Some groups have initiated outpatient bariatric surgery programs in selected patients, publishing good results after sleeve gastrectomy. Recent studies show that outpatient surgery is also feasible and safe in Roux-en-Y gastric bypass.
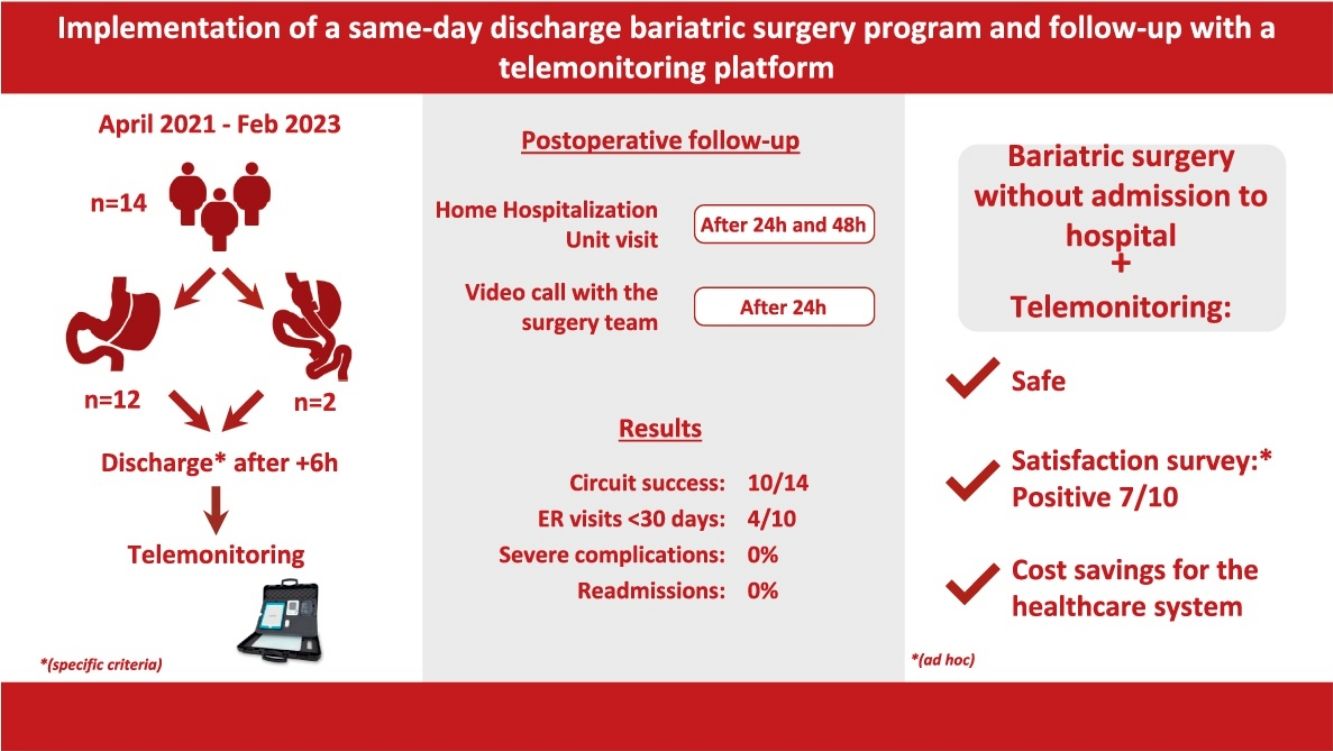
The aim of this paper is to describe and analyze the results of our initial experience after the implementation of a same-day discharge bariatric surgery program using a telemonitoring system.
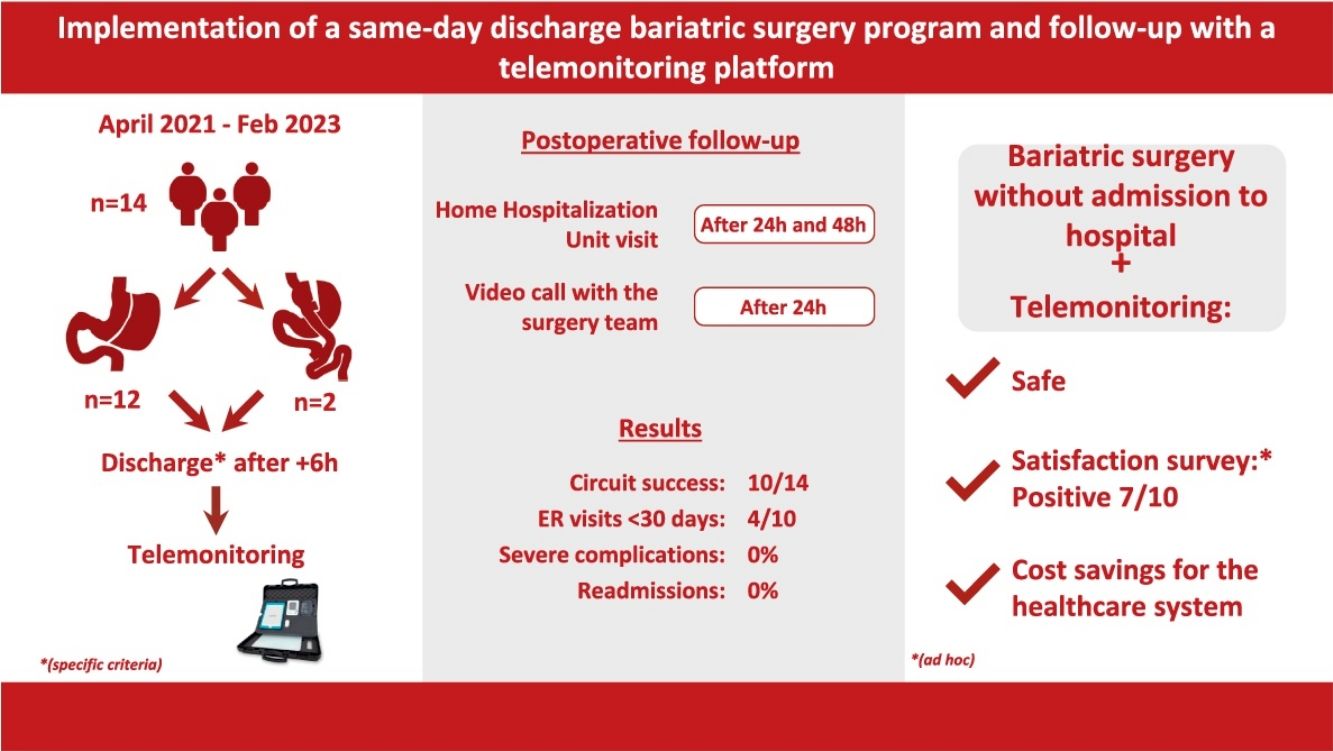
MethodsWe have completed a prospective, observational study with 14 consecutive, selected patients undergoing primary bariatric surgery (sleeve gastrectomy or Roux-en-Y gastric bypass) at a single center from April 2021 to February 2023, with home follow-up using the REVITA® telemonitoring platform (HI Iberia, S.A.) and the Home Hospitalization Unit.
ResultsFrom April 2021 to February 2023, 14 patients were selected for this program, which meant 7.3% of the total of 191 patients who underwent bariatric surgery during this period. Ten out of the 14 patients selected completed the circuit (71.4%), 4 of whom consulted the emergency department within the first 24 h (40%). There were no serious complications, readmissions or re-operations typical of bariatric surgery.
The estimated savings per patient who completed the circuit was 762.
ConclusionBariatric surgery without hospital admission is feasible and safe in selected patients using a telemonitoring platform and with the support of a home hospitalization unit.
Existe experiencia previa en programas de cirugía bariátrica ambulatoria en pacientes seleccionados, que reportan buenos resultados tras gastrectomía vertical. Estudios recientes demuestran que la cirugía ambulatoria también es factible y segura en el bypass gástrico en Y de Roux.
El objetivo del presente trabajo es describir y analizar los resultados de nuestra experiencia inicial tras la implementación de un programa de cirugía bariátrica sin ingreso hospitalario, con la utilización del sistema de telemonitorización.
MétodosEstudio observacional prospectivo con 14 pacientes consecutivos seleccionados, intervenidos de cirugía bariátrica primaria (gastrectomía vertical o bypass gástrico en Y de Roux) en un único centro, desde abril de 2021 hasta febrero 2023, con seguimiento en domicilio mediante la plataforma de telemonitorización REVITA® (HI Iberia, S.A.) y la Unidad de Hospitalización a Domicilio.
ResultadosDesde abril de 2021 a febrero 2023 fueron seleccionados para este programa 14 pacientes, lo cual significa el 7,3% del total de 191 pacientes intervenidos de cirugía bariátrica durante este periodo. Llegaron a completar el circuito 10 de los 14 pacientes seleccionados (71,4%). 4 de los 10 pacientes que completaron el circuito consultaron a urgencias en las primeras 24 horas (40%). No hubo complicaciones graves, reingresos, ni reintervenciones propias de la cirugía bariátrica.
Se ha estimado un ahorro de 762 por cada paciente que completa el circuito.
ConclusionesLa cirugía bariátrica sin ingreso hospitalario es factible y segura en pacientes seleccionados usando una plataforma de telemonitorización y con el apoyo de una unidad de hospitalización a domicilio.
Advances in surgical techniques and the implementation of multimodal rehabilitation programs have improved the results of patients undergoing bariatric procedures, while also reducing their hospital stays.1 In addition, ambulatory surgery programs have proven to be cost efficient and safe in various pathologies and even in high-risk patients.2
These advances have prompted several groups to initiate outpatient bariatric surgery programs in selected patients. Good results have been published in sleeve gastrectomy, with no increase in the number of complications, readmissions, or emergency department visits.3–5 Recent studies show that ambulatory surgery is also feasible and safe in Roux-en-Y gastric bypass.6,7
When it comes to the generalized use of this type of procedure in the day surgery setting, one of the main problems is the need to be able to offer patients a safe environment during the immediate postoperative period. Thus, devices that facilitate the acquisition, recording and interpretation of data (especially vital signs) that also promote effective communication with the patient are essential to provide optimal care in a remote context. Advances made in these devices as well as the appropriate computer support have made it possible for telemonitoring to become a reality in today’s patient care.
Coinciding with the SARS-CoV-2 pandemic, which affected the availability of healthcare resources, the viability of implementing a bariatric surgery program without hospital admission for a selected group of patients was considered by the Endocrine, Bariatric and Metabolic Surgery unit at our hospital. Such a program was made possible by the experience of the team, the infrastructure of our hospital, and the use of a telemonitoring platform.
The objective of this paper is to describe the results of our initial experience, while also analyzing factors related to patient safety and satisfaction, the use of the telemonitoring system, as well as difficulties in the implementation of the program.
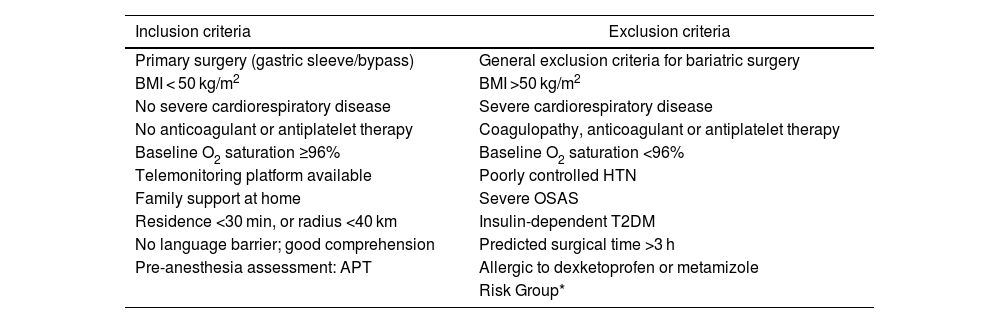
MethodsWe have conducted a prospective, observational study in patients undergoing primary bariatric surgery (sleeve gastrectomy or Roux-en-Y gastric bypass) at a single tertiary referral center, from April 2021 to February 2023, using the inclusion and exclusion criteria specified in Table 1.
Inclusion and exclusion criteria (Risk Group*: 4 or more): male, age >45, BMI > 45, previous DVT or PE, HTN (Nijland et al.6).
| Inclusion criteria | Exclusion criteria |
|---|---|
| Primary surgery (gastric sleeve/bypass) | General exclusion criteria for bariatric surgery |
| BMI < 50 kg/m2 | BMI >50 kg/m2 |
| No severe cardiorespiratory disease | Severe cardiorespiratory disease |
| No anticoagulant or antiplatelet therapy | Coagulopathy, anticoagulant or antiplatelet therapy |
| Baseline O2 saturation ≥96% | Baseline O2 saturation <96% |
| Telemonitoring platform available | Poorly controlled HTN |
| Family support at home | Severe OSAS |
| Residence <30 min, or radius <40 km | Insulin-dependent T2DM |
| No language barrier; good comprehension | Predicted surgical time >3 h |
| Pre-anesthesia assessment: APT | Allergic to dexketoprofen or metamizole |
| Risk Group* |
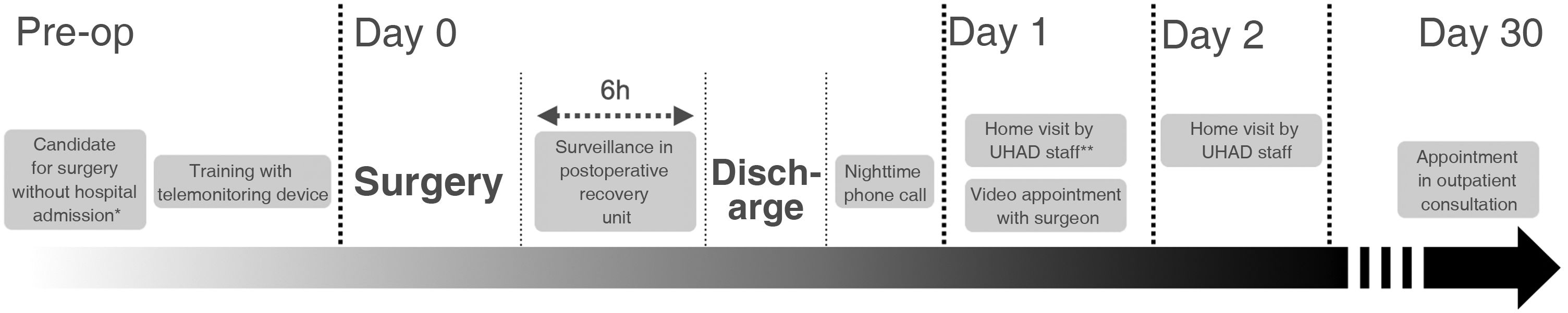
We discussed the possibility of surgery without hospital admission with the selected patients and explained the circuit described in Fig. 1. When they accepted participation in the program, they signed the specific informed consent form.
Before the visit with the anesthesiologist and after being assessed by our Home Hospitalization Unit (Unidad de Hospitalización a Domicilio, or UHAD), the patients were trained in the use of the REVITA® telemonitoring platform (HI Iberia), which provides telemonitoring of vital signs (blood pressure, heart rate, oxygen saturation, temperature and weight), as well as video calls. The device includes a blood pressure monitor, pulse oximeter, thermometer and scale. These elements are connected by Bluetooth to a portable tablet, from where the recordings are sent to the hospital electronic registry (SAP, IBM Cloud) (Fig. 2).
The patients underwent surgery with either the Da VinciⓇ Xi/X robotic platform (Intuitive Surgical Inc, USA) or laparoscopy, scheduled first thing in the morning in order to have a minimum postoperative surveillance period of 6 h before being discharged to home.
The same multimodal anesthesia and rehabilitation protocol was used as in our inpatient bariatric surgery program. The indication and surgical technique (sleeve gastrectomy or gastric bypass) were no different from our team’s usual program.
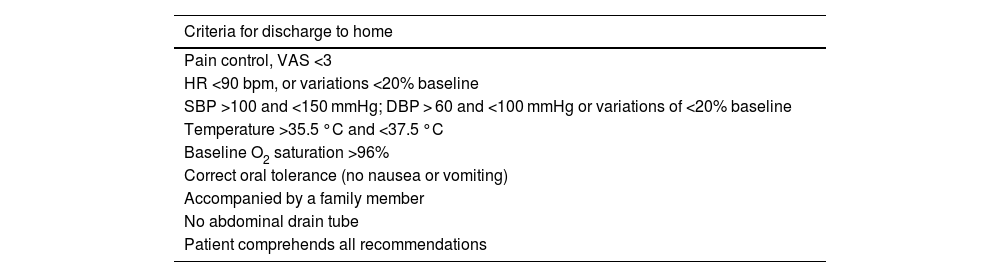
After surgery, patients remained for 2 h in the postoperative recovery room under the supervision of the Anesthesiology Service. Subsequently, patients were transferred to the surveillance room of the Major Ambulatory Surgery Unit to complete a period of 4−6 h of monitoring by nursing staff. Lastly, a member of the surgical team decided whether to discharge each patient to home, based on strict compliance with the criteria in Table 2. Otherwise, the patient was admitted to the conventional surgical ward.
Criteria for discharge.
| Criteria for discharge to home |
|---|
| Pain control, VAS <3 |
| HR <90 bpm, or variations <20% baseline |
| SBP >100 and <150 mmHg; DBP > 60 and <100 mmHg or variations of <20% baseline |
| Temperature >35.5 °C and <37.5 °C |
| Baseline O2 saturation >96% |
| Correct oral tolerance (no nausea or vomiting) |
| Accompanied by a family member |
| No abdominal drain tube |
| Patient comprehends all recommendations |
Analgesia consisted of an elastomeric pump for continuous intravenous infusion of 200 mg/100 mL dexketoprofen and 8 g/100 mL metamizole during the first 48 h. Thromboprophylaxis with weight-adjusted subcutaneous low-molecular-weight heparin and 4 mg intravenous ondansetron were indicated as antiemetic treatment during in-hospital surveillance.
Once at home, that same afternoon and every 8 h thereafter, patients measured their vital signs with the telemonitoring platform, which transmitted the data to the medical team electronically. Both 24 h and 48 h after surgery, patients were evaluated at home by a member of the UHAD in order to monitor symptoms and adjust treatment, if necessary. In addition, a surgeon from the team held a video consultation 24 h after surgery, consisting of a video call to confirm the absence of surgical complications and to answer any possible patient questions.
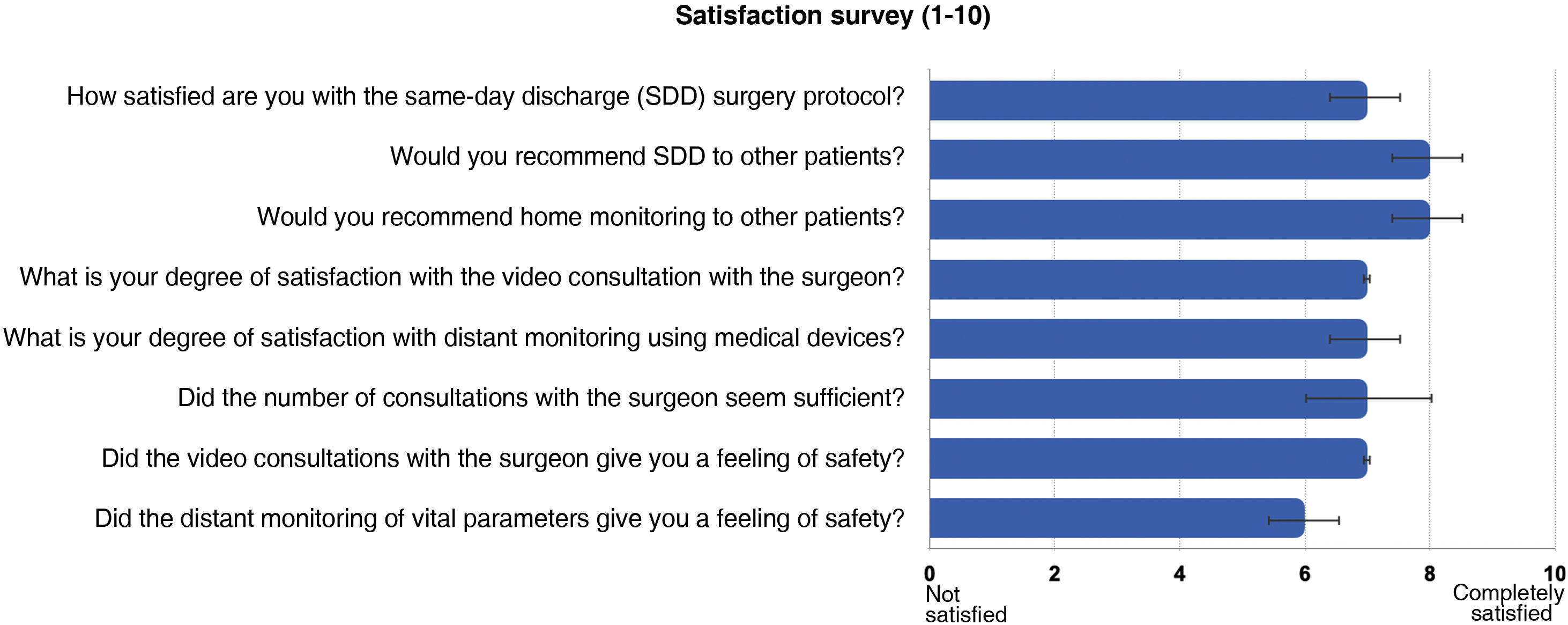
Our study has analyzed the total number of patients undergoing bariatric surgery, the number of patients selected for the surgery program without hospital admission, the number of patients who ultimately were able to complete the circuit, intra and postoperative complications, consultations in the Emergency Department, and readmissions within 30 days. Likewise, we have estimated the direct economic costs derived from the hospital stay per patient. Given that the average stay in our unit in a conventional hospitalization regimen is 2.5 days (SD 0.93), our analysis considered the cost of surgery without admission and the hypothetical savings per patient and per day that the program would provide. Lastly, patient satisfaction was analyzed amongst those who completed the circuit using an ad hoc survey during the first in-person consultation. This survey was equivalent to those used in similar programs, such as the one employed by Nijland et al.6
The data have been collected prospectively with a total number of 14 consecutive patients, and a descriptive analysis of the data was performed. The qualitative variables are presented by number of cases and frequency distribution of the percentages of each category. Quantitative variables are expressed using indicators of central tendency (median and interquartile range).
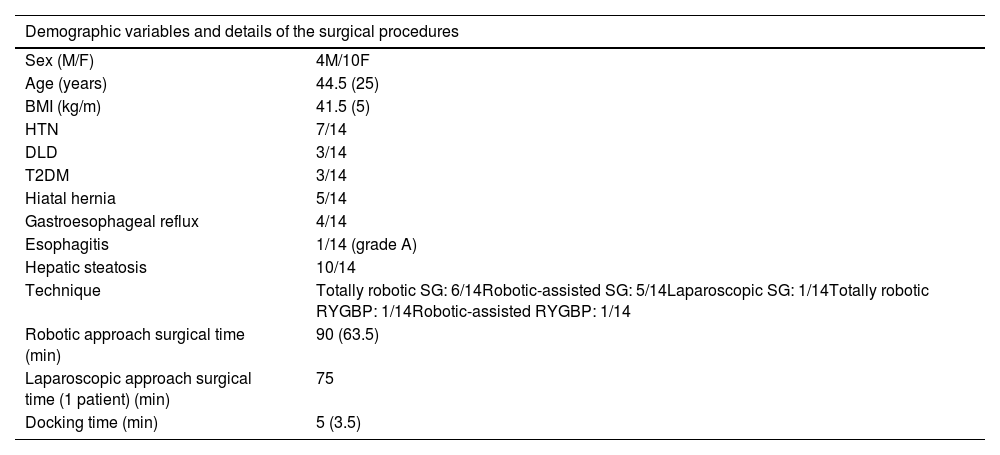
ResultsFrom April 2021 to February 2023, 14 patients were selected, representing 7.3% of the total number of patients operated on for bariatric surgery during this period. Ten out of the 14 selected patients (71.4%) completed the circuit. The characteristics of these patients and the surgeries performed are detailed in Table 3. In the end, 4 out of the 14 selected patients were admitted to the conventional hospital ward because the established discharge criteria were not met (28.5%): one patient presented persistent baseline oxygen saturation levels below 96%; 2 patients presented poor pain control, nausea and inability to initiate an oral diet; and the last patient was not able to complete the required hours in the postoperative recovery room after undergoing surgery in the afternoon. None of the 14 patients included in the circuit presented intraoperative complications. Four out of the 10 patients who correctly completed the circuit visited the emergency room in the first 30 days: one due to poor pain control caused by poor perfusion of the elastomeric pump; 2 due to surgical wound dehiscence; and one due to constipation with fecaloma and prolapsed hemorrhoids, which required manual reduction in the operating room with locoregional anesthesia and sedation. There were no serious complications, readmissions, or reoperations typical of bariatric surgery.
Demographic variables: M/F (Male/Female); and details about the surgical procedure (SG: sleeve gastrectomy; RYGBP: Roux-en-Y gastric bypass).
| Demographic variables and details of the surgical procedures | |
|---|---|
| Sex (M/F) | 4M/10F |
| Age (years) | 44.5 (25) |
| BMI (kg/m) | 41.5 (5) |
| HTN | 7/14 |
| DLD | 3/14 |
| T2DM | 3/14 |
| Hiatal hernia | 5/14 |
| Gastroesophageal reflux | 4/14 |
| Esophagitis | 1/14 (grade A) |
| Hepatic steatosis | 10/14 |
| Technique | Totally robotic SG: 6/14Robotic-assisted SG: 5/14Laparoscopic SG: 1/14Totally robotic RYGBP: 1/14Robotic-assisted RYGBP: 1/14 |
| Robotic approach surgical time (min) | 90 (63.5) |
| Laparoscopic approach surgical time (1 patient) (min) | 75 |
| Docking time (min) | 5 (3.5) |
The quantitative variables are expressed in median and interquartile range in parentheses.
According to the estimated cost analysis of our medical center, the cost of a conventional hospital admission for bariatric surgery is 409/day, versus the cost of “home hospitalization” of 109/day, without including the expenses of the operation itself.
If we multiply this by the average stay (2.5 days), the estimated cost per patient in a conventional hospitalization regimen would be 1022.50, compared to 272.50 if the patient were monitored at home. Therefore, the savings for each patient who completes the circuit is estimated at 750. However, the cost of the telemonitoring device must also be added, which is 90/month per device as an initial investment.
As shown in Fig. 3, the patients evaluated the program with a positive score in terms of overall satisfaction according to the results of the satisfaction surveys.
DiscussionThe growing prevalence of obesity and the increase in bariatric procedures require the constant optimization of resources while guaranteeing appropriate follow-up. The initial results of our program allow us to believe that it is feasible to implement a bariatric surgery program with same-day discharge (SDD) in selected cases, with the help of constant telemonitoring platforms for patient safety and with the help of the Home Hospitalization Unit.
In our hospital, we have treated 7.3% of all patients undergoing bariatric surgery over the last 22 months. A significant number of patients could have become candidates but ultimately did not give their consent, mainly out of fear (of not being able to be treated in the event of a complication) or uncertainty about the efficacy of the devices. Another possible influencing factor is the important cultural differences observed in an area with a population as heterogeneous as ours, although this parameter was not analyzed. We believe that the results of this initial experience, together with patient satisfaction, will allow us to increase the number of patients who will benefit from this follow-up modality.
Our circuit has had a success rate of 71.4% (10 out of the 14 selected patients completed the circuit successfully). This datum gives us an idea of safety and good compliance with the strict discharge criteria, even though there was a significant rate of emergency room visits in less than 30 days (40%; 4 out of the 10 patients who completed the circuit), although there were no serious complications, readmissions, or reoperations. Interestingly enough, these patients continued to have a high level of satisfaction.
In the context of the SARS-COV-2 pandemic, or in other situations requiring the optimization of intra-hospital resources (number of hospital beds, less contact with medical staff), the evolution of new telemonitoring devices and the implementation of surgery programs without hospitalization or 100% ambulatory surgery may allow for surgical activity to be maintained and may even reduce the costs of metabolic and bariatric surgery.
In recent years, we have witnessed improved results for this type of surgery, together with a significant reduction in hospital stay, thanks to advances made in the surgical technique, the application of minimally invasive procedures and the implementation of perioperative multimodal rehabilitation.8–10 Moreover, several study centers have published their experience and good results with outpatient bariatric surgery programs.3–7,11 The study by Nijland et al.6 is especially interesting, in which they demonstrate that gastric bypass without hospital admission using telemonitoring support is feasible and safe in selected patients, reporting strong compliance with the circuit and an 88% success rate (44/50 patients included), an 11% rate of emergency visits in the first 30 days, a 4% readmission rate, and no reoperations or mortality in their series.
In our case, the accumulated experience in minimally invasive bariatric surgery, and especially the use of the robotic platform, has led to a clear improvement in the results and a reduction in hospital stay in accordance with the mentioned literature. This has made it possible to develop this program with no observed increase in complications to date. The fact that 71.4% of the selected patients did not need hospital admission allows us to determine the feasibility of the program and to be optimistic regarding its clinical and economic impact as more patients are incorporated.
There is not enough evidence in the literature to recommend which patients are candidates for outpatient bariatric surgery, although those with a BMI greater than 50 kg/m2 have a higher risk of perioperative complications and, therefore, would apparently not be candidates.12 For this reason, the selection criteria that we have established are based on the work of previous groups, adapted to the setting and conditions of our patients and healthcare system.
This study has several limitations. First of all, as it is a pilot study experience with a small number of patients, we can only affirm that this bariatric surgery program without hospital admission is viable; however, a much larger sample is needed to confirm that its safety is comparable to standard practice. Secondly, the use of the telemonitoring platform entails a certain amount of complexity, and selection biases may occur due to the “digital divide” (inequality in access, use, or impact of new technologies between social groups). Finally, the fact that most of our patients were operated on using a robotic platform could be considered a factor that prevents this study from being reproduced at medical centers where it is not available. Nevertheless, our impression is that this patient care strategy can be generalized to other surgical approaches. The studies published to date on ambulatory bariatric surgery correspond to laparoscopic procedures, so we believe that the availability of the robotic platform is not a condition for initiating a similar program.
Previous retrospective studies about ambulatory surgery with laparoscopic Roux-en-Y gastric bypass have reported unfavorable results in terms of complications. However, more recent studies, such as the Leepalao et al. paper11 from 2020, have concluded that ambulatory bariatric surgery in selected patients is safe. In none of these studies was a telemonitoring platform used.
Therefore, we can conclude that bariatric surgery without hospital admission is feasible and safe in selected patients using a telemonitoring platform with the support of a home hospitalization unit. In addition, it provides benefits for patients, with good scores on satisfaction questionnaires (Patient-Reported Experience Measure [PREM] and Patient-Reported Outcome Measure [PREM]), while also optimizing healthcare resources and surgery circuits, which will ultimately reduce the cost of the process.
Conflict of interestNone.
To my colleagues at the Morbid Obesity Unit of the Germans Trias i Pujol University Hospital.
To the medical, nursing and administrative staff of the Home Hospitalisation Unit of the Hospital Universitari Germans Trias i Pujol.
To the nursing and auxiliary nursing staff of the Major Outpatient Surgery Unit of the Hospital Universitari Germans Trias i Pujol. Germans Trias i Pujol University Hospital.
To the medical and nursing staff of the Anaesthesiology and Resuscitation Service of the Hospital Universitari Germans Trias i Pujol.
To the nursing, auxiliary nursing and administrative staff of the sixth floor of the Hospital administrative staff of the sixth floor of the Hospital Germans Trias i Pujol University Hospital.