Learning surgical techniques is a dynamic process. In the 1980s David Kolb described developed a learning model that enabled teaching styles to adapt for better learner outcomes. The aim of this study was to identify the Kolb learning styles of the participants in a laparoscopic technical skills course and to check see if there was any relationship with performance.
MethodsAn observational descriptive study was conducted with 64 participants in an intensive course in which they performed laparoscopic manual intestinal anastomoses. All completed Kolb's inventory of learning styles. For each anastomosis, join quality was assessed and the performing time recorded. After that, they were analyzed through statistical studies.
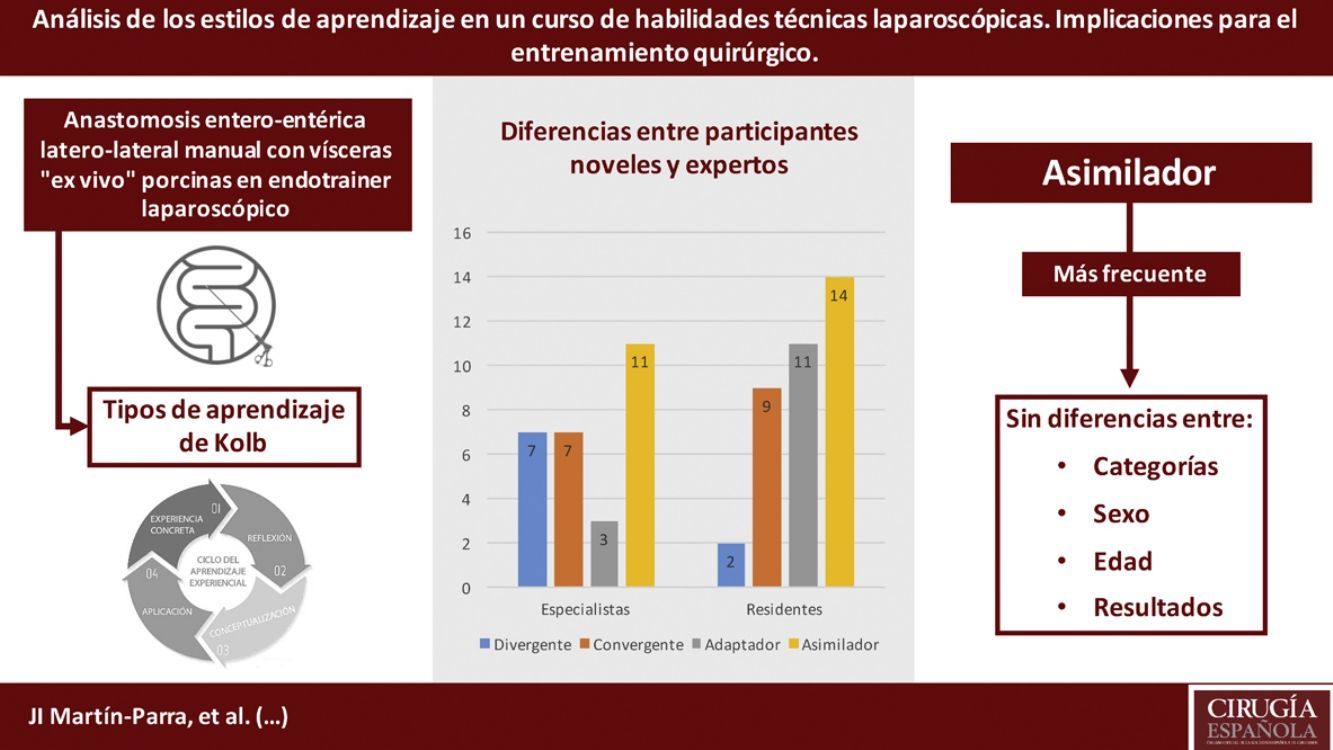
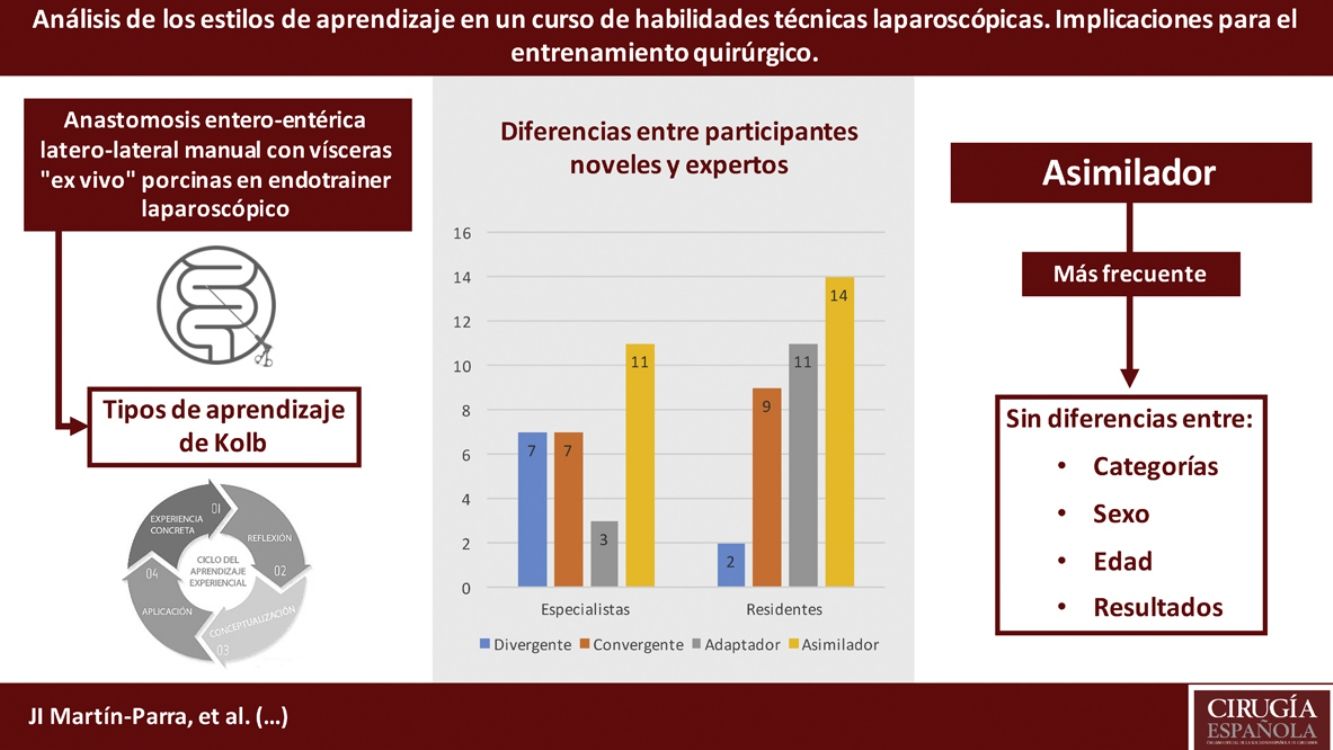
ResultsThe most frequent learning style was assimilating type (39.1%). No significant differences were observed between different learning styles and gender, professional category, the time taken or the quality of the anastomoses.
ConclusionsAssimilating type was the most frequent Kolb learning style, with no differences observed between categories, age or gender. There is no relationship between the learning style of the participants and the results obtained in the course.
El aprendizaje de las técnicas quirúrgicas es un proceso dinámico. David Kolb describió en los años ochenta un modelo de aprendizaje que permite adaptar el tipo de enseñanza y mejorar los resultados de esta. El objetivo del estudio es identificar los estilos de aprendizaje según Kolb de los participantes en un curso de habilidades técnicas laparoscópicas y comprobar si existe relación con el rendimiento final de la tarea realizada.
MétodosEstudio observacional descriptivo que incluye 64 participantes que completaron un curso intensivo donde realizaron anastomosis intestinales manuales laparoscópicas. Todos ellos completaron el inventario de estilos de aprendizaje de Kolb. En cada anastomosis se recogió el tiempo de ejecución y se valoró su calidad. Posteriormente, los datos fueron analizados estadísticamente.
ResultadosEl estilo de aprendizaje más frecuente fue el asimilador (39,1%). No se observan diferencias significativas entre los estilos y el sexo de los participantes, su categoría profesional, el tiempo en realizar la anastomosis o su calidad.
ConclusionesEl estilo de aprendizaje predominante es el asimilador, sin diferencias entre categorías, edad o sexo. No existe relación entre el estilo de aprendizaje de los participantes y los resultados obtenidos en el curso.
The adult learning process is considered a permanent change in behavior resulting from experiences1. It is an active and dynamic process. This idea from the world of pedagogy is perfectly applicable to the training of surgeons, as the cognitive abilities of participants in technical skills courses are relevant for the success of the learning experience. Therefore, understanding the different ways of learning of these participants can help us design a balanced teaching model that is useful for all students.
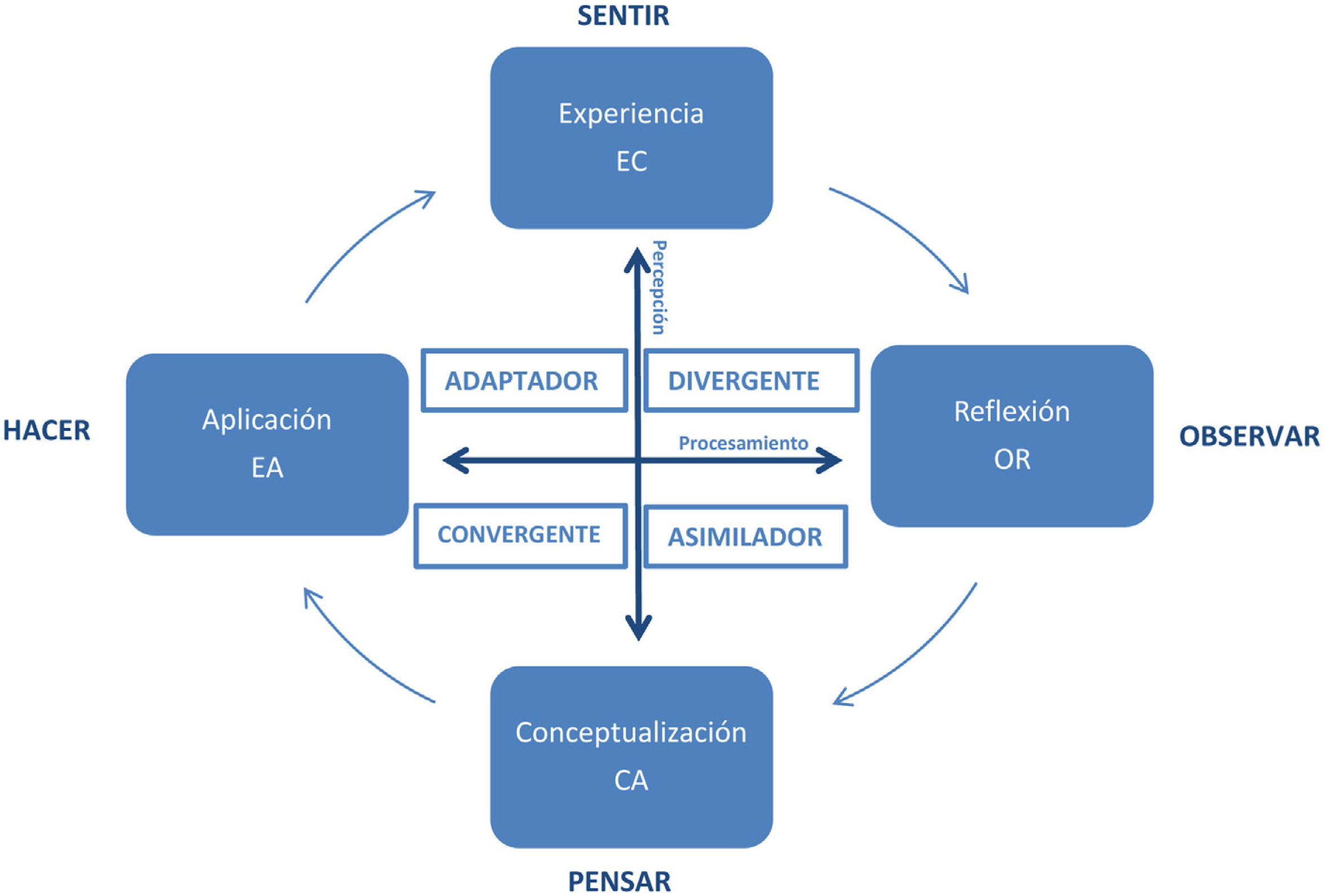
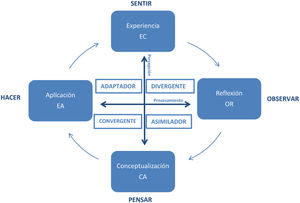
Since the middle of the 20th century, several authors have focused on the study of cognitive skills to achieve more effective learning. In 1984, David A. Kolb published his experience-based learning model, which proposed four learning styles that are closely related to the cognitive abilities of each individual2,3. This model identifies how students learn as a result of the way they perceive and then process what is perceived, which are the two main dimensions of the learning process: perception and processing. According to Kolb, perception is a process that encompasses a field between two opposite poles: people who perceive through concrete experiences, and people who perceive through abstract conceptualizations (generalizations). People then process what is perceived and transform it into knowledge in different ways, which also fall between two extremes: active experimentation, and reflective observation (Fig. 1).
Concrete experience (CE), reflective observation (RO), generation of abstract concepts based on reflection (AC) and active experimentation (AE) are part of the learning experience, which may start with any of them but typically begins with a CE. If we juxtapose the two ways of perceiving and the two ways of processing, we obtain Kolb’s Experiential Learning Method (ELM), from which four types of learners emerge:
- •
Converging: AC and AE. Active students who learn from a direct CE and are good at practical applications of ideas, using deductive reasoning for problem solving. Theorists: think and act.
- •
Diverging: CE and RO. Imaginative, reflective students who bring diverse views of things and excel in situations such as brainstorming. Active: experiment and reflect.
- •
Assimilating: AC and RO. Students who are more theoretical and are able to create models using induced reasoning. They systematize information into unifying theories or patterns. Reflective: think and reflect.
- •
Accommodating: CE and AE. They use perceived information to experiment and do things more than reading or studying about them. Pragmatists: experiment and act.
Each learning style highlights individual differences based on the preference for the different phases of the learning cycle (Fig. 1)3. Kolb indicates that an ideal learning process combines the four models and is more effective when the four parts of the cycle are experienced. Meanwhile, each student is different according to their personality, preferences and behavior4.
In the literature, several articles have studied the learning styles of residents from different medical specialties, mainly using VAK-type questionnaires and the Kolb Learning Styles Inventory (KLSI)3, which is undoubtedly the most commonly used. The objective is to evaluate and improve the learning process in the various contents of these specialties5–14.
Our hypothesis is that if each style presents peculiarities when it comes to learning, this could have implications in the design of training models and directly influence surgical teaching programs. Thus, if these learning styles were known, it would be possible to make adaptations and improve the outcomes.
The objective of this study is to use the KLSI adapted to Spanish in order to determine the most prevalent learning style among the participants in an intensive training course of an advanced laparoscopic surgical technique. We will compare the different Kolb learning types with the final performance of the task performed.
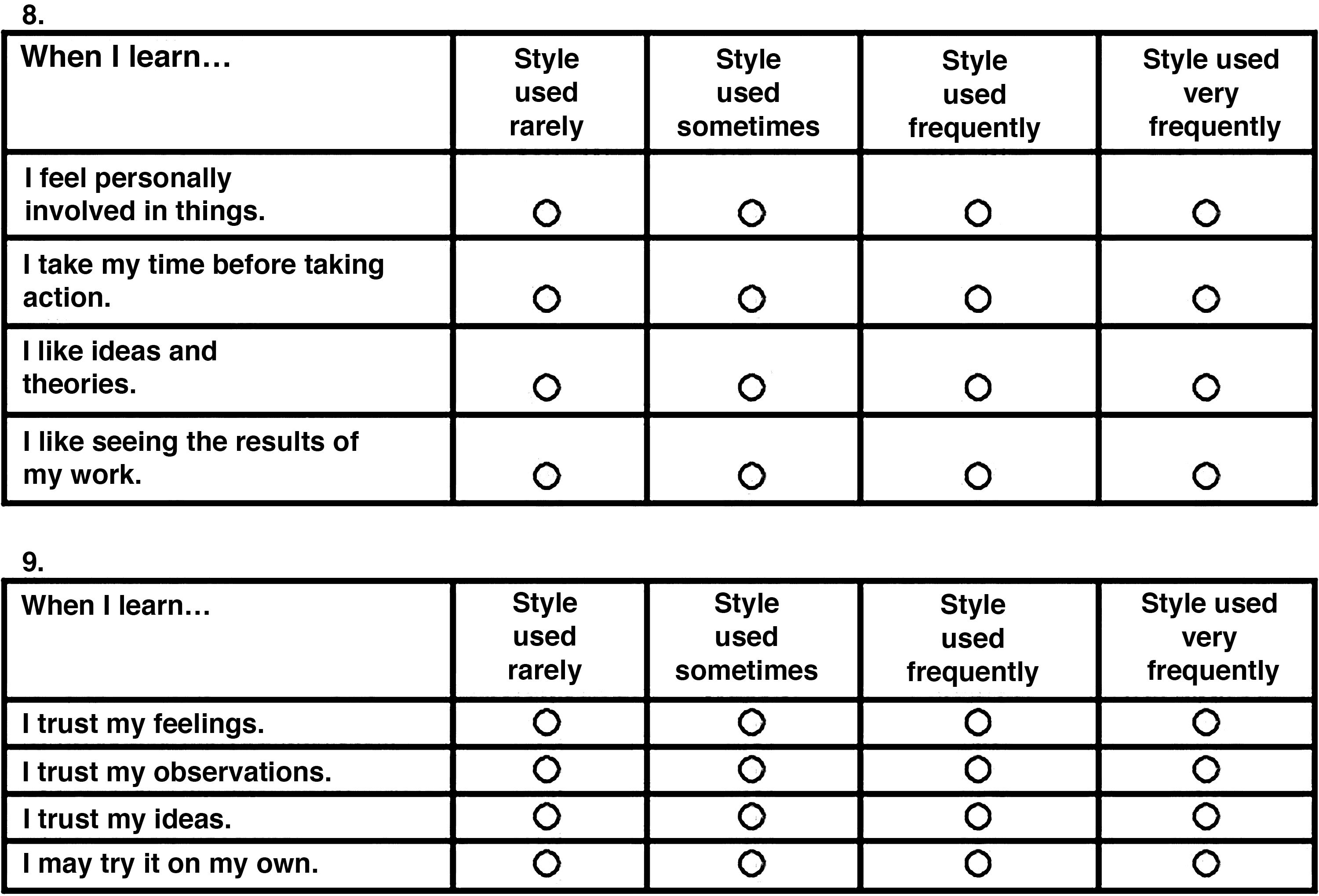
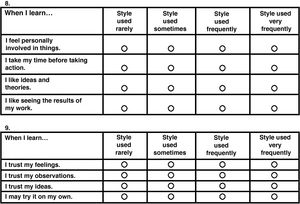
MethodsWe conducted an observational, descriptive study of general surgery surgeons and residents (4th and 5th year) participating in advanced laparoscopic skills training courses (50 h, 10 participants/course) at the Valdecilla Virtual Hospital (Santander, Cantabria, Spain) between June 2016 and November 2019. Participants were informed and consent was requested prior to completing the KLSI 3.1, adapted to Spanish (Korn Ferry® Group). The inventory consisted of 12 items with 4 possible answers. Each trainee ranked the possible endings to complete each sentence according to what was most similar to what s/he does when learning something, following a Likert-type verbal scale (Fig. 2). Participants were required to complete all the sentences, and two or more endings could not be assigned the same rank in a sentence.
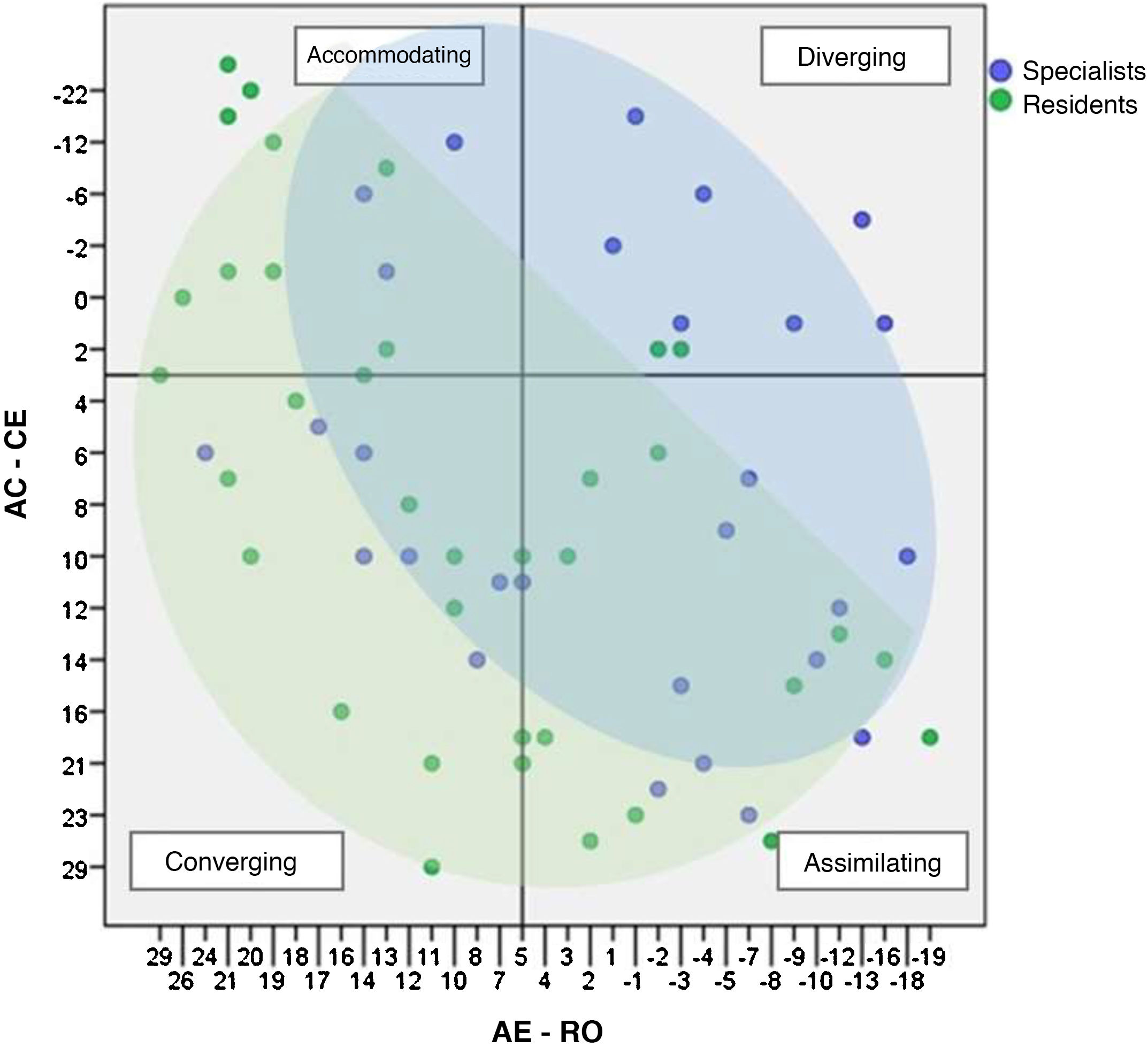
Subsequently, the four columns were added up: CE, RO, AC and AE. The relationship established between the four modalities was calculated using the formula: AC minus CE and AE minus RO; the obtained values were translated into a system or coordinates. The vertical axis represents the score of AC – CE, and the horizontal axis is the value of AE – RO. The quadrant of the generated point determines the learning style of the participant.
During the training sessions, manual laparoscopic side-to-side intestinal anastomoses were performed on ex vivo porcine viscera in a Pelvitrainer (Storz). The standard teaching methodology of the center was maintained during all the courses.
We evaluated the time, total number of anastomoses completed, and the quality of each. This quality was measured using a tool previously validated in our hospital15 that assesses separation between stitches, edge eversion, suture tension and leakage. Scores between 3 and 28 were given: low (3-11), moderate (12-19) and good (20-28) quality.
Statistical analysisThe IBM SPSS Statistics version 21.0 program (Chicago, USA, 2012) was used. A P value <.05 was considered statistically significant. The Kolmogorov-Smirnov test was used to determine the normal distribution of continuous variables. These variables were compared using the Student’s t test and ANOVA. For each subject, the values of each skill were quantified: CE, AC, RO, AE. The difference of AE – RO was represented on the X axis, and the AC – CE difference on the Y axis.
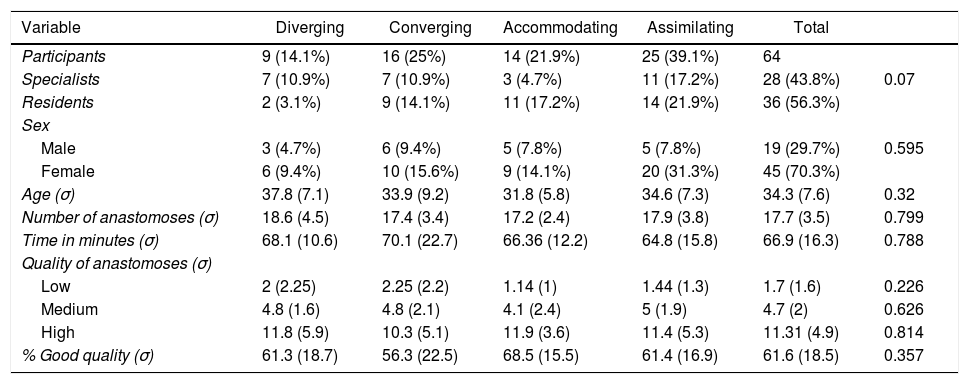
ResultsA total of 64 participants were included in the study: 28 specialists (43.8%, mean age 39.5 years), and 36 residents (56.2%, mean age 30.2 years). The participants were predominantly female (45 vs 19) in both groups. The specialists performed an average of 17.3 anastomoses and the residents 18 (P=.983), with mean times of 70 vs 64.6 min (P=.071); 56.5% were classified as ‘good quality’ (56.5% vs 65.6%; P=.05) (Table 1).
Table of descriptive variables of the population according to learning styles.
| Variable | Diverging | Converging | Accommodating | Assimilating | Total | |
|---|---|---|---|---|---|---|
| Participants | 9 (14.1%) | 16 (25%) | 14 (21.9%) | 25 (39.1%) | 64 | |
| Specialists | 7 (10.9%) | 7 (10.9%) | 3 (4.7%) | 11 (17.2%) | 28 (43.8%) | 0.07 |
| Residents | 2 (3.1%) | 9 (14.1%) | 11 (17.2%) | 14 (21.9%) | 36 (56.3%) | |
| Sex | ||||||
| Male | 3 (4.7%) | 6 (9.4%) | 5 (7.8%) | 5 (7.8%) | 19 (29.7%) | 0.595 |
| Female | 6 (9.4%) | 10 (15.6%) | 9 (14.1%) | 20 (31.3%) | 45 (70.3%) | |
| Age (σ) | 37.8 (7.1) | 33.9 (9.2) | 31.8 (5.8) | 34.6 (7.3) | 34.3 (7.6) | 0.32 |
| Number of anastomoses (σ) | 18.6 (4.5) | 17.4 (3.4) | 17.2 (2.4) | 17.9 (3.8) | 17.7 (3.5) | 0.799 |
| Time in minutes (σ) | 68.1 (10.6) | 70.1 (22.7) | 66.36 (12.2) | 64.8 (15.8) | 66.9 (16.3) | 0.788 |
| Quality of anastomoses (σ) | ||||||
| Low | 2 (2.25) | 2.25 (2.2) | 1.14 (1) | 1.44 (1.3) | 1.7 (1.6) | 0.226 |
| Medium | 4.8 (1.6) | 4.8 (2.1) | 4.1 (2.4) | 5 (1.9) | 4.7 (2) | 0.626 |
| High | 11.8 (5.9) | 10.3 (5.1) | 11.9 (3.6) | 11.4 (5.3) | 11.31 (4.9) | 0.814 |
| % Good quality (σ) | 61.3 (18.7) | 56.3 (22.5) | 68.5 (15.5) | 61.4 (16.9) | 61.6 (18.5) | 0.357 |
σ: standard deviation.
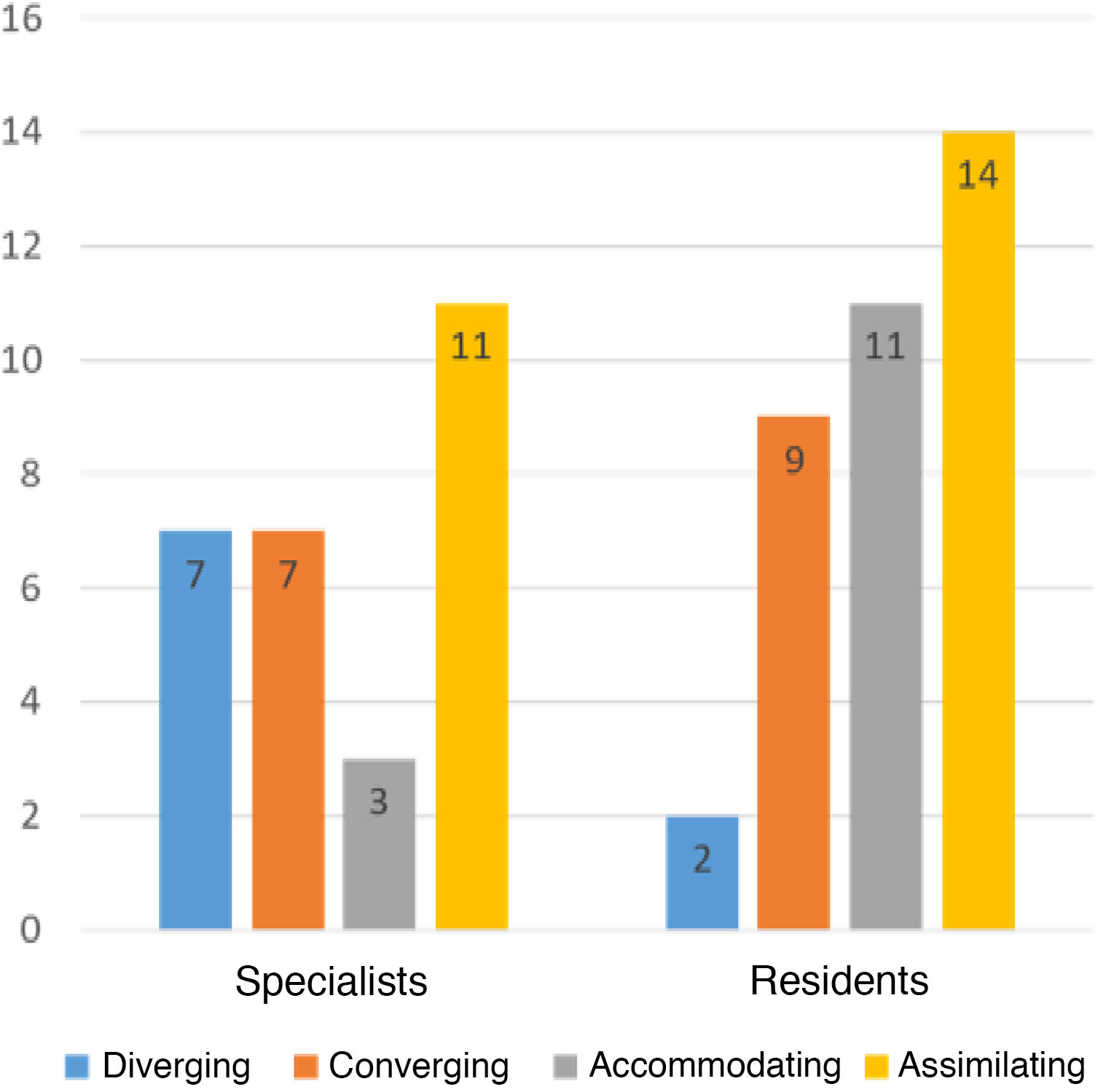
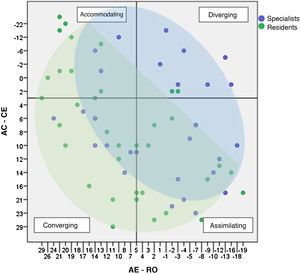
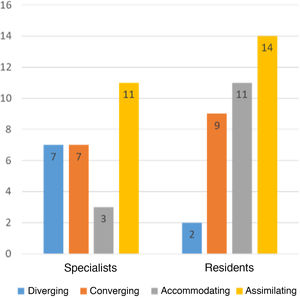
In Fig. 3, the participants are classified according to their learning style, and the ‘assimilating’ type was the most frequent in both groups (specialists 39.3%, residents 38.9; P=.974), followed by the ‘converging’ type (25% in both groups), ‘accommodating’ and, finally, the ‘diverging’ type, which was very rare among residents (5.6%). The specialists presented 10.7% accommodating vs 30.6% in residents (P=.057) and 25% diverging vs 5.6% (P=.026) (Fig. 4). No significant differences were observed between the different styles and the sex of the participants (P=.402), time to perform the anastomoses (P=.387) or the final quality of the anastomoses (P=.598).
Understanding the learning style of participants of training courses could make it possible to adapt the experience to each person, thereby increasing the effectiveness of these courses and positively affecting time, use of resources and the final outcome. The use of the KLSI to understand how people learn, with solid internal and external validation, is a tool widely used in education, psychology, business and other areas, such as the health sciences3. In this last category, there are publications that investigate university students of medicine7,8,14,16, nursing1,17 and different medical specialties, such as neurosurgery11, orthopedics9,18, pathological anatomy14, internal medicine8 or general surgery6,10,19. These studies have shown the a predominance of the converging learning style in general surgery residents. Mammen et al6 included 91 residents over a period of 12 years and showed the converging style was predominant (57%), followed by the assimilating style (18%). Another study in the same institution with 130 residents showed that the converging style was most frequent (49.7%)10.
In the literature, there are studies that show that the learning style of certain medical specialties (such as internal medicine8,20, pediatrics21, anesthesiology22 or psychiatry23) is different from the style of surgical specialties, but even the styles among these can differ. Lai et al11 studied 81 participants (neurosurgeons, neurosurgery residents and neurology residents) in Taiwan, finding that the most frequent styles were assimilating and diverging, which was different from general surgery residents, as we have seen before. However, the learning style of 13 first-year orthopedic residents in Ontario (Canada) was predominantly converging (53.8%)9.
The results of our study show that the majority of the training course participants showed an assimilating style (39.1%), followed by the converging style (25%) and the accommodating style (21.8%); the diverging learners were the minority (14.1%). There were no differences in terms of learning styles and age or sex. Some studies show a slight predominance of a learning style in each sex6, but most of them agree with us that sex does not make any difference, and the same is true for professional category (attending/resident)5,7,11,16.
Our results differ with previous publications, in which the converging style was predominant. This style is characterized by ‘thinking and acting’ (taking an active role in learning through specific experiences), which makes these learners good at the practical application of ideas and solving problems while making decisions. These learners would be perfect candidates for simulation learning, since it would fit perfectly with their way of perceiving and processing experiences11,24. Without a doubt, they are more attracted to tasks or technical problems than to people and interpersonal factors11. Contessa et al5 affirm that the work of a surgeon includes quick decision-making and problem-solving, which is consistent with the converging style being more frequent among them. Along the same lines, Modi et al25 indicate that this is consistent with the way surgeons transform their experiences, which is more likely to be with active experimentation than with reflective observation.
The results obtained in our study show that the assimilating learning style was the most frequent (39.1%), which is characterized by ‘thinking and reflecting’24, together with a well-structured understanding. These learners are concise and logical individuals who are able to take in a lot of information and structure it in a well-organized way. Their preferred methodology includes conferences and master classes rather than hands-on activities and having time to think carefully in order to create a structured model11. Lai et al11 help us try to explain this result on the basis that the complexity and difficulty of the tasks presented in our course require more than simple AE, making RO necessary to understand the different steps of the technique and thus be able to learn while overcoming the inherent difficulties of laparoscopic techniques. For this reason, at the Valdecilla Virtual Hospital we always advocate reflection on the practice carried out as a way to improve the training results (debriefing), which is a very important part of our educational methodology26.
The near absence of residents with a diverging style of learning is noteworthy (5.6%), while among surgeons this percentage is 25%, a finding that is repeated in the literature5,7,9–11,24. However, Ahmed et al14 recently observed that this is a frequent style among pathological anatomy residents that decreases as the years of residency progress and increases between fellows and pathologists. Perhaps this transition towards the converging style is due to the greater need to work within a team and incorporate different viewpoints during decision making.
When we compared the different styles with the performance and quality of the anastomoses performed in the laboratory, no correlation was found15, which could be due to the size of the sample or, as we have indicated before, it may be a task so complex that mastery of the skill requires all the perception and processing resources of the participants, making it difficult for one style to dominate over the others. According to our results, sex and professional category also do not influence a good final quality of the anastomosis. The tool used for the analysis of the anastomoses is effective in discriminating the novice participants from the experts15, without finding differences between professional categories due to the fact that it is an advanced skills course, and all the participants had a good level of laparoscopic technique.
Other studies, such as the Engels and Gara7 study with general surgeons and the Richard et al article18 with orthopedists, also did not find significant differences between learning styles depending on the professional categories.
Regarding the possible implications in training and program designs, the results obtained do not support the introduction of changes in the structure of the course depending on the participants’ learning style. However, if we look at Fig. 3, we observe that most of our participants are below the X axis (AE – RO), which means that they perceive the experience through AC. Participants who learn based on an experience theorize, classify or generalize that experience in an effort to generate new information, which generates new knowledge by identifying patterns and norms. This process is crucial when transferring knowledge from the laboratory to healthcare practice. Such reasoning will enable us to reinforce the actions that allow this majority of participants to optimize their learning experience through presentations, sending relevant documentation prior to the course, and emphasizing the instructor’s role as an expert and coach.
Learning is a complex process that is still being researched to complete our understanding of it. The theory of experiential learning offers a method to better understand how individuals learn based on the assumption that knowledge is shaped by the experiences of daily life. Thus, at this time it is very difficult to try to generalize the results of our study, since they would need to be validated. More studies are needed with much larger samples at more institutions, which is directly related to the limitations of this study: sample size, its single-center nature, and the variability and possible subjectivity of the anastomosis evaluations, despite using a validated tool and having a small group of instructors/evaluators (<10 people).
ConclusionsThe assimilating learning style is predominant, with no differences between professional categories, age or sex. There is no correlation between the learning style of the participants and the results obtained in the course.
FundingNone.
Conflict of interestsThe authors have no conflict of interests to declare. The Valdecilla Virtual Hospital is affiliated with the Center for Medical Simulation (Boston, MA, USA), both of which are non-profit educational institutions that offer clinical training programs and tuition education.
Please cite this article as: Martín Parra JI, Toledo Martínez E, Martínez Pérez P, Ruiz Gómez JL, Fernández Santiago R, López Useros A, et al. Análisis de los estilos de aprendizaje en un curso de habilidades técnicas laparoscópicas. Implicaciones para el entrenamiento quirúrgico. Cir Esp. 2021;99:730–736.