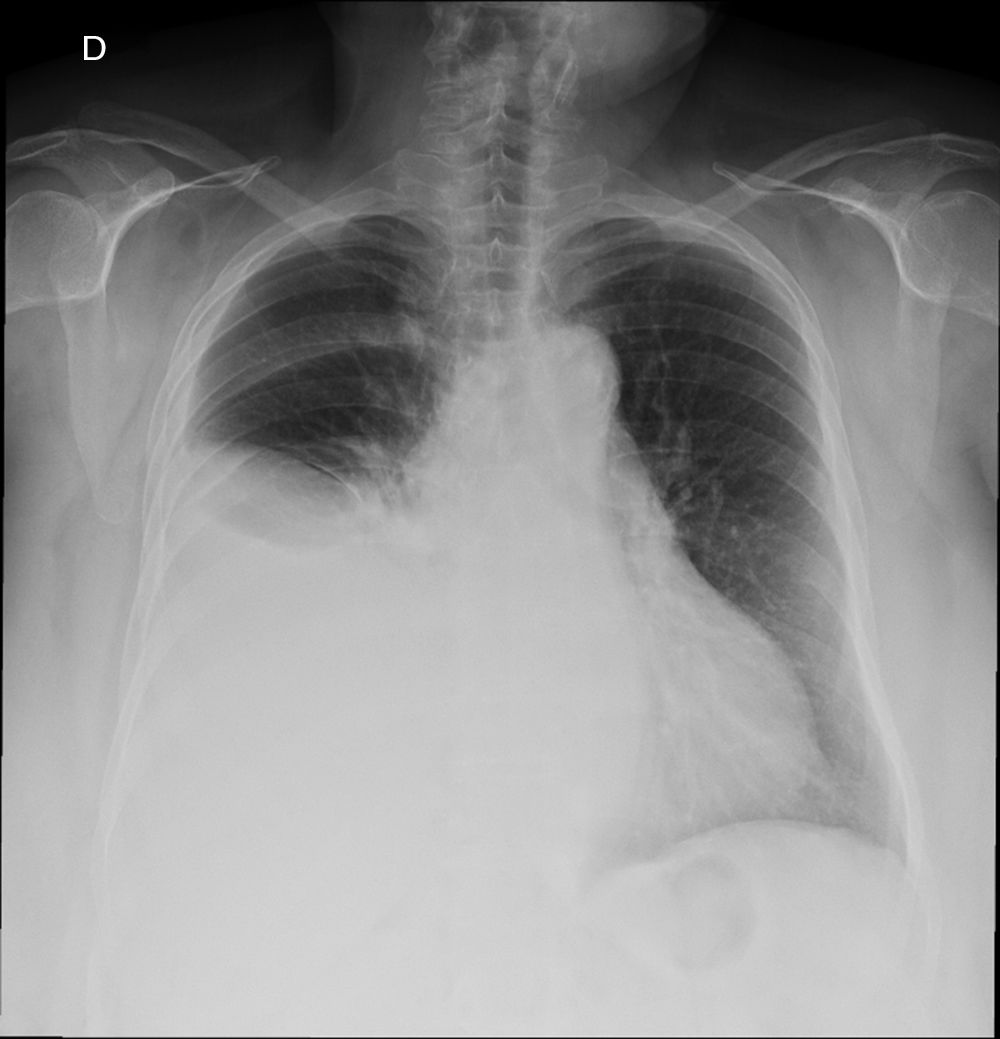
Amyloidosis located in the gastrointestinal tract is an uncommon entity.1,2 Immunoglobulin light chain deposits in the thickness of the intestinal wall cause structural and functional alterations that lead to a great variety of digestive symptoms1,3,4 similar to those of other digestive diseases, such as inflammatory bowel disease, ischemic colitis, collagenous colitis and neoplasms. The subclinical nature of its presentation and nonspecific symptoms make it difficult to correctly diagnose.1,3,4 We present an unusual case of a large solitary amyloid tumor of the descending colon located in the submucosa, with extraluminal extension and associated with changes of lymphoplasmacytic lymphoma involving occlusion at that level. The patient is an 84-year-old man with hypertension and diabetes who came to the Emergency Room for abdominal pain during the previous three days, located in the left iliac fossa, with abdominal distension. In the ER, the patient was stable, with no fever, but had pain, abdominal guarding and palpation of an inflammatory mass in the left iliac fossa. The blood work-up was normal. An abdominal radiograph showed distension of the colon with an abrupt change in size in the left iliac fossa, with absence of gas in the distal sigmoid colon. With a differential diagnosis of acute diverticulitis versus a neoplasm, an abdominal CT scan was ordered (Fig. 1), which showed a 96.6mm tumor located in the descending colon with a filiform contrast path through the lesion.
With the suspicion of an obstructive cancer, a colonoscopy was performed, which revealed an ulcerated and infiltrating mass 45cm from the anal margin invading a large part of the intestinal lumen. Biopsies were performed. As there was no clinical improvement, we decided to carry out deferred emergency surgery, still pending the result of the biopsy performed during the colonoscopy. A left oncological hemicolectomy was conducted, with manual end-to-end anastomosis. In the postoperative period, the patient presented a low-output subclinical intestinal fistula that responded to medical treatment, and the patient was discharged on the tenth postoperative day. The result of the biopsy performed by endoscopy was: “massive deposit of amyloid substance of the AL type in the submucosa”.
The pathology study of the surgical piece reported a large mass that was hard in consistency, measuring 9.5cm×6cm, which showed a yellowish brown tissue when sliced. Microscopically, in the muscular layer of the colon wall there was an abundant deposit of eosinophilic fibrillar material that was amyloid in appearance, with plasma cells positive for CD138, MUM-1, IgG, CD20 and lambda light chain restriction. The final diagnosis was AL-type primary amyloidosis, presented in the form of masses of amyloid deposits measuring 9.5 and 1.5cm in the intestinal serosa, the largest of which ulcerating the intestinal mucosa, with no evidence of malignant epithelial neoplasm. Lymphoplasmacytic lymphoma (Fig. 2).
Amyloidosis is a group of diseases that are characterized by the extracellular deposition of different unbranched protein fibrils that are biochemically heterogeneous and resistant to degradation. These proteins share morphological, staining (Congo red) and similar ultrastructural characteristics, but their chemical structure is different.
The main biochemical types are:
- -
Primary amyloidosis (AL): comprised of lambda or kappa immunoglobulin light chains in the context of hematologic pathologies. This is the most common type and is associated with monoclonal proliferation of B-cells or plasma cells.
- -
Secondary amyloidosis (AA): associated with very long-term chronic inflammatory diseases, such as Crohn's, anchylosing spondylitis, Reiter syndrome, rheumatoid arthritis and systemic erythematous lupus. It is also found in infectious processes like tuberculosis, osteomyelitis and leprosy, as well as in neoplastic processes like renal carcinoma and gastrointestinal stromal tumors.2,3
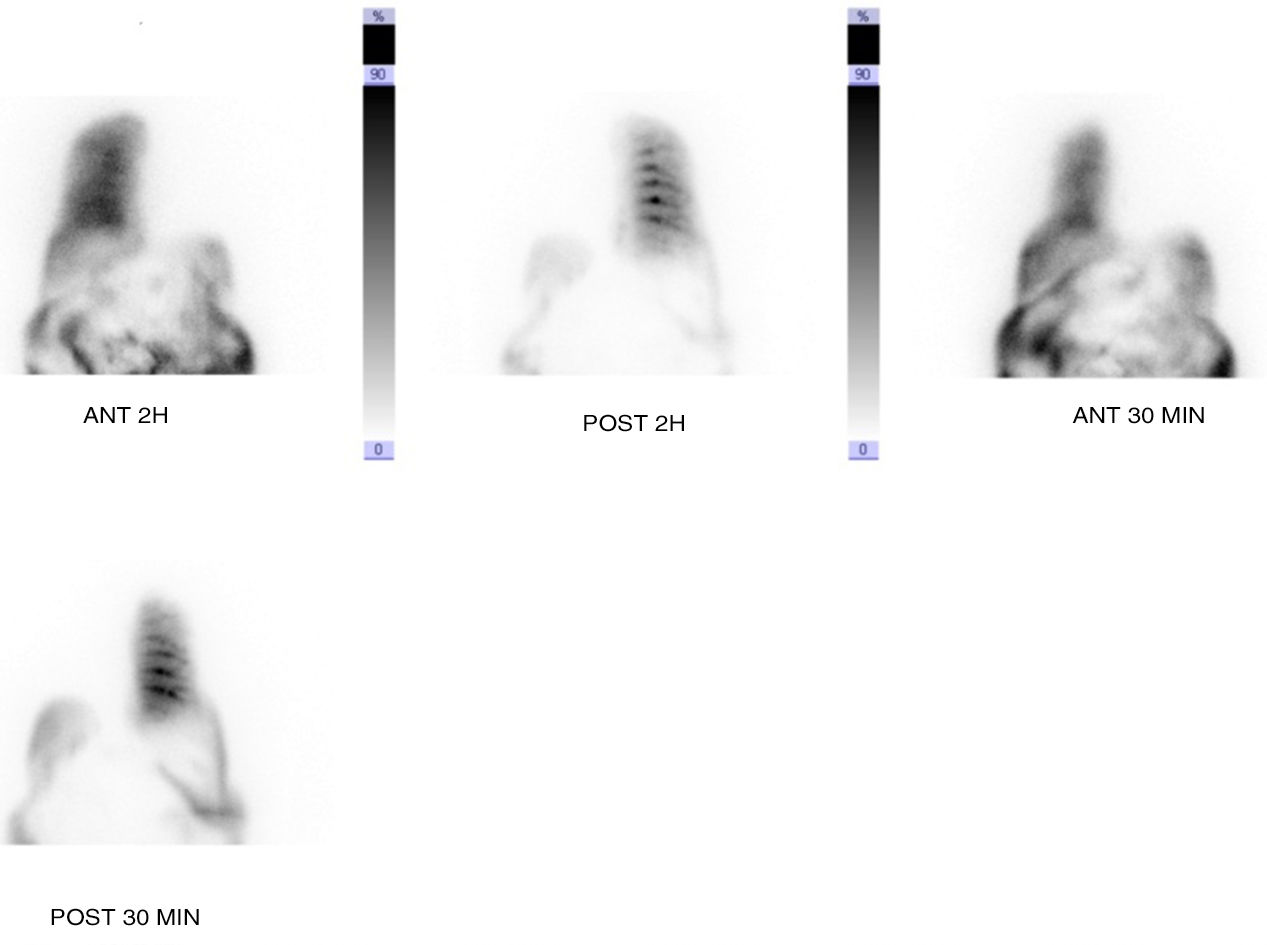
The average age at presentation of AL amyloidosis is 65, and two-thirds of patients are males. Asthenia and weight loss are the most frequent symptoms. The most affected organs are the kidneys (70%–80%) and heart (50%–60%).1–5 Amyloidosis located in the gastrointestinal tract is a rare entity, and the most common form is AL. The clinical manifestations are variable, non-specific and may depend on the type of amyloidosis: AL usually presents as an obstructive condition, and AA presents with symptoms of malabsorption, diarrhea and bleeding.2,3 The endoscopic and radiological findings are not specific.2,3 The diagnosis and type of amyloid are obtained with the histological result of the biopsy, and Congo red staining is the most specific.2–4 In cases like this, in which the diagnosis of amyloidosis is postoperative, it is important to determine whether the involvement is local or systemic because the management and prognoses are different. Plasma and urine electrophoresis studies, autoimmune markers, electrocardiogram and echocardiogram were performed to check the most frequently affected organs.5,6
The treatment of amyloidosis depends on the type of amyloid. In the AL type, the aim of the treatment is to suppress the synthesis of immunoglobulin light chains with chemotherapy control of the underlying hematological disease. Treatment studies with high doses of chemotherapy and stem cell transplantation have provided encouraging results, but the mortality rate remains high.3 In patients with localized disease with no specific systemic treatment, as in the case described, follow-up is recommended, although progression from localized to systemic disease is rare (2%).2 In type AA, treatment involves control of the primary disease, with remission of amyloid deposits and a decrease in the mortality rate.3 Surgical treatment is only indicated, as in this case, for the control of symptoms (abdominal pain not controlled by medical treatment) and complications (bowel obstruction).
Please cite this article as: Pérez X, Ramírez-Maldonado E, Martín C, Fumanal V, Urra I. Amiloidosis de colon y clínica de oclusión intestinal. Cir Esp. 2018;96:304–306.