Fecal incontinence is one of the leading causes for the institutionalization of people in the last decades of life, associated with a great psychosocial and economic burden. The literature is scarce in this population group, due to the absence of universally accepted criteria to define “elderly patients” and difficulties in detection and diagnostic. The aim of this article was to conduct a narrative review of the main aspects related to fecal incontinence in older patients, providing management support. Toileting assistance, dietary change, controlling stool consistency and medical treatment can be used to treat these patients. Nevertheless, other therapies, such as biofeedback, neuromodulation or surgical treatment, can be considered in selected patients.
La incontinencia fecal representa una de las principales causas de institucionalización en las últimas décadas de la vida de una persona, asociando además gran repercusión psicosocial y económica. La literatura muestra escasa evidencia cuando se trata de analizar de forma específica a este grupo de población, debido a la falta de uniformidad en la consideración de «paciente anciano» y en la dificultad de su detección y diagnóstico. El objetivo de este artículo ha sido realizar una revisión narrativa de los principales aspectos relacionados con la incontinencia fecal en el anciano y facilitar el manejo de estos pacientes. La asistencia para la defecación, las modificaciones dietéticas y el control de la consistencia de las deposiciones o el tratamiento farmacológico son en muchos casos medidas suficientes. No obstante, otras terapias como el biofeedback, la neuromodulación o el tratamiento quirúrgico no deben descartarse y han de ser valoradas de forma selectiva en pacientes ancianos.
The elderly population does not constitute a homogeneous group, and in many cases its exact definition varies according to the bibliographic reference and the country studied. The World Health Organization considers the age brackets from 60 to 74 years early old age, 75 to 90 older old or elderly, and over 90 oldest old or oldest elderly.1 Fecal incontinence (FI) is a syndrome that has great psychological impact and an enormous effect on the quality of life of geriatric patients and caregivers. Moreover, the economic cost and expenditure of resources involved in its treatment make it a major problem for the social healthcare system.2 In fact, FI is considered a negative marker in health, as affected patients present elevated mortality rates.3 The treatment of FI in these patients must integrate a combination of habit modification, hygienic-dietary measures, medications and, to a lesser extent, surgery.
Despite the high incidence of fecal incontinence in elderly patients, there are few studies specifically related to this age group. This article answers questions that frequently arise in the comprehensive management of these patients. A non-systematic search was conducted in the MEDLINE, Cochrane Library, SCOPUS, ISI Web of Science and Ovid databases, identifying articles published between 1992 and May 2017 referring to patients older than 65 years of age and using the following keywords
“fecal incontinence” AND “elderly” (“conservative therapy” OR “surgical treatment”).
Prevalence and Healthcare Costs of Fecal Incontinence in Older PatientsThe prevalence of fecal incontinence in the elderly is very variable among published series, mainly due to the different populations studied and lack of consensus in the definition of FI, including in many cases the involuntary loss of mucus. Despite this underdiagnosis, it is estimated to affect between 3% and 21% of patients over 65 years of age in the general population, more than 50% of institutionalized patients and more than 80% of hospitalized patients with dementia. This broad epidemiological population study determines that its prevalence increases significantly in the three age groups studied: 65–74 (3%), 75–84 (5.3%) and older than 85 (8.2%) and that age represents a risk factor due to its presentation regardless of comorbidity.4
These data have a lower prevalence than those published in a study conducted in the metropolitan area of Barcelona with direct interviews of 518 patients that evaluated FI in patients treated at primary care centers; statistically significant differences were observed according to age (2.8% in patients under 45 years, 11.3% in those between 45 and 65 years, and 14.1% in patients over 65 years of age).5 These differences with other studies were explained by the authors because of the study population, since it include patients who went to the Health Center for various reasons and were usually older and more pathological than the baseline population. In younger people, FI is more frequent in women, although this prevalence equals out between the ages of 70 and 80, then becoming higher in men after the age of 80.6 According to data from the Ministry of the Interior, in Spain the use of protectors is equivalent to 3% of the pharmaceutical expenditure of the National Healthcare System, making them the healthcare product with the highest consumption (43.6% of total packages).7 In addition, in Primary Care, this represents an increase of 55% in the healthcare costs for these patients.8 These figures are difficult to individualize, since it is estimated that approximately 65% of patients with fecal incontinence also have urinary incontinence and that FI associated with urinary incontinence is 12 times more frequent than isolated fecal incontinence.9
Predisposing Factors for the Appearance of Fecal Incontinence in Elderly PatientsThe etiology of FI is multifactorial. The risk factors that contribute most to its presentation in the elderly population include: immobility, presence of acute or chronic diarrhea, constipation and fecal impaction, laxative use, polypharmacy, low level of consciousness, dementia, cerebrovascular disease, Parkinson's disease, pelvic floor laxity, rectal prolapse, anal sphincter injury or altered anorectal sensitivity.10,11 Despite our greater understanding of the mechanisms involved in continence, there is still no clear concept of the biological and pathophysiological mechanisms that give rise to incontinence in general and in the elderly in particular. Aging causes a decrease in neurons of the enteric nervous system and in the release of neurotransmitters, as well as an increase in the proportion of abnormal myenteric ganglia, resulting in altered intestinal motility.
With the passage of time, there is a decrease in neurons of the enteric nervous system and the release of neurotransmitters, as well as anatomical and functional changes: loss of anal cushions, non-functional thickening of both sphincters, decrease in resting pressure and sphincter contraction, decreased distensibility and rectal sensitivity or perineal laxity.12,13
There are several studies that have analyzed the risk factors associated with FI in elderly patients. An epidemiological study published in 2010 differentiated them according to gender. In men, these factors were: age over 85 years (OR 2.5), chronic kidney failure (OR 1.9) and associated urinary incontinence (OR 2.3). However, in women these were: white race, score higher than 5 in the geriatric depression questionnaire (OR 2), associated urinary incontinence (OR 2) and chronic diarrhea (OR 3.5).14
It is also known that, in institutionalized patients, cognitive decline is the most frequent cause of FI,15 since the neurological control of continence largely depends on the central nervous system. Almost 80% of patients who live in nursing homes have some degree of dementia; in this group, it is essential to identify treatable causes of FI, differentiating those cases susceptible to specific therapy from those that will only benefit from supportive treatment.
This deterioration means that sometimes there is no awareness of the need to defecate; at other times communication, mobility or vision are difficult. In patients with mental disorders, it may be sufficient to simply help them improve their mobility, lead them to the bathroom or remind them to go.16
Most published clinical guidelines referring to incontinent older patients often exclude patients with dementia. This was observed in two systematic reviews about various conservative measures in the management of these patients, which concluded that there was not enough evidence to support or rule out their efficacy, so no specific strategy could be recommended.17,18
After the presentation of a cerebrovascular accident, the appearance of FI is not uncommon, even when not present beforehand. Its prevalence decreases with the passage of time: while almost 30% of patients have FI the first 10 days after stroke, this rate stabilizes to around 10% one year later.19 Other gastrointestinal disorders, such as incomplete evacuation or constipation, can affect up to 25% of patients after the acute episode.20 Among all the causes of FI in elderly patients, fecal impaction is, according to different series, the most frequently observed, especially in bedridden patients.21,22 The mechanism that causes incontinence is similar to what occurs in children with encopresis. Fecal impaction leads to irritation of the rectal mucosa, with production of mucus and flow; liquid feces, favored by the use of laxatives in these patients, pass around the compact stools, developing so-called “paradoxical” FI.23,24
Need for Complementary Tests in Older Patients with FIOne of the main disadvantages that we find in these patients is their difficult detection, since information on incontinence is rarely offered spontaneously. Therefore, directed anamnesis and physical examination must be carried out, documenting any previous surgeries, obstetrical history or pelvic radiotherapy. Abdominal palpation, anal inspection and digital rectal examination are also determinants for diagnosis. In these patients, it is useful to perform specific tests to evaluate their mental state, which will help detect whether there is cognitive impairment.25 Once the existence and severity of the pathology are detected, the approach to be followed will be different in a bedridden or dementia patient as opposed to patients who present what in Geriatrics is known as “satisfactory aging”: a patent who is able to independently perform activities of daily living, with no cognitive impairment. In this second case, the studies should be similar to those we would perform in another population group, although they should not delay the start of symptomatic treatment26 (anal ultrasound, manometry and, in very select cases, electrophysiological testing).
Impaction sometimes occurs in the distal colon or proximal rectum, which are areas not accessible to digital examination. If there is clinical suspicion, a simple abdominal radiograph should be requested for diagnosis. Endoscopic studies should be conducted in patients with signs of organ disease, signs for concern (sudden onset, weight loss, rectal bleeding, iron deficiency anemia or family history of colorectal cancer) and in patients who have never undergone screening for colorectal carcinoma.27 In general, we propose complementary testing in patients with suspected organ pathology or impaction and candidates for biofeedback or sphincter repair, provided that we believe that the result could change the therapeutic management.28
Basis for the Conservative Treatment of FI in the ElderlyThe management of older patients with fecal incontinence should be considered in an integral manner, with the involvement of medical professionals as well as family and caregivers. There is a series of support measures, as well as pharmacological measures, which can be applied successively and maintained to improve the quality of life of patients in this age group.
Hygienic and Dermatological CareThe continuous wetness caused by urine and/or fecal leaks causes the skin to be exposed to erosion and frequent overinfections, favoring the appearance of pressure ulcers. Therefore, in these patients it is recommended to use moisturizing creams with a barrier effect, such as those that have zinc oxide, or hydrocolloids.29,30 Fungal overinfections of the perianal skin often occur, which must be detected and treated with topical antifungal agents.
Recommendations in Defecatory HabitSeveral studies have demonstrated that a regular schedule for defecation, as well as going every 3–4h to the bathroom to also promote the urinary habit, significantly decreases episodes of incontinence.31 These measures are especially useful in patients with dementia and those requiring assistance for activities of daily living.
Dietary ChangesSometimes, nutritional management of these patients may be enough to improve involuntary fecal leaks. In general, fat intake should be reduced and precautions taken with products that have sorbitol and lactose or derivatives. If there is no associated diarrhea, it is recommended to gradually add vegetable fiber supplements accompanied by at least 1l of water per day. The mechanism by which fiber decreases FI episodes is related to its solubility, degradation and fermentation by colon bacteria.32 Fermentable or intermediate fermentable soluble fiber has no laxative effect and can be recommended in these patients (psyllium, guar gum or pectin, at a dose of about 15g per 1000kcal ingested). A clinical trial that compared three different types of dietary fiber obtained a lower rate of FI episodes in patients treated with psyllium.33
Mechanical DevicesAnal plugs are devices that have been adapted from devices used in stomata. They usually consist of a polyurethane sponge wrapped in a plastic that maintains its compact shape to facilitate insertion. This plastic dissolves upon contact with the rectal mucosa and the plug expands in a few seconds, adapting to the shape of the lower rectum. Anal plugs often cause discomfort and are difficult to tolerate. They can be useful in passive FI with small fecal leaks, so they should be considered in the treatment algorithm of these patients. A related Cochrane review concluded that plugs are difficult to tolerate but, in those patients who are able to use it, the prevention of fecal leaks is effective. Likewise, it indicates that the type of plug may influence the result, and polyurethane is favored over polyvinyl.34
Enemas and Irrigation SystemsTransanal irrigation is another support tool in the management of these patients. It can be carried out simply by filling the irrigation “bulb” with warm water; this procedure can be repeated until the rectal ampulla is emptied. There are also other commercial irrigation systems that are somewhat more complex, in which the patient or the caregiver can control the amount of liquid that is introduced and the length of stay in the colon. After evacuating the balloon and removing the catheter, the fecal content is evacuated. Patients with FI often benefit from the use of enemas when defecation does not occur within 2–3 days and the rectal ampulla is full. In cases of sphincter dysfunction, this measure may be ineffective due to the inability to retain the introduced content. Likewise, caution is recommended with enemas that contain sodium phosphate, since they can produce local ulceration in the rectum.
Pharmacological TreatmentUsually, these physical and dietary measures are not sufficient to improve FI, so we must frequently associate medical treatment according to the consistency of the feces. When there is diarrhea or semi-liquid feces, loperamide is indicated as the first line of treatment, starting with effective minimum doses and not exceeding 8g. Codeine can also be used at a dose of 30mg every 8h and diphenoxylate at a dose of 15mg distributed throughout the day. A cross-over, double-blind study comparing these three treatments for 4 weeks showed less of a benefit in patients treated with diphenoxylate. This, together with the fact that it is a drug that crosses the blood–brain barrier and can have anticholinergic side effects, makes it the least recommended.35 Amitriptyline at low doses (20mg/day) has also been used as a complementary treatment in these patients because of its effect both in reduction the amplitude and frequency of rectal motor complexes and in the increase in sphincter pressure.36
In cases of constipation, we must bear in mind that prescribing fiber supplements may not be appropriate as they must be accompanied by ingestion of abundant fluids, which is sometimes not achieved in this type of patients. Therefore, it is advisable to start treatment with organic osmotic laxatives (polyethylene glycol with electrolytes, lactitol or lactulose); if they are not effective, continue with inorganic osmotic laxatives (magnesium salts), lubricants (glycerin suppositories) and, as a last step, stimulating laxatives (bisacodyl).37 This last group should be administered with caution, since their long-term use can cause atonic colon. Likewise, emollient laxatives like paraffin are not routinely recommended because of the risk of pneumonia secondary to microaspiration and the altered absorption of fat-soluble vitamins. When there is suspicion or confirmation of fecal impaction, the treatment should be aimed at disimpaction, colon cleansing and, subsequently, measures to prevent recurrence.38
After fragmentation of the fecaloma, a warm water enema can be administered to help empty the rectum. Initially, small volumes can be used that will be progressively increased. The most widely recommended osmotic laxative for the treatment of fecal impaction is macrogol with electrolytes (8 sachets per day diluted in 1l of water to be taken within 6h; this dosage can be repeated up to 3 days).
The Role of Biofeedback and Pelvic Floor Rehabilitation in the Treatment of Fecal Incontinence in Elderly PatientsRehabilitation through biofeedback aims to reeducate the coordination between voluntary contraction of the sphincter and emptying of the rectum, increase muscle contraction, and improve rectal sensitivity and reflexes. Whitehead et al. specifically analyzed a group of patients with a mean age of 73 years (65–92), obtaining a 77% improvement in the force of contraction and 50% in the reduction of the sensitivity threshold.39 There are minimum requirements to achieve positive results in these patients: sufficient cognitive function, willingness to cooperate and a certain functionality of the external anal sphincter, maintaining some capacity for voluntary contraction. Therefore, we should consider biofeedback in the treatment algorithm of patients who are candidates for this therapy.
Effectiveness of Sphincteroplasty in Patients Over 65In the published literature, there are few articles that specifically study the result of sphincter repair according to age, making it difficult to draw conclusions in older patients. There are studies that determine that the older the age, the worse the prognosis. However, others have not found a correlation between age and postoperative result.
Simmang et al. analyzed 14 patients between 55 and 81 years of age undergoing sphincteroplasty; thirteen of the fourteen improved clinically, and 50% achieved perfect continence. These results were comparable to another subgroup of younger patients.40 Another study of almost 200 patients undergoing sphincteroplasty analyzed the results comparing two groups, with a cutoff age of 60 years; there were no differences between the two for severity scale, quality of life or overall satisfaction.41 In contrast, a publication by the Oxford group did find significant differences between the mean age of patients who improved compared to those who did not (38 vs 56 years), although belonging to one or another group was not defined by age.42 Therefore, older patients should be informed about the limited long-term improvement and may consider other alternatives that offer higher rates of symptomatic response.
Improved Continence After Rectal Prolapse Repair in the SeniorsExternal rectal prolapse is a frequent cause of FI in the general population; its association with perineal laxity frequently observed in the elderly makes it necessary to consider its repair in patients who are candidates for surgery. So far, no surgical technique has been shown to be superior for the treatment of rectal prolapse in elderly patients.43 Perineal procedures (interventions by Altemeier and Delorme) have shown in a recently published (in press) systematic review an improvement in continence of 61.4% and 69%, respectively, with morbidity figures of around 10%.44 On the other hand, the abdominal approach should also not be ruled out only based on the age of these patients. Laparoscopic ventral rectopexy has been shown to be a safe procedure in people over 70 years of age, with no differences in morbidity and mortality compared to younger patients and a continence improvement rate of 45%.45
Result of Nerve Stimulation in Older PatientsThe increase in life expectancy and quality of life of the population in developed countries makes it necessary to consider the use of specific therapies in increasing age groups. Sacral nerve stimulation is the most effective treatment for FI that is refractory to conservative measures; however, there is some reluctance to indicate it in older patients due to possible complications, the ability to understand their management or the lower efficacy. Although there is less experience in patients older than 65–70 years, there are some specific publications in this regard. Thirty patients with a mean age of 69.3 years were followed prospectively for a mean of 44 months by George et al.,46 obtaining an efficacy similar to that shown in younger patients, both in episodes of incontinence per week and in the ability to delay defecation. A study published by White et al. also showed similar efficacy, although with a higher rate of implant removal in patients over 70 years of age.47
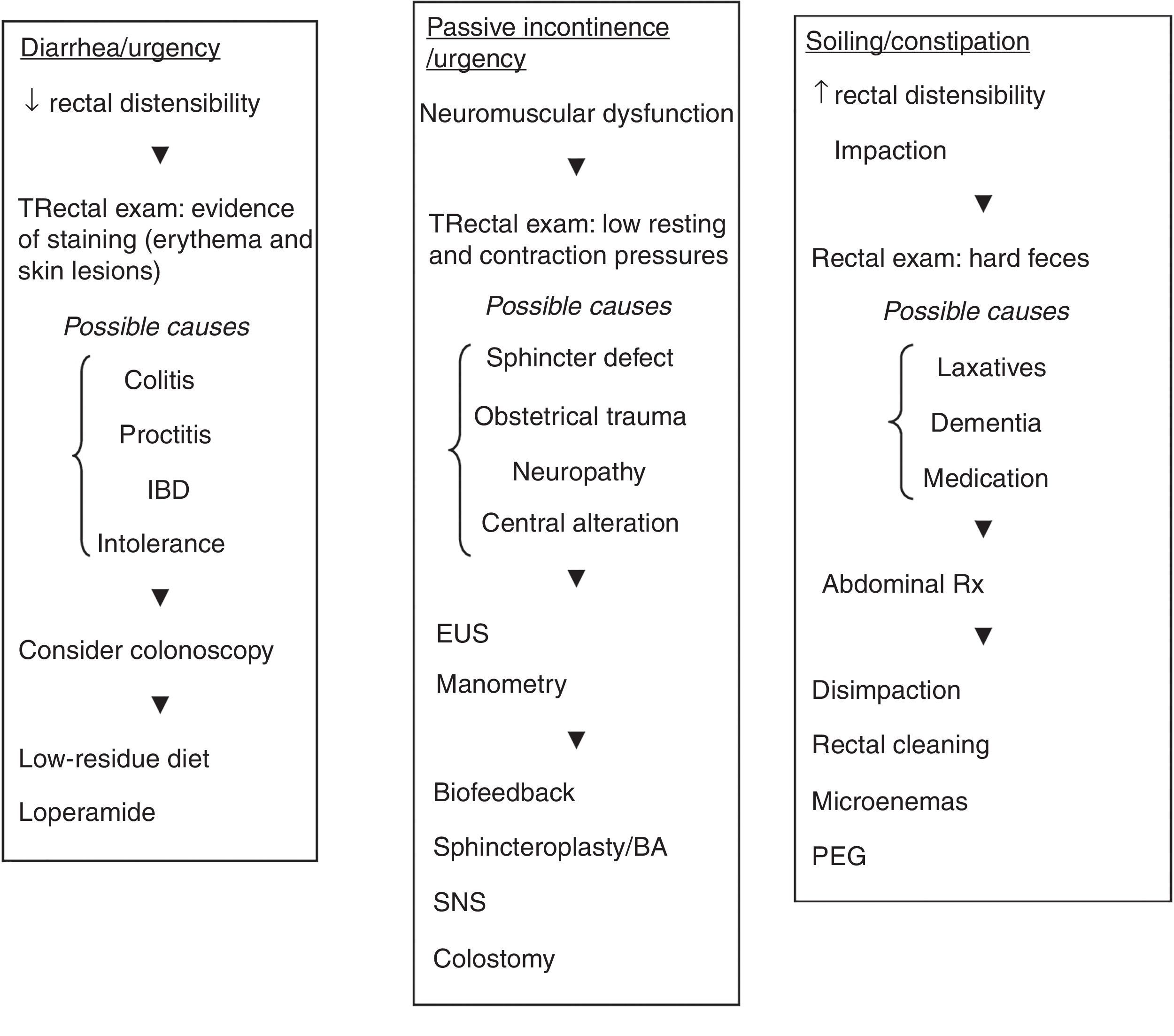
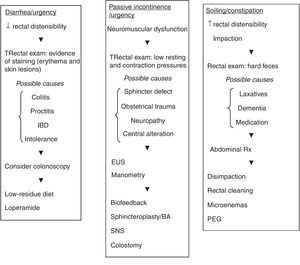
Management AlgorithmGiven the information obtained in the review of the literature, we have created a management proposal for these patients, represented in a diagnostic-therapeutic algorithm for different clinical scenarios: increase or decrease in rectal capacity and neuromuscular dysfunction (Fig. 1).
Diagnostic-therapeutic algorithm in different clinical scenarios.
BA: volume increasing agents; EUS: endoanal ultrasound; PEG: polyethylene glycol; SNS: sacral nerve stimulation.
The prevalence of fecal incontinence significantly increases with age, regardless of comorbidity. Complementary studies should be conducted in patients with suspected organ pathology or impaction and whenever they are being considered candidates for specific treatment. Modifications in habits and diet, as well as control of the consistency and frequency of stools, are often effective in the management of these patients. Other more invasive treatments should not be ruled out and should be assessed individually, as they can provide optimal results in older patients. Unfortunately, the absence of randomized studies, clinical guidelines and meta-analyses limits the conclusions obtained for each question posed. Additional specific studies are necessary to identify the most beneficial and cost-effective management regimen in these patients.
Authorship/collaboratorsAna María García Cabrera and Fernando de la Portilla have participated in the study design, analysis and interpretation of the results as well as the critical review and approval of the final version.
Rosa María Jiménez, María Luisa Reyes and Carmen Palacios have contributed to the data collection and study design.
José Manuel Díaz and María Ramos have participated in the study design and data collection.
Jorge Manuel Vázquez and Carmen Palacios have contributed to the study design as well as the analysis and interpretation of the results.
Javier Padillo has participated in the analysis and interpretation of the results as well as the critical review and approval of the final version.
The authors declare having no conflict of interests.
Please cite this article as: García Cabrera AM, Jiménez Rodríguez RM, Reyes Díaz ML, Vázquez Monchul JM, Fernández MR, Díaz Pavón JM, et al. Incontinencia fecal en el paciente anciano. Revisión de conjunto. Cir Esp. 2018;96:131–137.