There is no standard procedure for the detection of the sentinel node (SN) in thyroid disease. However, the recent detection of the SN using a paramagnetic tracer is proving to be useful in breast cancer and melanoma. The objective was to assess the utility of super paramagnetic iron oxide tracer for the intraoperative detection of the SN in patients with papillary thyroid cancer without nodal involvement in the preoperative study.
MethodA single center, prospective pilot study of a class IIa medical device (a paramagnetic tracer). The study included thyroid cancers which were T1–T2 tumors in the cytohistological analysis with a negative preoperative nodal assessment, operated on consecutively during scheduled treatment. For the localization of the SN, an interlesional injection of 2mL of super paramagnetic iron oxide was administered. After 10min, ferromagnetic activity was detected in the adjacent nodes. Once the node had been detected, we proceeded by extracting it for intraoperative analysis. The effectiveness of the procedure for detecting the SN was assessed, with the main variable being whether it was detected or not.
ResultsThe project was assessed after the first cases had been carried out. The SN was located in all cases, which was done easily in the first four, but in the fifth case the SN detection was complicated by the interference of the reusable neurostimulation electrodes with the ferromagnetic signal. Intraoperative histology revealed the SN was positive in 80% (n=4) of cases (20% [n=1] were macrometastases and 60% [n=3] micrometastases). Total thyroidectomies were carried out, with central lymph node dissection in 4 of the patients and lateral in one due to the result of the detected SN. The histology showed the carcinoma was papillary, a classic type, in 80% (n=4) and a follicular variant in 20% (n=1). Forty percent (n=2) were multifocal, 40% (n=2) had vascular infiltration, and 60% (n=3) had extrathyroidal extension. Staging determined the application of radioactive iodine therapy (150mCi) in 80% of cases (n=4).
ConclusionsA paramagnetic tracer can be useful for detecting the SN and correctly staging papillary carcinoma.
La detección del ganglio centinela (GC) no se ha generalizado en la enfermedad tiroidea. Sin embargo, la recientemente detección del GC mediante trazador paramagnético está siendo útil en la cirugía del cáncer de mama y melanoma. El objetivo es evaluar la utilidad del trazador superparamagnetic iron oxide para la detección intraoperatoria del GC en el cáncer papilar de tiroides sin afectación ganglionar en el estudio preoperatorio.
MétodoEstudio piloto unicéntrico y prospectivo con un producto sanitario de clase IIa (trazador paramagnético). Se incluyen cánceres de tiroides que tras el análisis cito-histológico son tumores T1-T2 con resultado negativo en la evaluación ganglionar preoperatoria, intervenidos de forma programada y consecutiva. Para la localización del GC se realiza una inyección intralesional de 2ml de superparamagnetic iron oxide. A los 10minutos se procede a detectar actividad ferromagnética en los ganglios adyacentes. Una vez detectado el ganglio se procede a su extracción y análisis intraoperatorio. Se evalúa la efectividad del procedimiento con la detección de GC, siendo la variable principal la detección o no de mismo.
ResultadosSe evalúa el proyecto realizados los 5 primeros casos. Se localiza el CG en todos ellos, en los 4 primeros fácilmente, pero en el quinto fue dificultosa por su localización paratraqueal, que dio interferencias con el tubo endotraqueal con electrodos de neuroestimulación recurrencial. La histología intraoperatoria informó de GC positivo en el 80% (n=4) de los casos (20% [n=1] macrometástasis y 60% [n=3] micrometástasis). Se realizó una tiroidectomía total y el GC condicionó la realización de vaciamientos centrales (n=4) y un vaciamiento lateral. La histología informa de carcinoma papilar, tipo clásico en el 80% (n=4) y en el 20% (n=1) variante folicular. El 40% (n=2) eran multifocales, el 40% (n=2) presentaban afectación vascular y el 60% (n=3) extensión extratiroidea. La estadificación condicionó la aplicación de yodoterapia (150mCi) en el 80% de los casos (n=4).
ConclusionesEl tratador paramagnético puede ser útil para detectar el GC y estadificar correctamente el carcinoma papilar.
Papillary thyroid cancer is the most frequent thyroid carcinoma.1 The surgical treatment has been changing in recent decades. Although its treatment is supported with iodine therapy, surgical treatment is still the most effective.2
In this regard, inadequate treatment inevitably increases recurrences, but extended treatment significantly increases complications.2 Therefore, the indications for lateral-cervical lymph node dissections, and especially for the central compartment (level VI), are controversial, especially given the low rate of lymph node involvement in tumors with no evidence of involvement in the preoperative assessment.
Techniques have been tried with only the dissections necessary for lymph node involvement, avoiding the high percentage of negative dissections, with the associated high morbidity.
Although selective sentinel lymph node biopsy has been applied in malignant thyroid disease and appears to contribute toward better staging,3 most of the techniques used to detect sentinel nodes until now (most of which use radioactive isotopes) are tedious and increase costs and surgical time. Furthermore, their usefulness is questioned.4
Recently, the detection of sentinel lymph nodes by paramagnetic tracer has been applied in breast cancer and melanoma surgery with hopeful results.5–8 In addition, this method offers the advantage of being performed in the OR by the surgeon, without interfering with the surgical time.8–10 However, the technique has not yet been applied in thyroid disease.
The objective of this study is to evaluate the utility of paramagnetic tracer for the intraoperative detection of sentinel lymph nodes in patients with papillary thyroid cancer and no lymph node involvement in the preoperative study.
MethodsPatient selection. A prospective, single-center pilot study using a class IIa medical device with CE certification. Patients had been diagnosed with thyroid cancer after fine-needle aspiration cytology, identified as T1–T2 tumors according to the TNM classification of the AJCC and negative lymph node evaluation results during preoperative staging. Patients were treated surgically and consecutively at a tertiary-level referral hospital for endocrine surgery.
The inclusion criteria were:
- a)
Patients older than 8 years of age
- b)
Diagnosis of papillary thyroid cancer with cN0 result after clinical, ultrasound and cytohistological evaluation
The exclusion criteria were:
- a)
Previous systemic chemotherapy
- b)
Previous surgery in the cervical area, as this could alter lymphatic drainage
- c)
Intolerance or hypersensitivity to iron or dextran compounds of Sienna+®
- d)
Diseases involving a high concentration of iron in the organism (hemosiderosis, hemochromatosis, iron-deficiency anemia of metabolic or circulatory origin)
- e)
Pacemakers or other thoracic or cervical metal implants
- f)
Patients under treatment with iron-chelating agents
Validation of the series. This project was designed in the context of a workgroup with experience in this technique in other types of solid tumors who have contributed to the validation and clinical application of this sentinel lymph node detection technique, especially in breast cancer and melanoma. This study was conducted by specialists familiar with the selective sentinel node biopsy technique in other tumors (breast and melanoma) and, specifically, with the procedure using the ferromagnetic tracer. This is corroborated in the IMAGINE and IMINEM projects, which had been previously approved and developed at the same medical center.
Technique protocol. Once the lesion is exposed in the surgical field, patients receive an intraoperative, intralesional injection of 2mL of undiluted Sienna+® to locate the sentinel node. Ten minutes after the injection, ferromagnetic activity is detected in the lymph nodes adjacent to the thyroid gland. If no activity is detected, the measurement should be repeated 5min later. Due to the systematic use of neurostimulation in thyroid surgery, it is recommended that, when searching with the magnetic detection probe, the direction of the probe should be aimed as far away as possible from the trachea and always directed outwards; searching toward the esophagus can erroneously detect ferromagnetic activity due to the metallic components of the neurostimulation sensors. While measuring with the SentiMag® device, plastic surgical material is used to avoid placing any metallic elements near the SentiMag® probe.
Once the lymph node is detected, it is extracted. After excision, each marked lymph node is measured ex vivo with the SentiMag® probe, recording the measured values. Afterwards, the lymph node is analyzed by histology and immunohistochemistry, following the treatment protocol.
During the same surgical intervention, standard treatment of thyroid disease is performed by thyroidectomy, with or without lymphadenectomy, following standard management protocols. Any residual tracer that may have remained in the injection area is eliminated with the surgical piece during thyroidectomy.
Inclusion of patients and informed consent. Patients who potentially could have participated in the project were explained the objective, benefits and potential risks of the technique. If they accepted, their written informed consent was obtained.
As for possible side effects, to date there has been no evidence of adverse reactions derived from the interstitial injection (in the tissue) of Sienna+®. In some patients, skin discoloration, inflammatory response or hypersensitivity may occur at the injection site.
However, this project is distinctive because the non-migrated tracer was completely eliminated. As all the patients underwent thyroidectomy, any residual amount of the ferromagnetic tracer was removed from the patient, which decreased the possibility of side effects caused by the action of the tracer.
Sample size. Given that this is a pilot study to assess the effectiveness of a technique for the detection of sentinel lymph nodes, there was no quantifiable objective. An assessment of the results was to be made after recruiting 5 patients. If the results were favorable and the sentinel lymph node was detected in most of these cases, the series was to be extended to 10 patients.
Study variables. The project evaluated the effectiveness of the procedure in the detection of sentinel lymph nodes. The main variable was the detection or not of the sentinel lymph node.
Statistical AnalysisFor statistical calculations, all valid patients were used, meaning that they met the selection criteria of the study and the necessary data were available for the analysis of the main objective. The detection rate was studied by proportion analysis. In this pilot study, and for continuance in subsequent studies aimed at the practical clinical application of this technique, a value higher than 80% is considered valid.
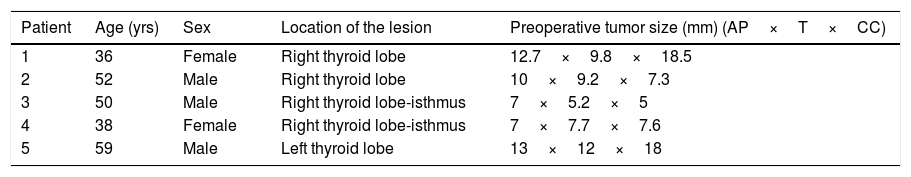
ResultsDescription of the series. The project was evaluated once the first cases were completed, which were 3 men and 2 women with an age range from 36 to 59 years, as shown in Table 1. The nodule containing the papillary carcinoma was located on the right side in 4 cases (80%) and on the left in the remaining case (20%). The preoperative assessment classified the lesions as T1aN0M0 in 3 cases (60%) and T1bN0M0 in the remaining 2 (40%).
Preoperative Data of the Patients Undergoing Sentinel Node Identification.
| Patient | Age (yrs) | Sex | Location of the lesion | Preoperative tumor size (mm) (AP×T×CC) |
|---|---|---|---|---|
| 1 | 36 | Female | Right thyroid lobe | 12.7×9.8×18.5 |
| 2 | 52 | Male | Right thyroid lobe | 10×9.2×7.3 |
| 3 | 50 | Male | Right thyroid lobe-isthmus | 7×5.2×5 |
| 4 | 38 | Female | Right thyroid lobe-isthmus | 7×7.7×7.6 |
| 5 | 59 | Male | Left thyroid lobe | 13×12×18 |
AP×T×CC: anteroposterior×transverse×craniocaudal.
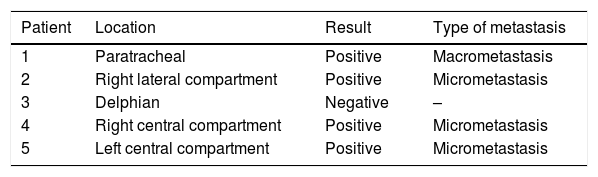
Detection of the sentinel node by paramagnetic tracer (Table 2). The sentinel lymph node was located in the 5 cases. In the first 4, localization was quick and confirmed in the surgical piece after excision. The fifth case was more difficult because of its location, which interfered with the endotracheal tube and the neurostimulation electrodes. This case required 4 biopsies for localization and extracorporeal confirmation.
Location and Histology Data of the Sentinel Lymph Node.
| Patient | Location | Result | Type of metastasis |
|---|---|---|---|
| 1 | Paratracheal | Positive | Macrometastasis |
| 2 | Right lateral compartment | Positive | Micrometastasis |
| 3 | Delphian | Negative | – |
| 4 | Right central compartment | Positive | Micrometastasis |
| 5 | Left central compartment | Positive | Micrometastasis |
The intraoperative histological results reported a positive lymph node in 80% (n=4) of the cases, 20% of which (n=1) presented macrometastasis and the remaining 60% (n=3) micrometastasis. The remaining patient (n=1; 20%) was negative for metastasis.
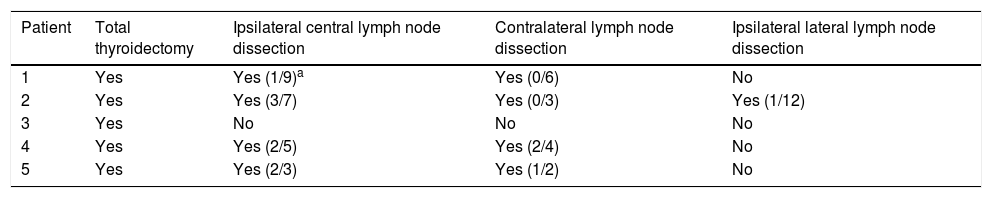
Surgery and results. In all cases, total thyroidectomy was performed. The results of the sentinel lymph node led to central lymph node dissection in the 4 cases of involvement and a lateral dissection in case 2, where the sentinel node was located in ipsilateral compartment IV. As shown in Table 3, lymph node involvement was observed in all the dissections completed.
Surgery Performed and Histology Results.
| Patient | Total thyroidectomy | Ipsilateral central lymph node dissection | Contralateral lymph node dissection | Ipsilateral lateral lymph node dissection |
|---|---|---|---|---|
| 1 | Yes | Yes (1/9)a | Yes (0/6) | No |
| 2 | Yes | Yes (3/7) | Yes (0/3) | Yes (1/12) |
| 3 | Yes | No | No | No |
| 4 | Yes | Yes (2/5) | Yes (2/4) | No |
| 5 | Yes | Yes (2/3) | Yes (1/2) | No |
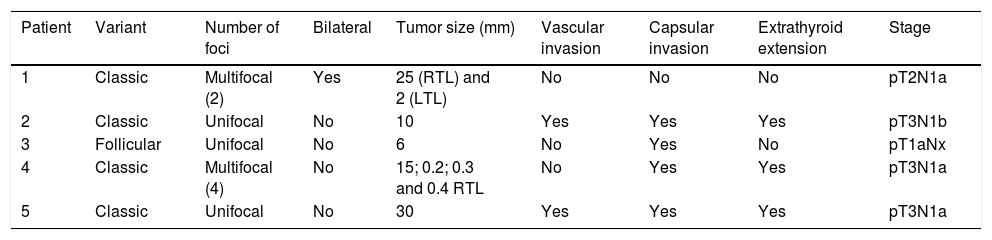
Final patient staging (Table 4). The definitive histological results reported papillary carcinoma: classic type in 80% (n=4), and a follicular variant in 20% (n=1). In 40% (n=2) the lesions were multifocal, in 40% (n=2) they presented vascular involvement and in 60% (n=3) extrathyroid extension.
Final Staging of the Papillary Carcinoma.
| Patient | Variant | Number of foci | Bilateral | Tumor size (mm) | Vascular invasion | Capsular invasion | Extrathyroid extension | Stage |
|---|---|---|---|---|---|---|---|---|
| 1 | Classic | Multifocal (2) | Yes | 25 (RTL) and 2 (LTL) | No | No | No | pT2N1a |
| 2 | Classic | Unifocal | No | 10 | Yes | Yes | Yes | pT3N1b |
| 3 | Follicular | Unifocal | No | 6 | No | Yes | No | pT1aNx |
| 4 | Classic | Multifocal (4) | No | 15; 0.2; 0.3 and 0.4 RTL | No | Yes | Yes | pT3N1a |
| 5 | Classic | Unifocal | No | 30 | Yes | Yes | Yes | pT3N1a |
RTL: right thyroid lobe; LTL: left thyroid lobe.
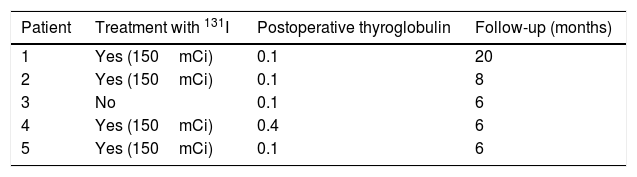
Adjuvant treatment and follow-up. Staging after sentinel lymph node and associated lymph node dissections indicated radioactive iodine therapy in 80% of the cases (n=4) of lymph node involvement, with a dose of 150mCi. The negative case did not require iodine therapy.
Currently, the follow-up is short but favorable, as can be seen in Table 5.
DiscussionIt is currently known that curing papillary thyroid carcinoma depends on early and adequate surgical resection. Recurrences are a factor for a poor prognosis, because they determine greater morbidity secondary to the disease, to surgery and to the side effects of the medical treatments administered, so the first step is not to leave active disease in the first surgery. However, sometimes the initial surgery is more aggressive than necessary, with unnecessary cervical lymph node dissections (both central and lateral-cervical), which entail unnecessary morbidity.11
The use of the sentinel lymph node technique has been generalized in tumors such as breast cancer or melanoma, with very favorable results.7,12,13 However, it has not become consolidated at the thyroid level.4
New techniques with paramagnetic tracer seem to improve the results in breast cancer,9 and our data show that it can be a simple technique to apply in the thyroid. It does not interfere with surgery and provides better intraoperative staging, while lymph node dissections can be more selective and effective. Notwithstanding, these are very preliminary results that require a greater contribution of cases and hospitals.
In the series presented, the high rate of sentinel lymph node involvement found in 80% of the cases is contrary to published reports for cases such as these, which were preoperatively assessed as T1a or T1b. However, we must clarify that ours is a short series of only 5 cases, with high risk patients such as men; meanwhile, the women presented multicentric disease, 40% vascular involvement and 60% extrathyroid involvement (T3). This aspect is quite remarkable and confirms the low utility of preoperative tests to assess metastatic involvement, especially in the central compartment (level VI) and in these cases where most were micrometastases. This confirms the need for tests like the sentinel lymph node, which allows us to identify cases of lymph node involvement.
A limitation of this technique is found in cases where the sentinel lymph node is located peritracheally, since neurostimulation of the recurrent nerve is currently used in most endocrine surgery units, and the electrodes interfere with the sentinel node signal. In this context, case number 5 of our series required 4 biopsies before being able to detect the affected node in the area of the recurrent nerve, where, by the time the lymph node was confirmed, most of the central lymph node dissection had already been performed.
In conclusion, sentinel lymph node identification with paramagnetic tracer is feasible and provides better tumor staging of patients with T1-2 and N0 papillary cancer in the preoperative assessment.
AuthorshipStudy concept and design: A. Ríos, J.M. Rodríguez and A. Piñero
Data collection: A. Rios and N. Ibañez
Analysis and interpretation of the data: A. Rios, J.M. Rodríguez and A. Piñero
Article draft: A. Rios and J.M. Rodríguez
Critical review of the manuscript; important intellectual content: A. Rios, J.M. Rodriguez and P. Parrilla
Statistical expertise: A. Rios and N. Ibañez
Supervision: A. Rios and J.M. Rodriguez
Approval of the final version for publication: A. Rios, J.M. Rodriguez, N. Ibañez, A. Piñero and P. Parrilla
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Ríos A, Rodríguez JM, Ibañez N, Piñero A, Parrilla P. Detección del ganglio centinela mediante trazador paramagnético en el cáncer de tiroides. Estudio piloto técnico. Cir Esp. 2019;97:169–174.