In the pathology study of most surgical pieces, normal histology is most frequent. In our case, the only evidence was vascular congestion of the appendix wall and the presence of E. vermicularis in the piece. Infestation by E. vermicularis can produce clinical signs of acute appendicitis, but it is not a frequent cause.
Please cite this article as: Alejandre Villalobos C, Fernández-SanMillán D, López-Tomassetti Fernández E, Hernández Hernández JR. Apendicitis aguda por parasitosis. Cir Esp. 2018;96:306–308.