Renal cell tumors have a great tendency toward growing and invading the renal vein1,2 and, as they progress, they can invade the vena cava, which is affected in 4%–15%2–4 of cases at diagnosis. Even though aggressive surgery is involved, complete resection of the tumor and thrombus can lead to a cure of the disease and better short and long-term prognoses.5–8
We present the case of a 59-year-old male who was admitted to the urology ward due to symptoms of hematuria. His personal medical history included hypothyroidism and bilateral pulmonary thromboembolism one year before.
On admission, abdominopelvic ultrasound showed a mass in the lower side of the right kidney, measuring 9cm and suggestive of hypernephroma. The study was completed with CT angiography, which detected renal hypernephroma with a tumor thrombus that extended along the renal vein up to the infrahepatic vena cava, as well as hilar, right paraesophageal and retroperitoneal lymphadenopathies.
The case was assessed by the Oncology Department; treatment with sunitinib was initiated (50ml every 24h), which was suspended during the second cycle due to toxicity.
Another CT angiogram was ordered, which showed a 1-cm reduction of the tumor, although the venous tumor thrombosis and local lymphadenopathies remained. The extension study of the tumor thrombosis was completed with magnetic resonance angiography (Fig. 1).
Given the impossibility to continue with chemotherapy, the Urology and Vascular Surgery Departments decided to carry out a joint surgical intervention.
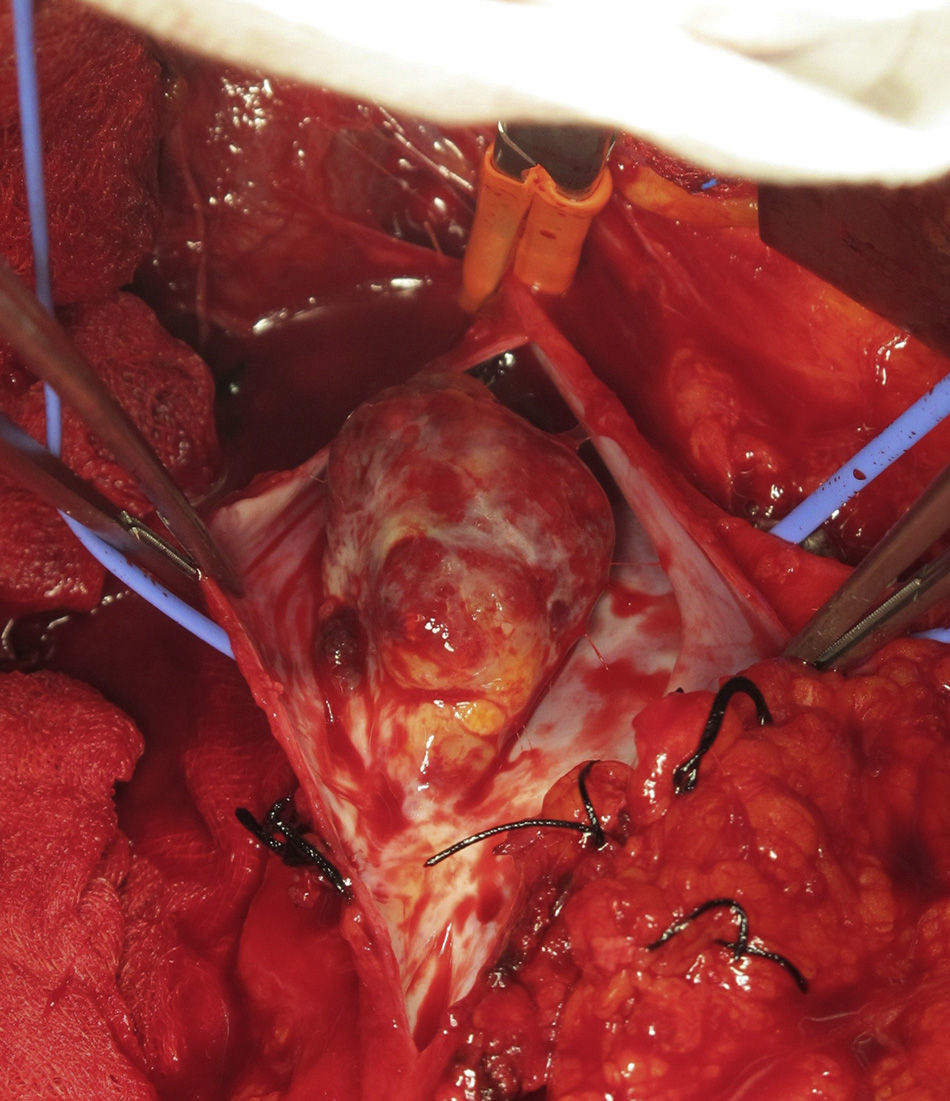
Using general anesthesia and midline laparotomy, a right nephrectomy was performed with proximal and distal control of the inferior vena cava (IVC) as well as the right renal vein. The IVC was opened and the tumor thrombus was resected en bloc; the venous wall was closed with a pericardial patch (Fig. 2).
The pathology study reported the surgical specimen to be club cell adenocarcinoma with a Fuhrman grade of I–II/IV with infiltration of the perirenal fat and the wall of the renal vein.
The post-surgical evolution was satisfactory and without complications. Follow-up MRI angiography was done 2 weeks later, which detected neither tumor recurrence nor thrombus in the vena cava. The patient was discharged with tinzaparin (20000IU).
Six months later, the patient was asymptomatic, with no signs of recurrence.
Renal tumors represent 2%–3% of malignant tumors in adults,9,10 although in recent years their incidence has been increasing due to incidental diagnoses. Invasion of the vena cava is more frequent in males (4:1)2 and is usually due to right renal tumors. More than 80% are adenocarcinomas and, amongst these, the club-cell variety is most frequent.
Apart from the locoregional symptoms of the tumor,1 the classic triad of hematuria, abdominal mass and lumbar pain is only found in one-third of cases at diagnosis and is usually accompanied by advanced disease, which implicates a poorer prognosis. 10%–40% of patients may present paraneoplastic syndromes. Only 35% of the patients present symptoms of venous obstruction due to tumor invasion.
In addition to standard diagnostic tests (lab work, chest X-ray, renal ultrasound), CT and MRI2,4,9,10 help to make a more precise diagnosis, with the advantage of being non-invasive tests. CT enables us to study the presence of metastasis and lymph node involvement, while MRI is considered the most sensitive and specific test for assessing the presence and extension of the thrombus in the vena cava.
As for surgical treatment, the approach and surgical technique5,8,9 depend on the level of the cephalic end of the thrombus in the vena cava. For the surgery to be successful, careful management of the vena cava is very important in order to minimize bleeding and avoid embolisms. The segment of the affected vein should be resected with safety margins, while allowing for correct drainage of the contralateral kidney. In order to substitute the resected segment, bovine pericardium, Dacron or Gore-Tex patches can be used. In recent years, neoadjuvant multikinase inhibitors (sunitinib) have been used to reduce the tumor thrombus.
Although the presence of tumor thrombus in the vena cava was considered a factor for poor prognosis,1,9 new surgical techniques have led to significant changes. Most series report that the presence of distant metastasis and lymph node involvement are the two factors that most influence survival. If there is no metastasis, surgery has a curative aim. Thus, although it is more aggressive and entails a higher morbidity and mortality, successful resection of the tumor and of the affected segment of the vena cava achieves a 5-year survival rate of 57%–68%.
Based on a review of the literature and on our experience, surgery in renal cell tumors with invasion of the vena cava is considered the technique of choice,8–10 since, in the absence of metastasis, it is able to cure the disease while improving short- and long-term prognoses.
FundingThe authors declare having received no funding.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: González Martínez P, Salazar Agorria A, Bravo Ruiz E, Suarez Tornin MJ, Vega Manrique R. Hipernefroma con trombosis tumoral de vena cava inferior. Cir Esp. 2014;92:632–633.
The authors indicate that the information from this article has not been presented at any congresses.