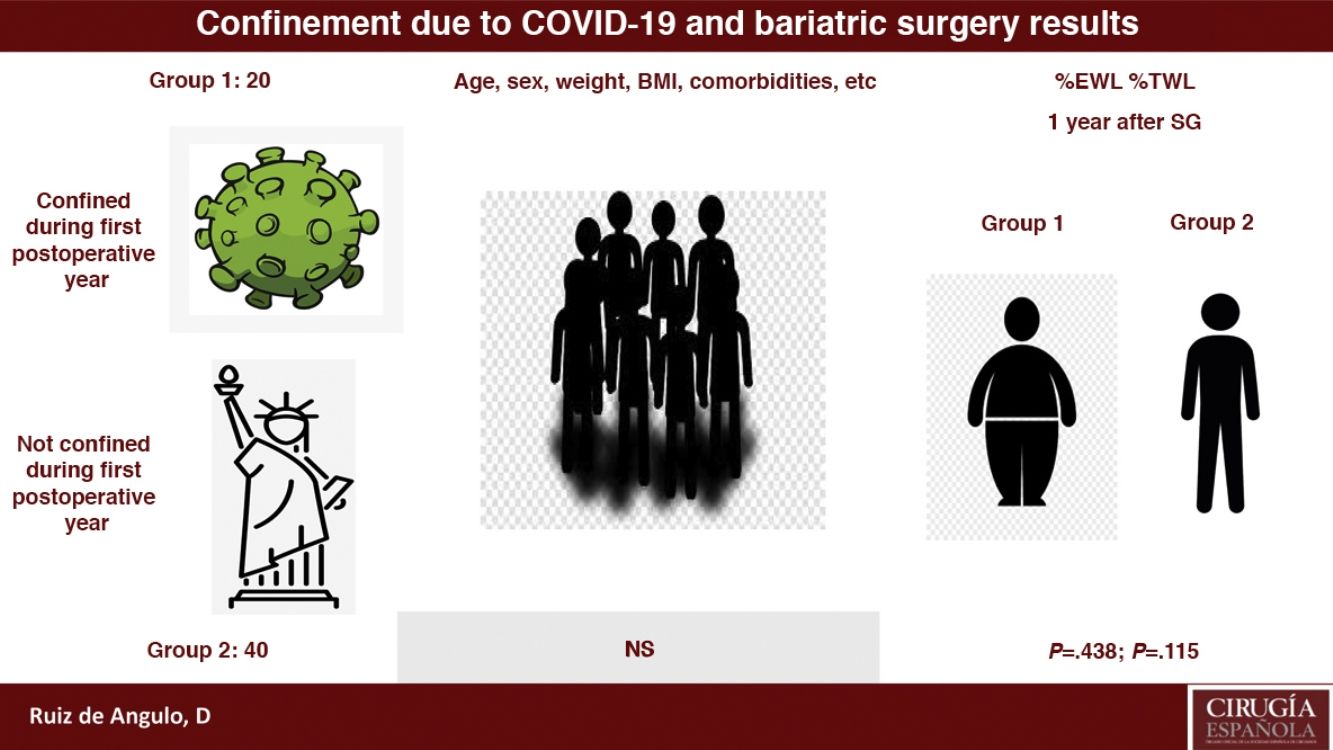
COVID-19 pandemic has lead to lockdown of population in many countries. In Spain, the state of alarm was established from March 15 to June 20, 2020. Usually this fact decreased people's mobility and physical activity, in addition to producing or exacerbating psychological disorders. Our aim was to determine the influence that this condition had over the short-term ponderal results of patients undergoing laparoscopic vertical gastrectomy from May 2019 to May 2020.
MethodsCase–control study for comparing the percentage of excess weight lost (%EWL) and the percentage of total weight lost (%TWL) of patients that underwent a VG during the last year, so they were affected by lockdown in April and part of March 2020 (group 1), to the %EWL and %TWL of a control group (group 2), obtained from our previous series.
ResultsThe mean %EWL in group 1 is 47.37±18.59 and in group 2 is 51.13±17.59, being P=.438. Meanwhile, the mean %TWL in group 1 is 21.14±8.17 and in group 2 is 24.67±8.01, with P=.115.
ConclusionsPopulation lockdown by COVID-19 did not get worse short-term results of vertical gastrectomy. More studies with a larger number of patients are necessary to draw firm conclusions.
La pandemia por COVID-19ha obligado al confinamiento de la población en muchos países. En España, el estado de alarma se estableció desde el 15 de marzo al 20 de junio del 2020. Este hecho, por lo general, disminuyó la movilidad y la actividad física de las personas, además de producir o exacerbar alteraciones psicológicas. Nuestro objetivo es analizar la influencia que esta situación ha ejercido sobre los resultados ponderales a corto plazo de los pacientes tratados mediante una gastrectomía vertical laparoscópica entre mayo del 2019 y mayo del 2020.
MétodosEstudio de casos y controles donde se compararon el porcentaje de exceso de peso perdido (%EWL) y el porcentaje de peso total perdido (%TWL) de los pacientes intervenidos en el último año y a los que ha afectado el confinamiento durante el mes de abril y parte de marzo del 2020 (grupo 1; n=20), con el de un grupo control (grupo 2; n=40) de nuestra casuística previa.
ResultadosEl %EWL medio en el grupo 1 es de 47,37±18,59 y en el grupo 2 es de 51,13±17,59, siendo la p=0,438. Por su parte, el %TWL medio en el grupo 1 es de 21,14±8,17 mientras que en el grupo 2 es de 24,67±8,01, resultando la p=0,115.
ConclusionesEl confinamiento de la población por COVID-19 no empeoró los resultados ponderales a corto plazo de la gastrectomía vertical. Son necesarios más estudios con un mayor número de pacientes para obtener conclusiones más sólidas.
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is the most important pandemic that humans have experienced as a species in recent decades, causing thousands of deaths around the world.1 In Spain, as in other countries,2 the population was confined to their homes for much of the month of March and the entire month of April, followed by different phases of de-escalation. The difficulty to perform normal physical activity during this period, as well as the appearance or worsening of different psychological syndromes derived from this situation,3 leads us to assume that the short-term weight-loss results after bariatric surgery would not be ideal. Since the first year after bariatric surgery is very important to achieve considerable weight loss,4 and given the consequent motivational implications and positive reinforcement resulting from this phenomenon, we believe that it is of great importance to quantify the influence that confinement has had on our patients. This is especially true since the epidemiological situation is still not under control, and it is unknown whether the appearance of new outbreaks will again require drastic social isolation measures in the near future.
Therefore, our objective is to quantify the weight-loss results obtained in patients whose first postoperative year included the period of confinement due to COVID-19. These results were compared with those from a control group whose first year after the bariatric procedure was not affected by the consequences of confinement due to the pandemic.
MethodsIn the Esophagogastric Surgery and Obesity Unit of the Hospital Universitario Virgen de la Arrixaca, we conducted this retrospective study of cases and controls using a prospective database, data obtained through telephone consultations, and data recorded in computerized patient medical records.
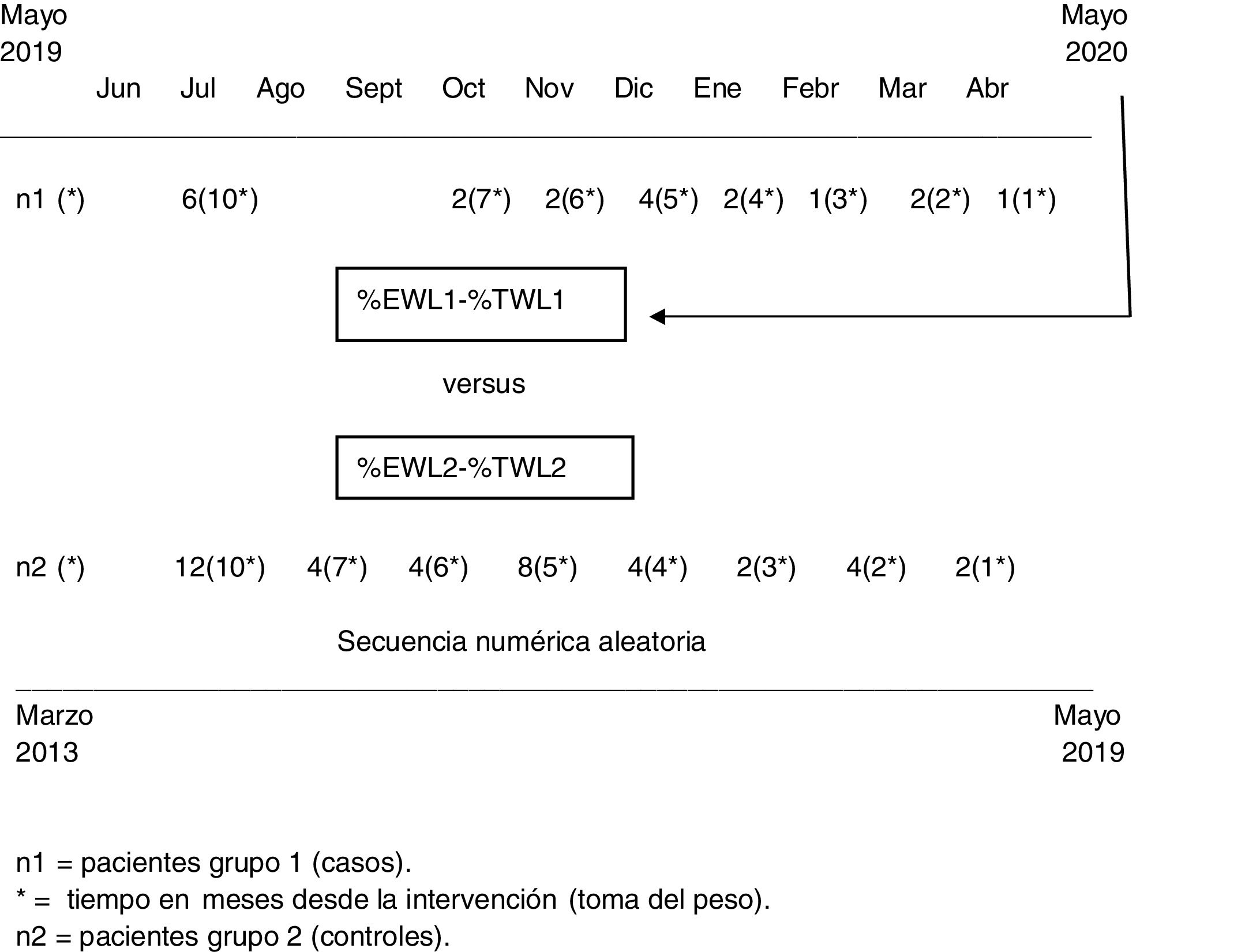
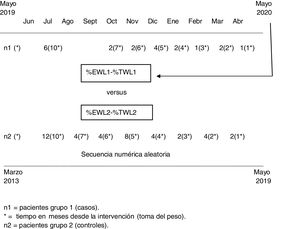
Group 1 (cases) included patients who underwent laparoscopic sleeve gastrectomy (SG) from May 2019 to May 2020 and who were therefore affected by the lockdown during the first postoperative year. We collected epidemiological characteristics and the current weight of the patients, as well as the time since the operation, in months. Group 2, the control group, was obtained from cases treated by our unit prior to the study period (March 2013–May 2019) and included twice as many patients as the cases from group 1. The cases and controls were organized by periods according to the time elapsed since the operation, and twice as many control cases were randomly chosen as patients. In other words, if the weight after one month was available for one case, the weight after one month was collected for 2 controls (Fig. 1). The selection of the control patients in group 2 was carried out using a random numerical sequence in the general database of our registered cases, where patients are organized chronologically by the date of surgery. Therefore, in the results, the numerical values of the percentage of excess weight lost (%EWL) or the percentage of total weight lost (%TWL) in each group were not relevant, since they represent mean patient weight at different times after surgery. What is interesting is the comparison between groups, since we tried to eliminate this bias by creating a control group with exactly twice the number of determinations, but at the same moments in time after the operation.
The surgical technique has undergone no modifications since the beginning of our surgical activity, and certain details have been described in previous studies.5,6 The %EWL was calculated with the Metropolitan Life Insurance formula; the %TWL for each patient in the two groups and their means were compared between cases and controls. A descriptive statistical analysis was conducted for each of the variables contemplated, using the median (range) and the mean (standard deviation) for continuous variables depending on whether their distribution was non-normal or normal, respectively. The distribution of these variables was analyzed using the Kolmogorov–Smirnov or Shapiro–Wilk statistical tests, as appropriate. For qualitative variables, absolute frequencies and their relative frequencies were used. For the study of the relationship between the variables, the chi-square test was applied, including the analysis of residuals between 2 qualitative variables, the Pearson correlation if the variables were quantitative, and the comparison of means (Student's t) or the Mann–Whitney U, as appropriate for the study of the relationship between a qualitative and a quantitative variable. In all situations, an association with a P value less than .05 was considered statistically significant. All data were analyzed with IBM SPSS statistics v.24 (SPSS, Inc. Chicago, IL, USA).
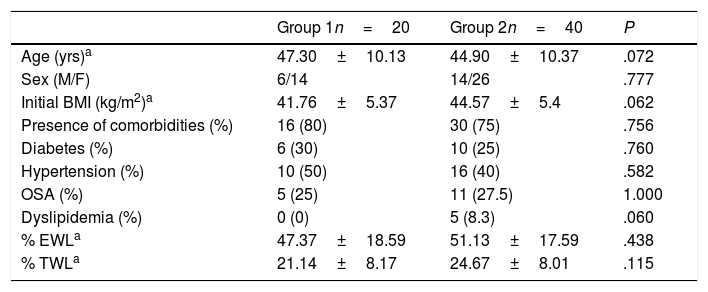
ResultsFrom May 2019 to May 2020, 20 patients (group 1) underwent SG in our unit. Specifically, and as of this writing, 6 patients underwent surgery 10 months ago, 2 patients 7 months ago, 2 patients 6 months ago, 4 patients 5 months ago, 2 patients 4 months ago, one patient 3 months ago, 2 patients 2 months ago, and one patient had only one month of postoperative follow-up (Fig. 1). Group 2 was made up of 40 patients evenly distributed among the different postoperative follow-up times at a ratio of 1:2 (one case for every 2 control subjects). Group 2 is homogeneous with group 1, as shown in Table 1. There were no differences between the two groups in terms of age, sex, presence of comorbidities, diabetes, arterial hypertension, dyslipidemia, or obstructive sleep apnea (OSA).
Epidemiological characteristics and weight-loss results for both groups.
| Group 1n=20 | Group 2n=40 | P | |
|---|---|---|---|
| Age (yrs)a | 47.30±10.13 | 44.90±10.37 | .072 |
| Sex (M/F) | 6/14 | 14/26 | .777 |
| Initial BMI (kg/m2)a | 41.76±5.37 | 44.57±5.4 | .062 |
| Presence of comorbidities (%) | 16 (80) | 30 (75) | .756 |
| Diabetes (%) | 6 (30) | 10 (25) | .760 |
| Hypertension (%) | 10 (50) | 16 (40) | .582 |
| OSA (%) | 5 (25) | 11 (27.5) | 1.000 |
| Dyslipidemia (%) | 0 (0) | 5 (8.3) | .060 |
| % EWLa | 47.37±18.59 | 51.13±17.59 | .438 |
| % TWLa | 21.14±8.17 | 24.67±8.01 | .115 |
Regarding the assessment of the weight-loss results, we observed that there were no statistically significant differences in either the %EWL or %TWL between the two groups, although poorer results were observed in the patients in group 1 (%EWL=47.37±18.59; %TWL=21.14±8.17) versus group 2 (%EWL=51.13±17.59; %TWL=24.67±8.01).
DiscussionBariatric surgery is the most effective and long-lasting treatment for morbid obesity today. Several studies support its cost-benefit ratio by providing a significant reduction in weight, as well as the resolution or substantial improvement of various associated comorbidities.7,8 All this results in lower pharmaceutical costs, as well as the greater work capacity and productivity of these patients. However, weight loss is more evident during the first year after the procedure, which increases motivation and establishes healthy lifestyle habits in many patients. One of these pillars is physical activity,9 which is especially important in subjects who have undergone a restrictive technique like SG, and a physical training program has been shown to prevent weight regain in the medium term, reducing body fat, glycemia and cholesterol.10
As a result of COVID-19, the Spanish population was confined to their homes, which reduced the mobility and physical exercise of most individuals, causing stress and fear in addition to addictions, depression, and even suicide.11–14 In this context, it would be concerning if bariatric surgery did not meet the excellent previous results and durability, since its cost-effectiveness could be called into question.
In our study, we were unable to demonstrate that confinement had a decisive or significant effect on short-term weight results, although poorer results were observed. We believe, however, that an increase in the number of cases could amplify this difference, since a preliminary calculation of the sample size required the recruitment of 135 patients per group, which was impossible in our case. Another limitation of the study is that some weight data of the patients in group 1 were obtained over the telephone, with possible variabilities resulting from the moment and the tool with which they were calculated.
Several authors have denounced the injustice that the approach to the COVID-19 pandemic has represented for the morbidly obese. This is mainly because other surgical procedures have been prioritized over bariatric surgery, and there has also been increased stigmatization that this situation has generated in this subgroup of patients.15 Other authors have described prioritization protocols for both bariatric and metabolic surgery.16 Even so, it is difficult to guess the evolution of the pandemic and whether confinement and social isolation will be imposed again. Bariatric surgery is the best treatment for thousands of people who have a serious illness, so we must demand its continuity from the competent authorities.17 Nevertheless, we must ensure that treatment results will continue to meet the established standards. Given the unpredictable evolution of the global COVID-19 pandemic, the nutritional and psychological support of patients undergoing surgery as well as those on the surgical waiting list18 should be fomented. In addition, the frequency of multidisciplinary committees should be increased in order to establish priorities until the healthcare situation is normalized. Finally, further studies are necessary with a greater number of patients to determine the actual influence that the confinement (and potential future confinements) has had on weight-loss results in order to develop transparent, effective protocols.
ConclusionsThe confinement of the population in Spain during the months of March, April and May 2020 did not significantly alter the %EWL or the %TWL of patients who underwent SG compared to patients whose first postoperative year was not affected by the COVID-19 pandemic. However, more studies with larger samples are necessary to reach more solid conclusions.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Ruiz de Angulo D, Balaguer Román A, Munitiz Ruiz V, Gil Vázquez PJ, Ruiz Merino G, Ortiz Escandell MÁ, et al. Influence of the lockdown due to COVID-19 on weight-loss results during the first year after sleeve gastrectomyInfluence of the lockdown due to COVID-19 on weight-loss results during the first year after sleeve gastrectomy. Cir Esp. 2021;99:428–432.