Acute emphysematous cholecystitis is a rare disease with a poor prognosis that represents between 1% and 3% of all acute cholecystitis.1 It is characterized by the presence of gas in the gallbladder lumen, wall and pericholecystic tissue caused by gas-producing microorganisms. It is more frequent in diabetic or immunosuppressed patients.2
Cases of acute cholecystitis after cardiac surgery often debut days or weeks after the procedure, and fatal emphysematous cholecystitis within hours of surgery is exceptional. We present a case of sudden acute emphysematous cholecystitis after cardiac surgery.
The patient was a 68-year-old woman with a history of hypertension under medical treatment, anticoagulation for atrial fibrillation and commissurotomy due to rheumatic mitral stenosis 10 years earlier.
The patient underwent scheduled surgery for double aortic valve lesion with a predominance of severe stenosis, which involved the placement of a mechanical aortic prosthesis (cardiopulmonary bypass time 120min and aortic clamping time 60min), with no intraoperative complications.
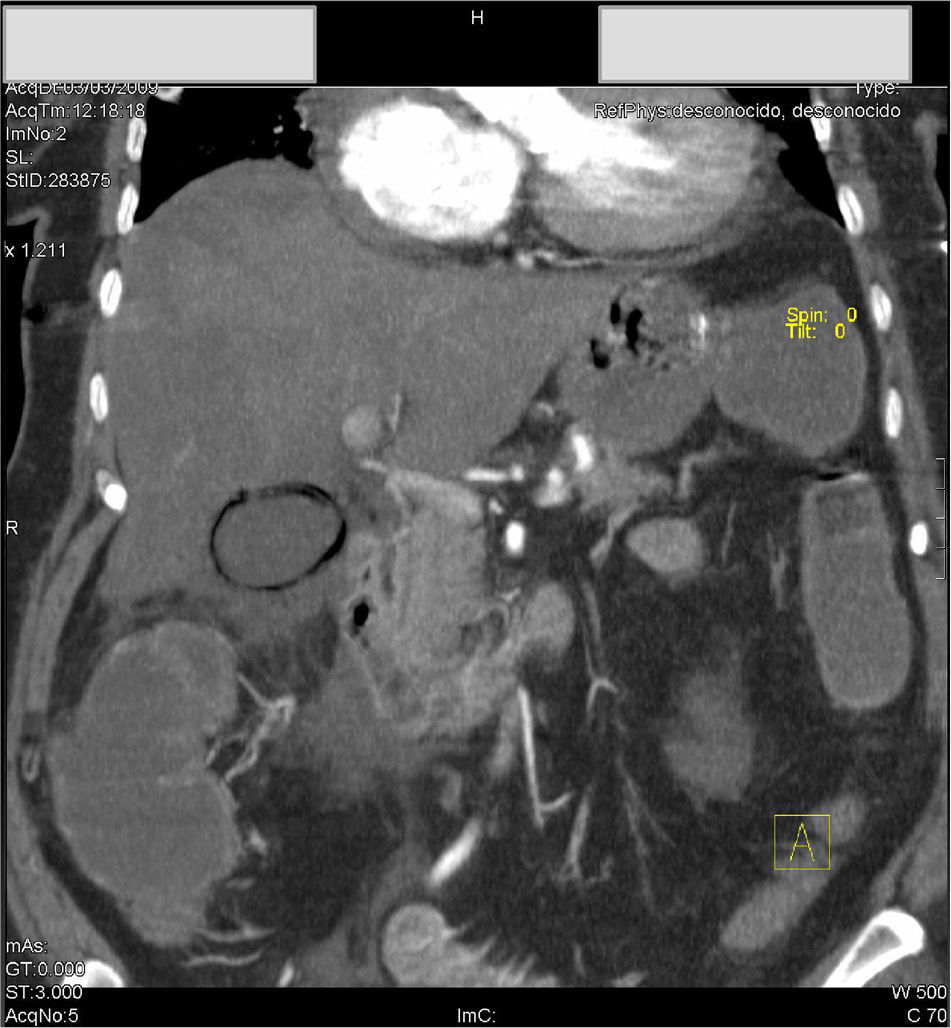
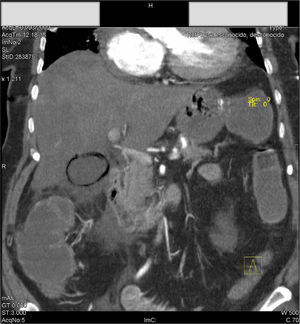
Eight hours after surgery and while still on mechanical ventilation, the patient began abruptly with oliguria, hypotension and tachycardia. Work-up revealed an increase in lactate levels of 9.3mg/dl, Hb 8.3g/dl (the patient left the operating room with 11g/dl) with no bloody discharge through the drains. An upper GI endoscopy was performed to rule out gastrointestinal bleeding, and ischemic gastric mucous membranes were observed. Follow-up analysis showed: GOT 4418; GPT 3195; prothrombin activity 33%; CPK 9013. Emergency CT scan revealed patchy hypodense areas in the liver, permeable hepatic artery and portal vein, acalculous emphysematous cholecystitis and left renal artery thrombosis starting at the aorta (Fig. 1).
Given these findings, emergency exploratory laparotomy was indicated, which demonstrated acute emphysematous cholecystitis, patches of hepatic ischemia and ischemic bowel loops. Cholecystectomy was performed, and bile samples were taken for culture.
The patient was transferred to the ICU, where she developed multiple organ failure and died 72h after the initial surgery. The pathology study reported necrosis of the gallbladder wall with organized thrombi of the small vessels. The bile culture was positive for Bifidobacterium sp.
Acute emphysematous cholecystitis represents between 1% and 3% of acute cholecystitis and is more common in men, the elderly and patients with diabetes mellitus, with a mortality rate of 15%–20%.3 Its pathogenesis involves bacterial invasion of the gallbladder wall by gas-producing bacteria after wall ischemia.
Symptoms are initially similar to simple acute cholecystitis, although they may exceptionally evolve to a fatal outcome. Abdominal CT with contrast demonstrates images of gas in the gallbladder region (Fig. 1). This entity is considered a surgical emergency and the treatment of choice is immediate cholecystectomy in association with broad-spectrum antibiotic coverage. Despite adequate treatment, mortality in these patients is approximately 15%.
Acute cholecystitis after cardiac surgery is uncommon (less than 0.1%), the majority of which are gallstone-related. Very few cases of acute emphysematous cholecystitis with fatal outcome have been reported in the literature after cardiac surgery. We have only found one fulminant case 12h after performing aortography.4 The published patients had a mean time to onset of symptoms of 4–9 days.5,6 The clinical symptoms of our patient, however, were established in less than 8h, possibly precipitated by the hypoperfusion during surgery with cardiopulmonary bypass, triggering massive subsequent thrombosis, ischemia and bacterial infection. The colonization of the gallbladder by a saprophytic anaerobe of the colon can explain how unusual and severe this case was, which rapidly evolved to sepsis and multiple-organ failure.
Please cite this article as: Abrisqueta J, Abellán I, Cascales P, Jara R, Parrilla P. Colecistitis aguda enfisematosa de curso fulminante tras cirugía cardiaca. Cir Esp. 2014;92:62–63.