Bile duct injury is one of the most severe complications after cholecystectomy. The aim of this study is to demonstrate how with a simple technique, an optimal critical view may be achieved by injecting indocyanine green directly into the gallbladder.
MethodsTwenty-three patients were prospectively studied in which direct gallbladder injection of indocyanine green during laparoscopy was administered with a fine needle using an easily reproducible technique.
ResultsBiliary tree identification was reported before and after injection. Critical view of safety was achieved in all cases.
ConclusionsOur technique of direct gallbladder injection of indocyanine green is simple, efficient and shows a real time fluorescent cholangiography and an optimal critical view of safety decreasing the risk for bile duct injury.
La lesión de vía biliar continúa siendo una de las complicaciones más graves tras la colecistectomía. El objetivo de este estudio es mostrar una técnica sencilla para la administración del verde de indocianina intravesicular, consiguiendo una visión crítica óptima durante la colecistectomía laparoscópica.
MétodosSe estudiaron prospectivamente 23 pacientes con administración intravesicular de verde de indocianina con aguja fina utilizando una técnica fácilmente reproducible.
ResultadosSe reportó la visión de las estructuras biliares antes y después de su administración. La visión crítica de seguridad se consiguió en todos los casos.
ConclusionesLa administración intravesicular de verde indocianina mediante la técnica que describimos es sencilla, efectiva y consigue una colangiografía por fluorescencia en tiempo real y una visión crítica de seguridad óptima, disminuyendo así el riesgo de lesión biliar.
Bile duct injury continues to be one of the most serious complications after laparoscopic cholecystectomy1. To reduce its incidence, it is essential to achieve the criteria for a ‘critical view of safety’ described by Strasberg2. However, to date, this objective has not always been achieved or carried out correctly. Thanks to its exclusive biliary excretion, indocyanine green (ICG), previously used in our field of medicine to measure liver function, also began to be used to identify the bile duct3. Its first intravenous use for this purpose was described in 2009 when a fluorescent cholangiography of the extrahepatic bile duct was performed successfully4. Several publications continued to confirm its usefulness for laparoscopic cholecystectomy5,6, even considering it comparable with intraoperative cholangiography7. In order to avoid the disadvantages of its intravenous use (such as simultaneous fluorescence of the liver), direct injection of ICG into the gallbladder has recently been described as a technical variant8–10. However, this technique has been reported few times in the literature, with no description of a standardized technique. The objective of this study is to describe a simple, effective and reproducible technique for direct gallbladder ICG injection that achieves an optimal critical view of safety during laparoscopic cholecystectomy.
Methods, surgical technique and resultsData were prospectively collected from 23 patients who underwent laparoscopic cholecystectomy between November 2019 and October 2020. The inclusion criterion was to be a candidate for laparoscopic cholecystectomy due to symptomatic cholelithiasis or acute cholecystitis. Patients with a diagnosis of gallbladder cancer were excluded. Out of the 23 patients, 12 were men and 11 women, with a median age of 58 years (26–80) and a body mass index of 24 kg/m2 (21–30). All were ASA I-II, with hypertension and type 2 diabetes mellitus being the most frequent comorbidities. The surgical indication was symptomatic cholelithiasis in 20 cases and acute cholecystitis in 3. We used the Pinpoint fluorescence endoscopic imaging system (Novadaq/Stryker®) for the procedure, as described below.
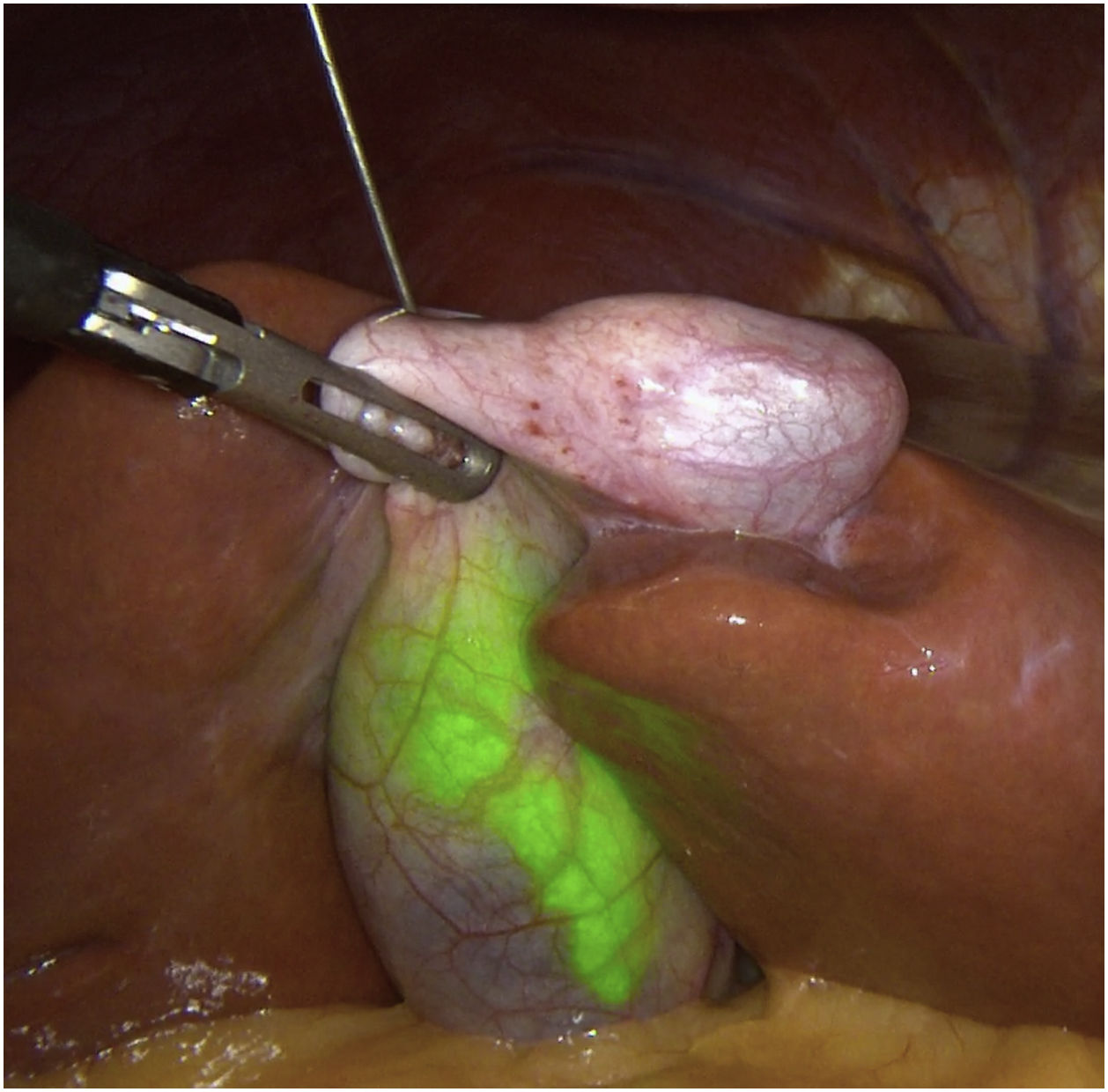
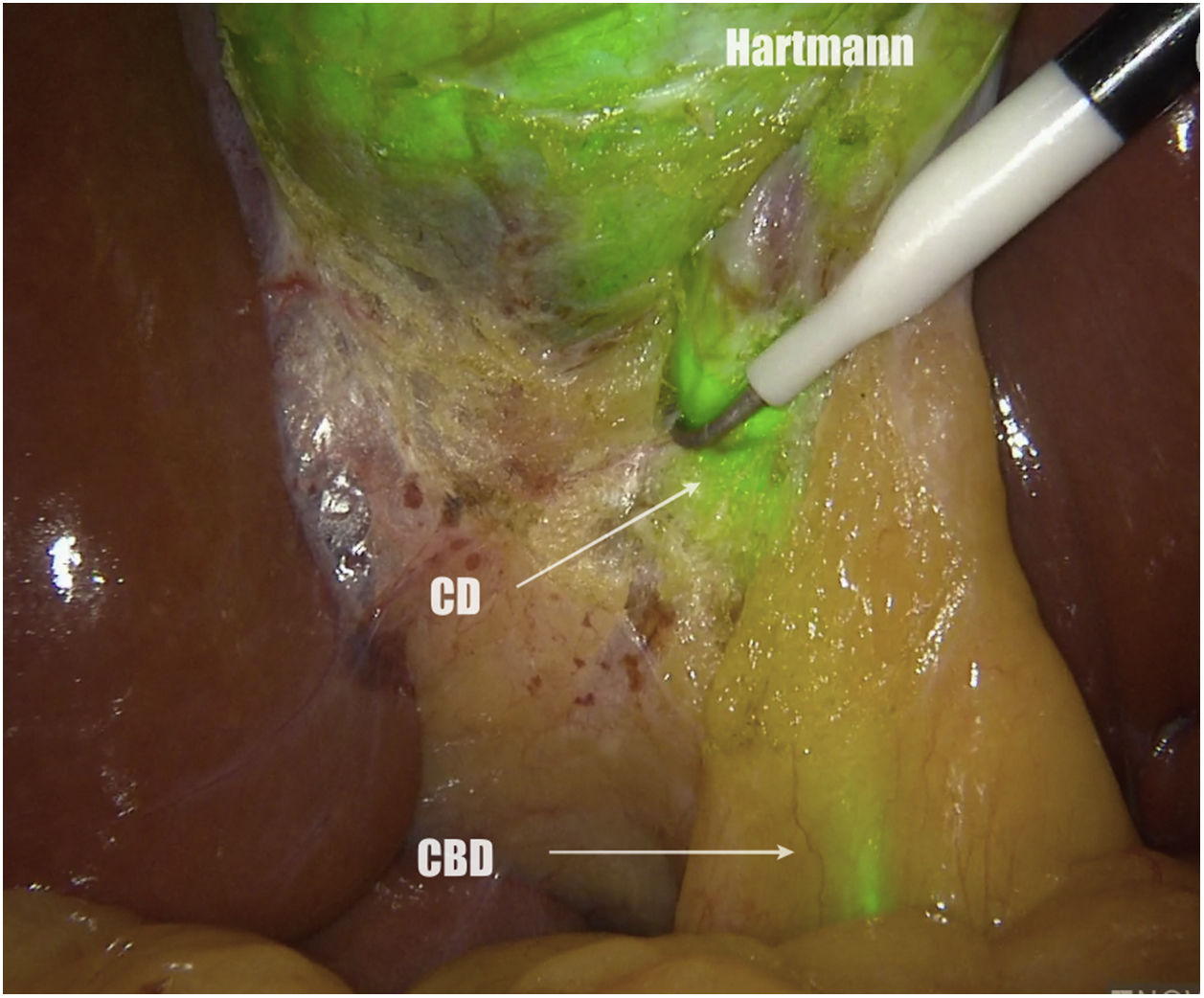
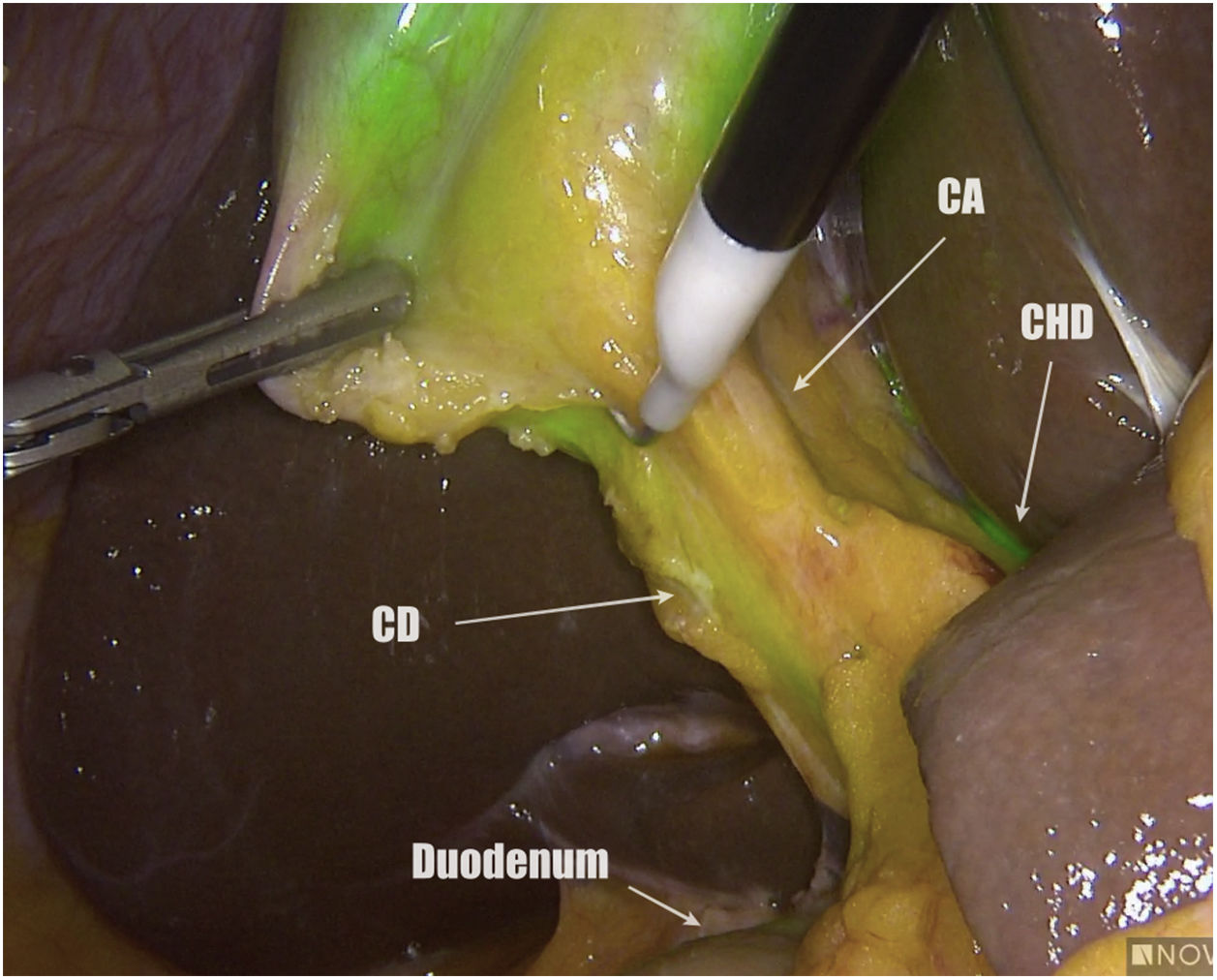
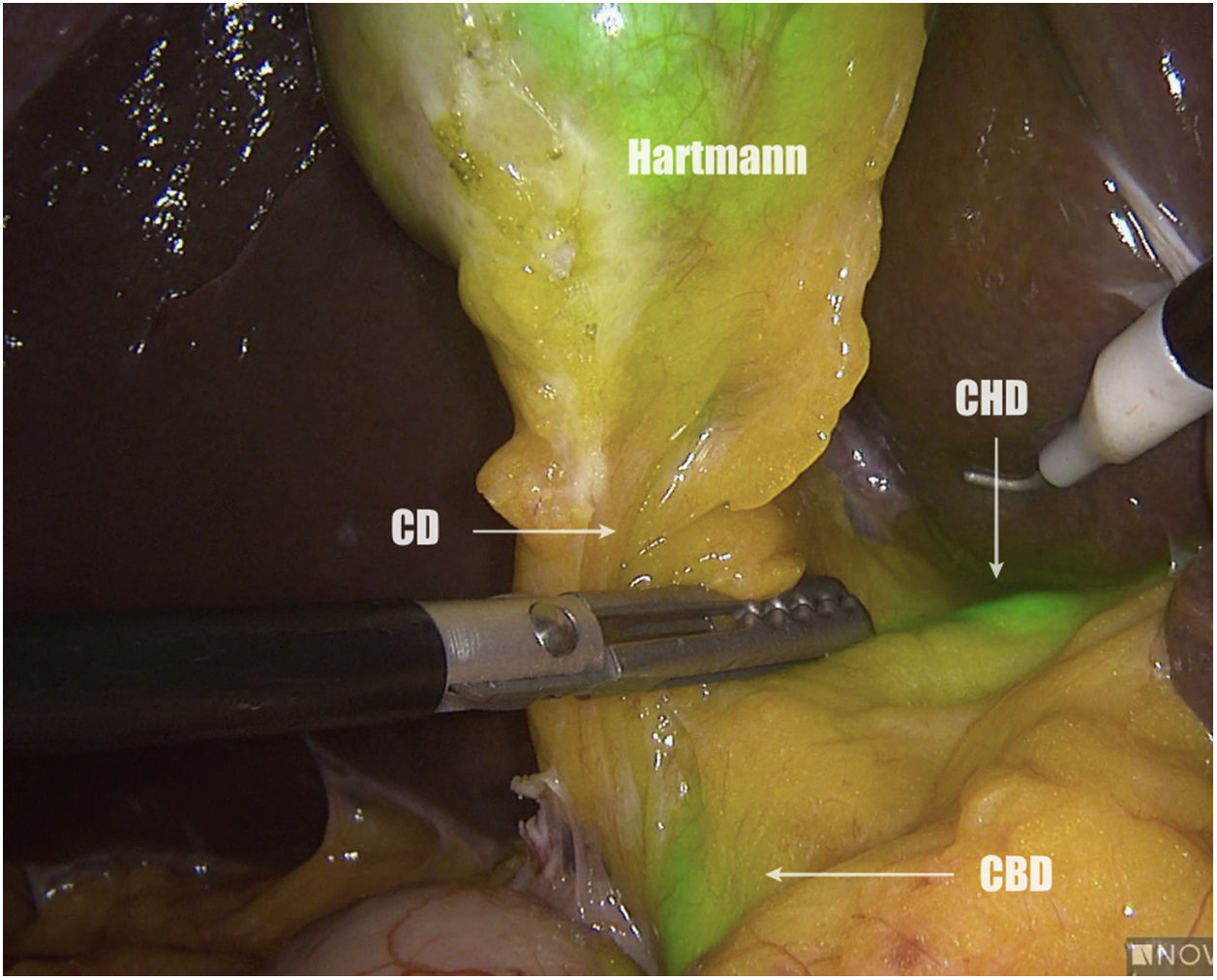
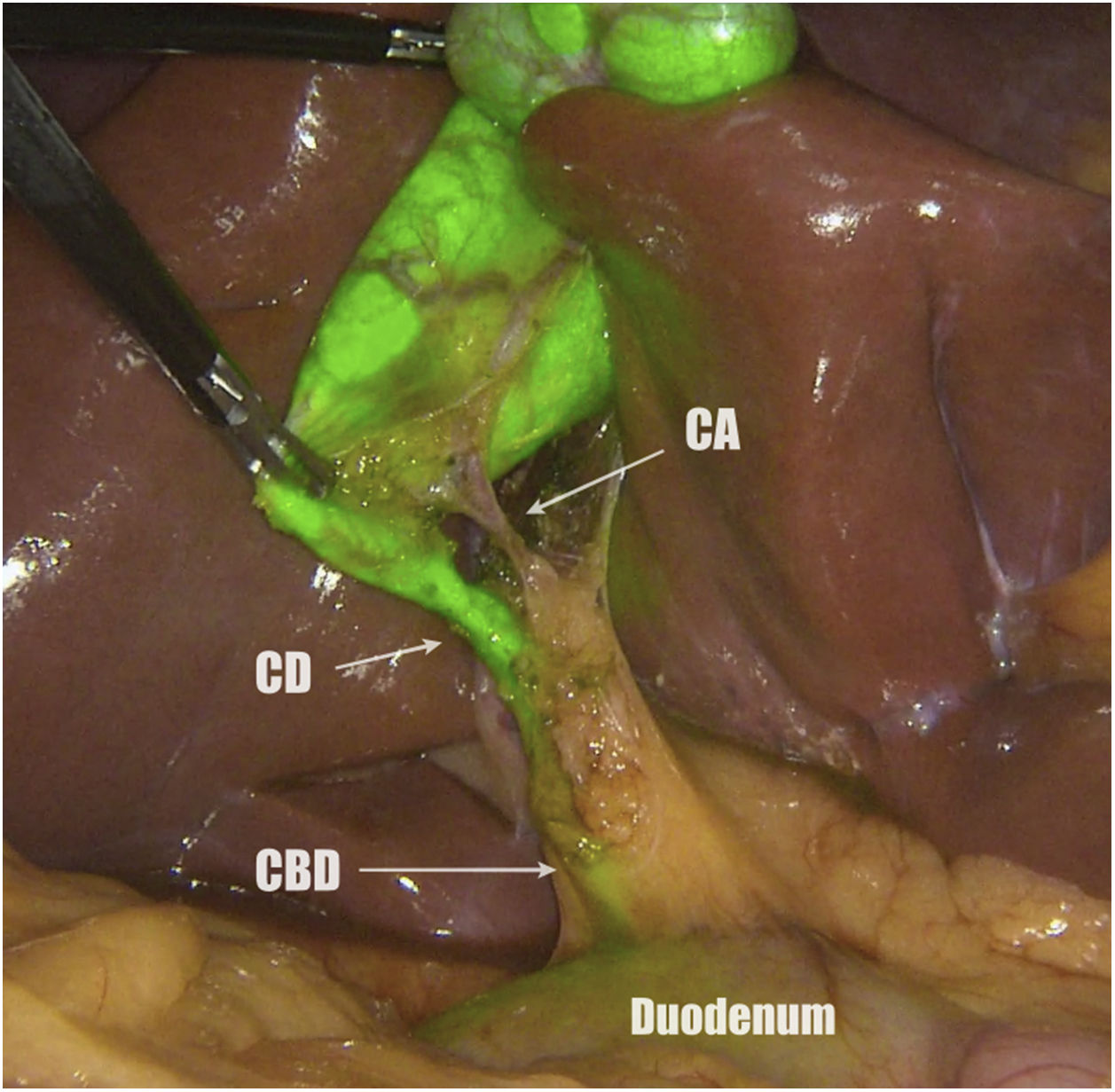
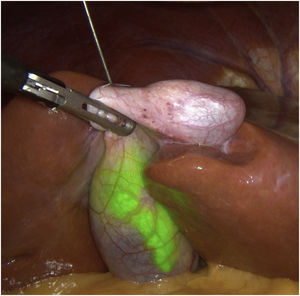
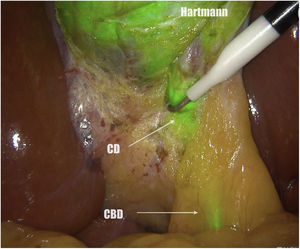
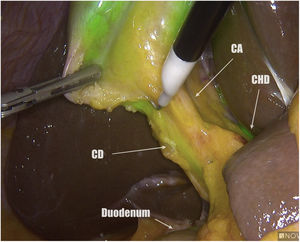
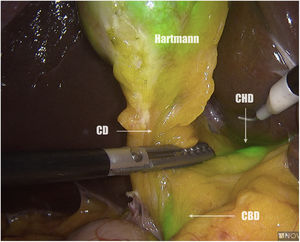
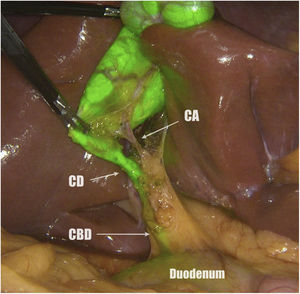
All patients are placed in the American position, and 4 trocars are used (11-mm umbilical for 30° optics, 12-mm epigastric, and two 5-mm in the right flank). The first step is to identify the cystic duct (CD), the common bile duct and the common hepatic duct (CHD) prior to ICG injection. The ICG (Verdye 25 mg) is diluted in 10 mL of distilled water, obtaining a concentration of 2.5 mg/mL. The gallbladder is brought closer to the abdominal wall in the right subcostal region, and percutaneous puncture is performed under direct vision in the fundus using a 22 G epidural needle (Spinocan, Braun®) (Fig. 1). The necessary dose is administered until satisfactory fluorescence is achieved, as determined by the surgeon. In our study, said dose varied between 2 and 4 mL, depending on the density of the bile. We use forceps to close the small puncture hole and pull the gallbladder cranially. Then, before starting the dissection, we again assess the bile structures. We always start the dissection on the posterior side of Calot’s triangle (Fig. 2). Once the widest possible posterior dissection is achieved, we continue the dissection anterior to the triangle, guided by fluorescent cholangiography (Fig. 3) and succeeding to identify not only the CD and the cystic artery, but also the common bile duct and CHD (Fig. 4). Finally, we separate the gallbladder from the cystic plaque to achieve a critical view of safety (Fig. 5) and divide the cystic duct and artery between clips.
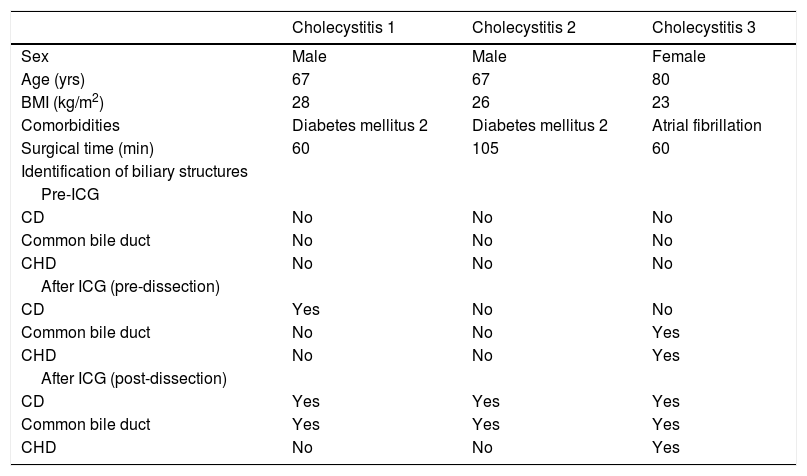
Prior to the administration of ICG in one case, the CD and CHD were visualized, and in 6 cases the common bile duct was observed. After its administration, and prior to initiating dissection, the CD was identified in 17 cases, common bile duct in 15 and CHD in 7. After initiating dissection, the CD was identified in all case, the common bile duct in 21, and the CHD in 11. The critical view of security was achieved in all cases. The 2 patients in whom the common bile duct could not be visualized after the dissection of Calot’s triangle was due to abundant fatty tissue, despite having a BMI < 25 kg/m2. Regarding the 13 patients in whom the CHD was not visualized after dissection, they are a heterogeneous group with demographic characteristics similar to the total population. The characteristics of the patients with acute cholecystitis are specified in Table 1. Out of the 23 patients, the median surgical time was 45 min (20–105), without any intraoperative complications. One patient had trocar bleeding as a postoperative complication, and all patients had a postoperative stay of 24 h, except for cases of acute cholecystitis (72 h) and the hemorrhage of the trocar (5 days).
Characteristics of pacients with acute cholecystitis.
| Cholecystitis 1 | Cholecystitis 2 | Cholecystitis 3 | |
|---|---|---|---|
| Sex | Male | Male | Female |
| Age (yrs) | 67 | 67 | 80 |
| BMI (kg/m2) | 28 | 26 | 23 |
| Comorbidities | Diabetes mellitus 2 | Diabetes mellitus 2 | Atrial fibrillation |
| Surgical time (min) | 60 | 105 | 60 |
| Identification of biliary structures | |||
| Pre-ICG | |||
| CD | No | No | No |
| Common bile duct | No | No | No |
| CHD | No | No | No |
| After ICG (pre-dissection) | |||
| CD | Yes | No | No |
| Common bile duct | No | No | Yes |
| CHD | No | No | Yes |
| After ICG (post-dissection) | |||
| CD | Yes | Yes | Yes |
| Common bile duct | Yes | Yes | Yes |
| CHD | No | No | Yes |
CD: cystic duct; CHD: common hepatic duct; BMI: body mass index; ICG: indocyanine green.
The main objective of using ICG for intraoperative fluorescent cholangiography during laparoscopic cholecystectomy is to create a visual map to safely perform biliary dissection, identify anatomical variants and reduce the incidence of biliary lesions.
There are currently 2 methods of administration. The first reported method was the intravenous route4. Most studies on the use of ICG in laparoscopic cholecystectomy use intravenous administration and report successful identification of biliary structures and their benefits. However, one of the most relevant disadvantages described is the intensity of liver fluorescence, which makes it difficult to distinguish the biliary tree. Furthermore, due to the exclusive biliary excretion of ICG, intravenous administration is a problem in patients with liver dysfunction or biliary excretion problems, since this considerably limits the flow to the common bile duct and, therefore, its visualization. Another limitation is that ICG has visualization capacity in tissues of less than 10 mm thick11, so this could be a drawback in patients with abundant adipose tissue. Direct gallbladder injection of ICG completely solves the problems of liver fluorescence and poor biliary excretion, while significantly increasing the intensity of intraductal-only fluorescence, improving visibility even in patients with abundant fatty tissue. According to the latest reports from the EURO-FIGS registry, there is great disparity in the protocols used for the use of ICG in laparoscopic cholecystectomy, mainly in the dose and time of administration12. It should be noted that, in this registry, ICG was administered directly into the gallbladder in only 2 out of 314 cases.
With regard to direct gallbladder injection techniques, the first description was in 2017 by Graves et al.8 and Liu et al.9 In the same article, Graves described 2 options for injection. The first is into the infundibulum by introducing a cholangiography or pigtail catheter through the umbilical trocar (together with the optics), aspirating the bile to mix with ICG and reinject into the gallbladder, withdrawing the catheter and closing the hole with a clamp. The second technique is fundus puncture following a Seldinger technique, using the same catheters. Liu used both gallbladder catheters inserted prior to surgery and intraoperative puncture with a Veress needle in the fundus and tobacco pouch suture of the orifice. In their results, they report an extravesicular ICG leak in 5 out of 28 cases (17.8%), which, according to their own description, makes correct evaluation impossible.
The goal of our fine-needle injection technique is to offer a simple, easily reproducible and effective method. As we can see, the main drawback of the use of direct gallbladder ICG injection is the possibility of leakage into the abdominal cavity, since fluorescence in the surgical field makes it impossible to differentiate biliary structures13. By performing the fine-needle puncture as described, we minimize the appearance of this problem. In no case in our series did dye leakage compromise the identification of the biliary structures. However, only 3 patients in our study had acute cholecystitis. Before describing our series, the situation in which we had the greatest difficulty in obtaining a successful cholangiography was in these patients. The distention of the gallbladder and the thickening of the walls make it difficult to hold and, in many cases, leads to the need for emptying with a Veress-type core needle. In these cases, the possibility of ICG leak is higher, and therefore the possibility of a successful cholangiography decreases. The advantages and disadvantages of intravenous versus direct gallbladder administration should be specifically studied in cases of acute cholecystitis, particularly in hydropic gallbladders with very thickened walls and multiple large stones inside. We are currently conducting a comparative study to evaluate the intravenous versus direct gallbladder fine-needle techniques in these patients.
Lastly, direct gallbladder injection perfectly delimits the liver bed dissection plane (Fig. 6), offering an interesting field for teaching, as it could speed up the learning curve for residents.
In conclusion, gallbladder injection of ICG by the fine-needle puncture technique is quick, simple and effective. It achieves real-time fluorescence cholangiography that allows for the identification of bile structures and a critical view of optimal safety, consequently reducing the risk of biliary injury.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Cárdenas G, Fornaguera I, Díaz del Gobbo R, Ginestà C. Técnica de punción de verde de indocianina intravesicular para conseguir una visión crítica de seguridad durante la colecistectomía por laparoscopia. Cir Esp. 2021;99:678–682.