The causes of occlusion of the inferior vena cava (IVC) are diverse and include thrombosis, agenesis or occupation by primary and secondary tumors.1 We present the description of an unusual case of IVC occlusion.
The patient is a 59-year-old woman with a history of arterial hypertension, who, while being studied for polycythemia, was incidentally diagnosed with thrombosis of the IVC during ultrasound. There was no lower limb edema. Thoracoabdominal CT angiography demonstrated iliac vein and IVC thrombosis extending to the right atrium. Anticoagulant therapy. MRI also identified a solid, well-defined mass adjacent to the uterus (Fig. 1). Given the suspicion of a gynecological tumor invading the IVC, tumor markers were requested, which were negative. Treatment was initiated with a selective progesterone receptor modulator (5 mg/24 h ulipristal acetate). One month later, the patient showed progressive clinical worsening with exertional dyspnea. Echocardiogram demonstrated a mobile echogenic image in the right atrium with no valve involvement. The case was assessed by a multidisciplinary committee, which indicated surgical treatment.
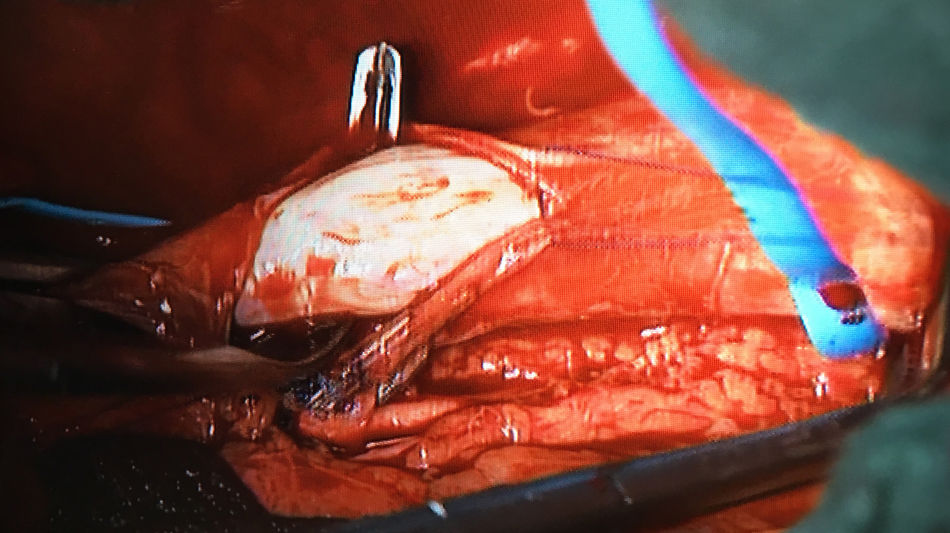
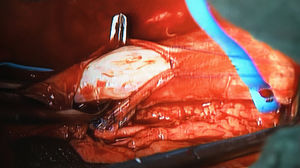
Due to the intracardiac extension, surgery was performed under cardiopulmonary bypass and moderate hypothermia (28 °C) in one surgical stage. Simultaneously, the vascular surgeon and the cardiac surgeon exposed the IVC at the infrarenal level and the right atrium using midline laparotomy and sternotomy, respectively. After the atriotomy, a free whitish solid mass was observed, and after cavotomy a whitish solid mass was observed, which was not adhered to the endothelium. The tumor was removed retrogradely from the cavotomy using continuous traction, with no resistance. A pearly tubular mass was removed (Fig. 2). After warming, hysterectomy was conducted by the gynecology unit with bilateral salpingo-oophorectomy. Prior to closure of the laparotomy, the patient suffered cardiac arrest with right-sided heart failure due to right ventricular akinesia. ECMO-type cardiac assistance was implanted, which was able to be removed 7 days after recovery of ventricular function. Associated pulmonary thromboembolism was ruled out. The patient presented progressive postoperative clinical improvement and was discharged to home 40 days after the intervention. The pathological results confirmed the diagnosis of intravenous leiomyomatosis (IVL) and ruled out malignancy. Six months later, the patient is asymptomatic, with no evidence of tumor recurrence on CT angiography.
IVL is a rare variant of uterine leiomyoma that is histologically benign. However, due to its ability to invade the lumen of adjacent veins, it can be considered malignant.2 It was first described by Birch-Hirschfeld in 1896, and the first cases of intracardiac leiomyomatosis were described in 1907.3 A total of some 400 cases of IVL have been published. Recently, Li et al. have published a series of 194 cases with intracardiac extension, all women with a mean age of 48 years; the majority had a history of uterine leiomyoma, and clinically symptoms included dyspnea, syncope and edema of the lower extremities.4
The diagnosis is usually made by Doppler ultrasound and confirmed with CT angiography and MRI. In case of intracardiac involvement, an echocardiogram is useful.5 In order to differentiate between venous thrombosis of the IVC and an occupying tumor, MRI is necessary because most IVL signals are similar to or slightly higher than those of muscle tissue in T1 and higher in T2. It can also show whether there is adhesion between the tumor and the vascular wall or the cardiac cavities. Therefore, it is important for the preoperative diagnosis, surgical planning and patient prognostic evaluation.6
The use of hormone therapy, as in our case, is based on studies that show the positivity of hormone receptors in tumor cells.7 However, the definitive treatment of this disease requires total surgical excision of the tumor.
The surgical strategy will depend on the tumor extension. In patients with intracardiac involvement, the most widely accepted surgery is complete removal of the tumor in one surgical stage. Hysterectomy and double oophorectomy are indicated in the same operation, although when to perform them is determined by the surgical team.8
Complete resection is essential to prevent disease recurrence, which is reported in 30% of cases.9 Since the most frequent extension pathway is the iliac vein, followed by the ovarian vein, all potential tumor extension pathways should be evaluated, including consideration of standard ligation of the internal iliac veins. The use of radiotherapy for recurrences has also been described. In our case, the absence of postoperative recurrence rules out this latter option.10
We conclude that IVL is a rare entity that can be life-threatening because of its ability to spread to the cardiac cavities. For this reason, it should be considered in patients with a history of uterine fibroids and diagnosis of inferior vena cava thrombosis. Treatment involves surgical removal of the tumor and hysterectomy with adnexectomy. The expected evolution is progression towards the cure of the disease, but follow-up is necessary for the early detection of recurrence, as described in the literature.
Please cite this article as: Huici-Sanchez M, Romera-Villegas A, Barahona-Opinell M, Rabasa-Baraibar JM, Vila-Coll R. Causa inusual de oclusión de la vena cava inferior. Cir Esp. 2020;98:106–107.