Laparoscopic Heller myotomy has become the gold standard procedure for patients with achalasia. This study evaluates the clinical status, quality of life, and functional outcomes after laparoscopic Heller myotomy.
Materials and methodsWe analysed patients who underwent laparoscopic Heller myotomy with an associated anti-reflux procedure from October 1998 to December 2010. Before surgery, we administered a clinical questionnaire and as of 2002, we also evaluated quality of life using a specific questionnaire (GIQLI). In 2011, we performed a follow-up for all available patients. We administered the same clinical questionnaire and quality of life test as before surgery and performed manometry and 24-h pH monitoring. According to the length of follow up, patients were divided into 3 groups. Group 1 with a follow-up between 6 and 47 months; group 2 with a follow-up between 48 and 119 months, and group 3 with a follow-up of more than 120 months. Moreover, 27 patients had already been evaluated with this same protocol in 2003. Pre- and postoperative data were compared for the 3 groups and for patients who completed follow up in 2003 and 2011.
ResultsNinety-five patients underwent laparoscopic Heller myotomy. Seventy-six (80%) patients were available for follow-up. Mean follow-up was 56 months (range 6–143). Global improvement in dysphagia was 89%. Total DeMeester score decreased in the 3 groups. GIQLI scores improved after surgery, reaching normal values. Manometric determinations showed normal LES pressures after myotomy in the 3 groups. Ten percent of overall 24-h pH monitoring was abnormal. The group of patients followed up in 2003 and in 2011 showed no impairment in the variables studied in the long term.
ConclusionsLong-term follow-up of the laparoscopic approach to achalasia showed good results concerning clinical status and quality of life, with normal sphincteric pressures and a low incidence of gastroesophageal reflux.
La miotomía laparoscópica se ha convertido en el tratamiento de elección en los pacientes con acalasia. Este estudio evalúa a largo plazo el estado clínico, de calidad de vida y los resultados funcionales posteriores a la miotomía de Heller laparoscópica.
Material y métodosSe analizó a los pacientes diagnosticados de acalasia primaria e intervenidos mediante una miotomía de Heller laparoscópica con un procedimiento antirreflujo desde octubre de 1998 hasta diciembre de 2010. Previamente a la intervención, se evaluó la sintomatología de los pacientes mediante un cuestionario específico (escala DeMeester) y desde el 2002 se evaluó la calidad de vida mediante un test validado (GIQLI). En el año 2011 se reevaluó el estado clínico y de calidad de vida, y además se realizó una manometría y una pHmetría de 24h. En función del tiempo de seguimiento, los pacientes fueron divididos en 3 grupos (grupo 1: seguimiento entre 6 y 47 meses; grupo 2: seguimiento entre 48 y 119 meses y grupo 3, seguimiento superior a 120 meses). Además, 27 pacientes de la serie fueron evaluados con el mismo protocolo en 2003 y reevaluados en 2011.
ResultadosNoventa y cinco pacientes fueron incluidos en el estudio. El 80% (n=76) estuvieron disponibles para realizar el seguimiento. El tiempo de seguimiento medio fue de 56meses (rango 6–143meses). La mejoría global de la disfagia fue del 89%. Los valores estudiados mediante la escala de DeMeester descendieron significativamente en los 3 grupos y los índices de calidad de vida se normalizaron posteriormente a la cirugía. Las determinaciones manométricas mostraron la normalización mantenida en la presión del esfínter esofágico inferior en todos los grupos. Se detectó una incidencia de reflujo gastroesofágico del 10%. En el subgrupo de pacientes analizados prospectivamente en 2003 y 2011, no se demostró empeoramiento de los resultados a largo plazo.
ConclusionesLa miotomía de Heller laparoscópica mejora la clínica y la calidad de vida de los pacientes con acalasia primaria manteniendo las presiones del esfínter esofágico inferior normales a largo plazo, con una baja tasa de incidencia de reflujo gastroesofágico.
Achalasia is an oesophageal motor disorder with no known definitive treatment. Altered oesophageal motility and the inability of the lower oesophageal sphincter (LOS) to relax leads to a difference in pressures when the food bolus is passed, which produces dysphagia, regurgitation, and chest pain, among other symptoms.1,2 The only effective treatment is the reduction of LOS pressure, either through the injection of muscle relaxants such as botulinum toxin, or the destruction of muscular fibres through endoscopic dilatation, or laparoscopic myotomy.3
Laparoscopic myotomy has become the gold standard treatment for achalasia. Csendes and Ortiz’ publication on long term outcomes showed that excellent results were achieved from an open surgery approach, even after a 30-year follow-up.4,5 Although there are no randomised prospective studies which compare the open approach with laparoscopic approach, the latter is currently accepted as the best surgical option. However, as laparoscopic myotomy has been used for less than 20 years, there are no long-term follow-up studies.
The aim of this study is to evaluate the clinical outcomes, quality of life, and functional outcomes of laparoscopic Heller myotomy in 3 patient groups, divided according to post-operative follow-up time up to more than 10 years.
Materials and MethodsSampleAll patients diagnosed with achalasia that underwent laparoscopic Heller myotomy between October 1998 and December 2011 were retrospectively analysed. Data from all patients were prospectively collected in the advanced laparoscopic surgery database of the Surgery Department of the Santa Creu i Sant Pau Hospital. The patients were monitored between June and December 2011 in the outpatient department. Depending on follow-up time after surgery, the patients were divided into 3 groups. Group 1: patients with a follow-up between 6 and 46 months; group 2: patients with follow-up of between 48 and 119 months; and group 3: patients with follow-up of over 120 months (10 years). Furthermore, analysis was performed on a patient subgroup that was assessed in 2003 following the same protocol as 2011. Pre and post operative data were compared for all groups.
Pre-operative AssessmentAll patients were diagnosed with achalasia following clinical suspicion as a result of the presence of dysphagia and regurgitation. A gastroscopy, oesophagogram, and oesophageal manometry were performed in all cases to establish diagnosis and rule out secondary causes. Symptom duration and use of endoscopic treatment prior to surgery were recorded.
The scale proposed by Johnson and DeMeester6 was used to assess the patient's clinical symptoms preoperatively. This scale classifies dysphagia, regurgitation, chest pain, and heartburn into 4 grades, 0 being absence of symptoms and 3 the presence of symptoms on a daily basis.
To assess quality of life, the GI quality of life index (GIQLI) was used, which in 2001 was validated for use in Spanish. This index contains 36 questions in 5 sections which cover GI symptoms and the emotional, physical, and social dysfunction of the condition for the patient. Each question scores from 0 (lowest possible score) to 4 points (highest possible score). The index has a maximum of 144 points, with an established normal score of 125.8 points (95% confidence interval: 121.5–127.5)7,8 for healthy individuals.
Surgical TechniqueFive trocars were used for the laparoscopic approach of the oesophageal hiatus. Following minimum dissection of the anterior side of the gastroesophageal junction, the cardial fatty tissue was dissected from left to right, including the left vagus nerve to prevent injury. The myotomy was started in the longitudinal muscle layer, separating its fibres down to the transverse muscle layer, which was sectioned. The myotomy was extended 6cm cranially and 2cm towards the distal part of the gastroesophageal junction. Once the myotomy was completed, a routine intraoperative endoscopy was performed to ensure that there were no residual fibres. A Dor or Toupet9 type fundoplication was then applied.
Post-operative Follow-upAll patients were monitored as outpatients following surgical intervention. In 2003 (n=27) and 2011 (n=76) they were called for specific monitoring, consisting of an assessment of their clinical symptoms according to the DeMeester scale, a new quality of life assessment using the GIQLI, and manometry and pHmetry to evaluate LOS functioning.
- a)
Manometry. Fasting for 12h was prescribed, together with avoidance of drugs which could alter oesophageal motility. The parameters used for the LOS evaluation were pressure at rest, length and percentage of postprandial gastric relaxation. Incomplete LOS relaxation and aperistalsis of the oesophageal body were the manometric diagnostic criteria of achalasia. Baseline pressure was recorded for analysis.
- b)
24h pHmetry. A 2-channel catheter was used. The distal channel was placed 5cm above the manometrically measured LOS. The proximal channel was positioned 10cm above this. The patients recorded information regarding their symptoms in a diary whilst recording pH variations on a laptop (Medtronic Inc., Minneapolis, Minn, USA). All data were downloaded into a specific programme. The test was considered pathological when the time percentage of pH<4 in the distal channel was above 4. A pathological result indicated fibrogastroscopy.
Continuous variable data were expressed as standard deviations, except ordinal variables which were expressed as medians. The Student's t-test and Wilcoxon tests were used. Non-paired variables were analysed using the Anova test. Statistical significance was fixed as P<.05. All calculations were performed using SPSS 19.0 (SPSS Inc., Chicago, IL, USA.).
ResultsPre-operative DataFrom 1998 to 2010, 95 laparoscopic Heller myotomies were performed: 55 on men (58%) and 40 on women (42%) with a mean age of 45 (15–81). Average duration of symptoms until surgery was 52 months (4–360 months). Twenty-five patients (26%) had received endoscopic treatment prior to surgery. Of these, 23 had previous dilatation and 2 had received botox treatment. The overall pre-operative sphincter pressure was 31mm Hg (12–60mm Hg).
Operative Data and Immediate Post-operative ResultsA total of 91 patients were treated using a Heller–Dor procedure and 4 patients using a Heller–Toupet procedure. Average operative time was 126min (75–270min). Three oesophageal perforations were defined which were repaired intraoperatively. Conversion to open surgery was required in 2 cases for haemostatic control in one and the inability to establish pneumoperitoneum due to adhesions in the other. Post-operative complications consisted of the appearance of a retro-oesophageal fistula and abscess. Both were treated conservatively. Mean hospital stay was 3 days (1–17 days). There were no fatalities.
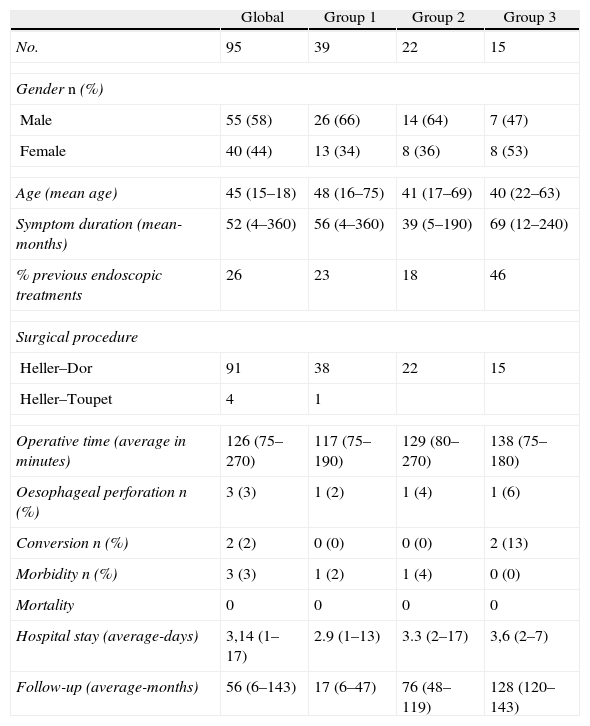
Follow-upIn 2011, 76 of the 95 patients (80%) were available for structured follow-up monitoring. 19 patients could not be assessed: 2 presented cognitive impairment, 6 had moved abroad and 9 could not be located. Mean follow-up time was 56 months (6–143 months). The patients were divided into 3 groups according to post-operative follow-up time. There were 39 patients (51%) in group 1 with a mean follow-up time of 17 months (6–47m). There were 22 patients (29%) in group 2 with a follow-up time of 76 months (48–119m) and there were 15 patients (20%) in group 3 with a follow-up time of 125 months (120–143m). The demographic data are shown in Table 1.
Demographic Data From Study Groups.
| Global | Group 1 | Group 2 | Group 3 | |
| No. | 95 | 39 | 22 | 15 |
| Gender n (%) | ||||
| Male | 55 (58) | 26 (66) | 14 (64) | 7 (47) |
| Female | 40 (44) | 13 (34) | 8 (36) | 8 (53) |
| Age (mean age) | 45 (15–18) | 48 (16–75) | 41 (17–69) | 40 (22–63) |
| Symptom duration (mean-months) | 52 (4–360) | 56 (4–360) | 39 (5–190) | 69 (12–240) |
| % previous endoscopic treatments | 26 | 23 | 18 | 46 |
| Surgical procedure | ||||
| Heller–Dor | 91 | 38 | 22 | 15 |
| Heller–Toupet | 4 | 1 | ||
| Operative time (average in minutes) | 126 (75–270) | 117 (75–190) | 129 (80–270) | 138 (75–180) |
| Oesophageal perforation n (%) | 3 (3) | 1 (2) | 1 (4) | 1 (6) |
| Conversion n (%) | 2 (2) | 0 (0) | 0 (0) | 2 (13) |
| Morbidity n (%) | 3 (3) | 1 (2) | 1 (4) | 0 (0) |
| Mortality | 0 | 0 | 0 | 0 |
| Hospital stay (average-days) | 3,14 (1–17) | 2.9 (1–13) | 3.3 (2–17) | 3,6 (2–7) |
| Follow-up (average-months) | 56 (6–143) | 17 (6–47) | 76 (48–119) | 128 (120–143) |
Seven of the 27 patients with a structured follow-up in 2003 did not take part in the 2011 control. Out of the remaining 20 patients, average follow-up time in the first control was 36 months (15–57 months) and in the second control it was 125 months (115–143 months).
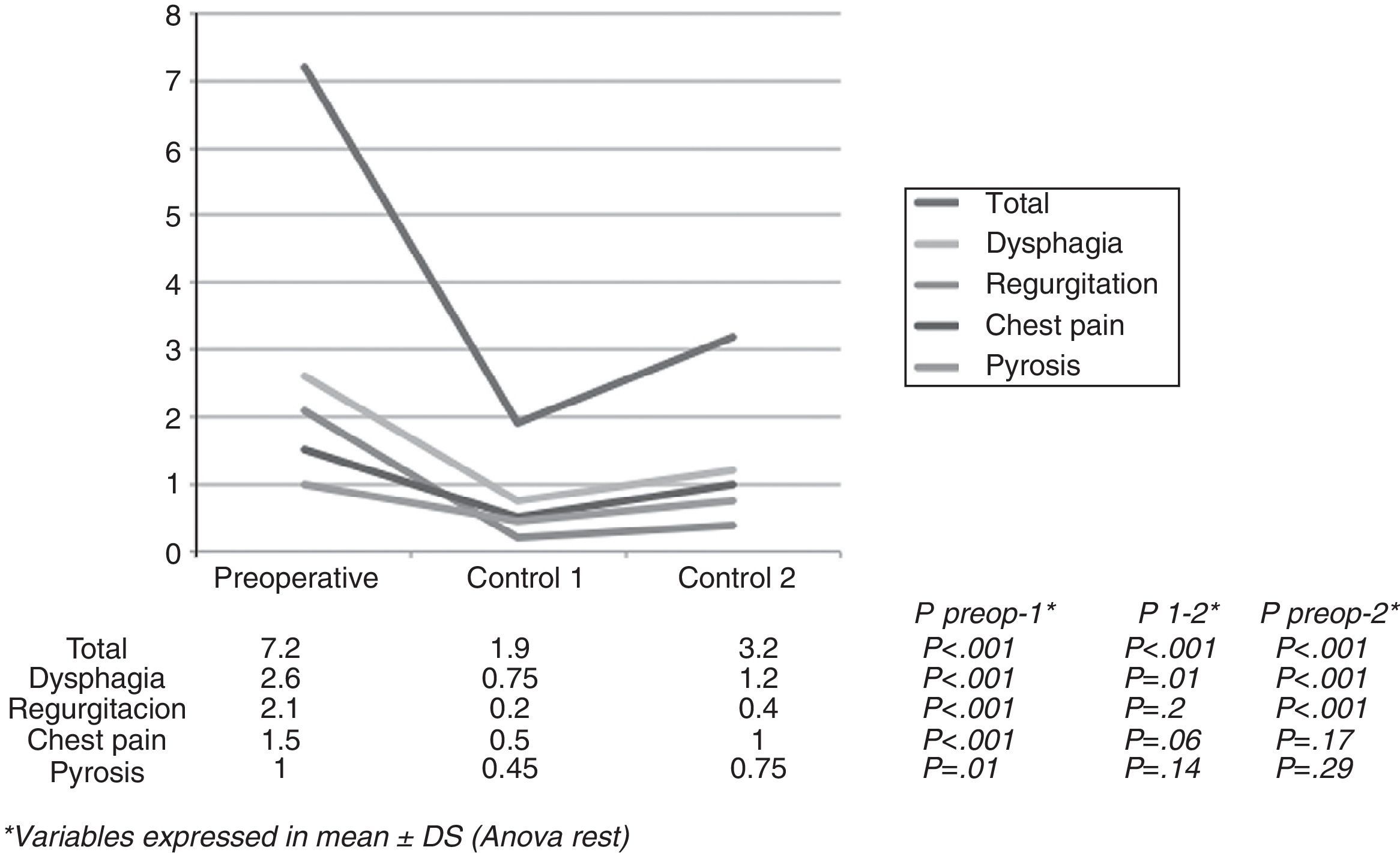
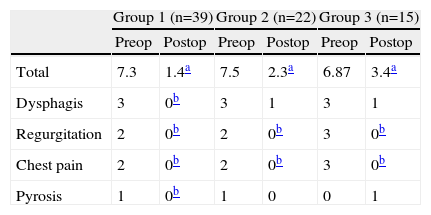
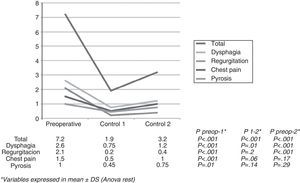
Analysis of Clinical SymptomsThe overall score according to the DeMeester scale significantly improved in the 3 groups after myotomy. The mean pre-operative score for dysphagia was 3 in all groups. In group 1 this score fell to 0 points and in groups 2 and 3, it fell to 1 point. After surgery, regurgitation and chest pain were significantly reduced to 0 in all groups. Heartburn, however, worsened in group 3 from 0 to 1 point with no statistical significance (Table 2).
In the patient cohort with a prospective follow-up in 2003 and 2011, an improvement in all symptoms was observed in the first control, after mean follow-up of 36 months (15–57 months). In the second control, after an average of 125 months follow-up after surgery (115–143 months), these scores were slightly less but remained lower than pre-operative scores (Fig. 1)
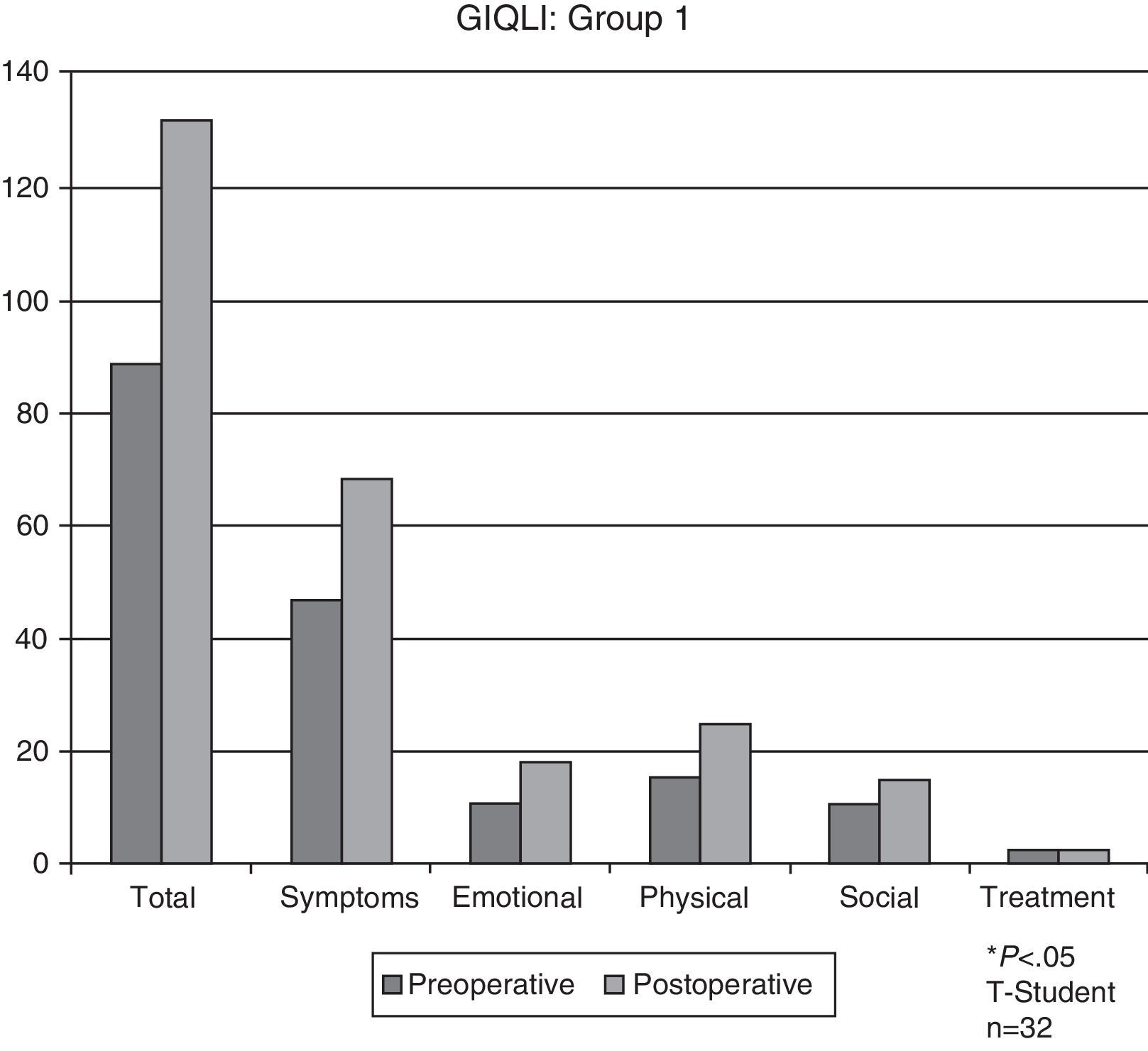
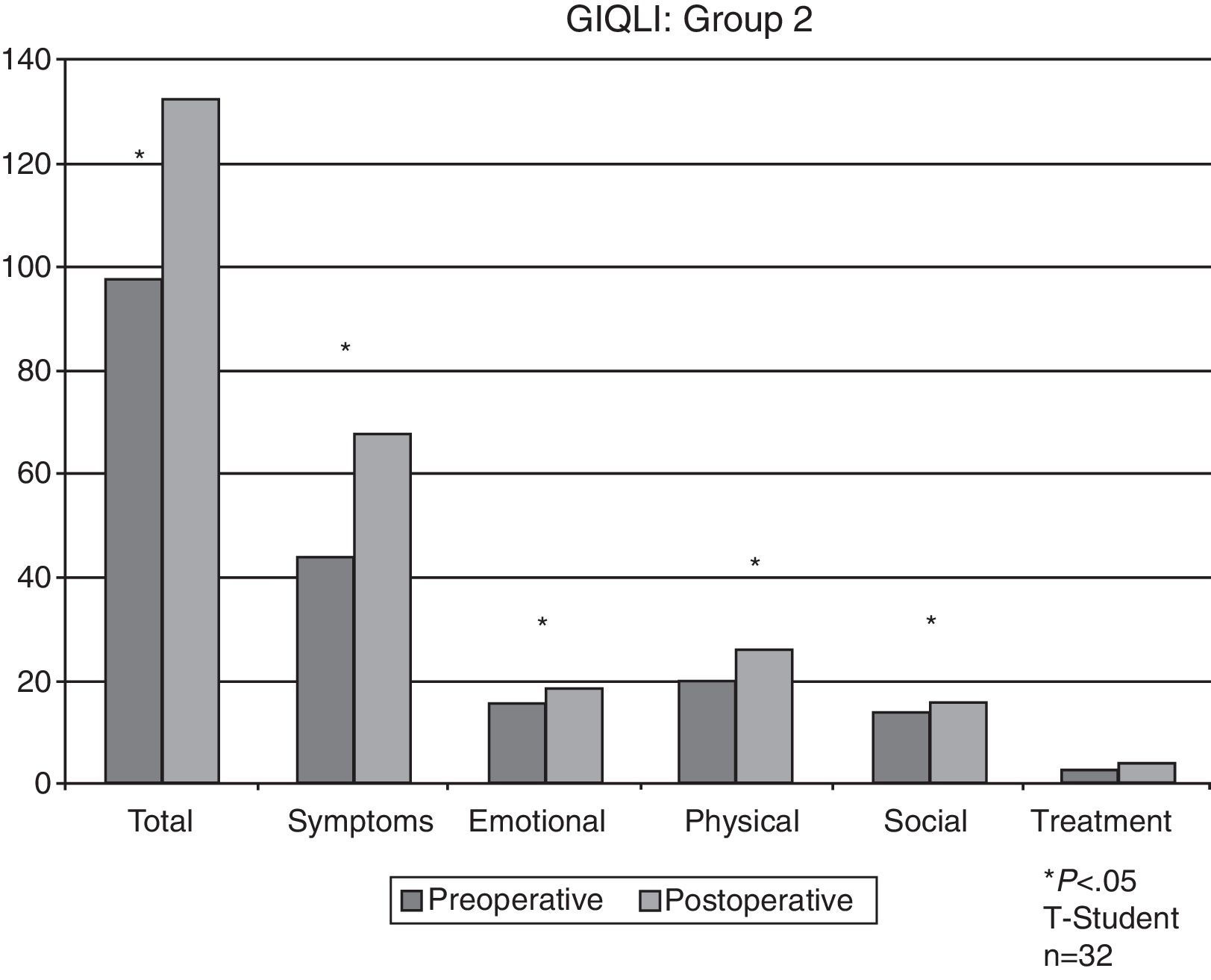
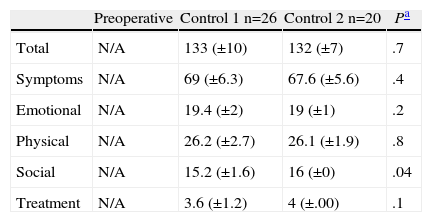
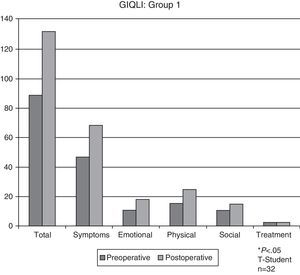
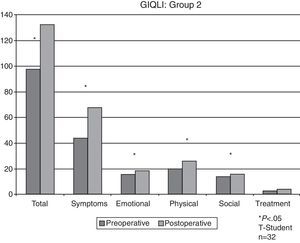
Quality of Life AnalysisAll preparatory quality of life rates were abnormal. Group 1 showed an improvement of 89 (±21) to 133 (±10) points and group 2 an improvement of 98 (±16) to 133 (±7) points (P<.05). There was no pre-operative quality of life control in group 3 since scale use began in 2002. However, the rate for this group was 132 (±8) in post-operative monitoring.
The patient subgroup analysed prospectively did not have a preparatory quality of life assessment either. In the 2003 control total GIQLI was 133 (±10) points and in the second control it was 132 (±7) points (Figs. 2–3 and Table 3).
Results of Quality of Life in the Prospectively Controlled Patient Subgroup.
| Preoperative | Control 1 n=26 | Control 2 n=20 | Pa | |
| Total | N/A | 133 (±10) | 132 (±7) | .7 |
| Symptoms | N/A | 69 (±6.3) | 67.6 (±5.6) | .4 |
| Emotional | N/A | 19.4 (±2) | 19 (±1) | .2 |
| Physical | N/A | 26.2 (±2.7) | 26.1 (±1.9) | .8 |
| Social | N/A | 15.2 (±1.6) | 16 (±0) | .04 |
| Treatment | N/A | 3.6 (±1.2) | 4 (±.00) | .1 |
In the 2011 control a manometry was performed on 37 patients (49%). Eleven patients (14%) did not tolerate this test and 28 patients (37%) refused it.
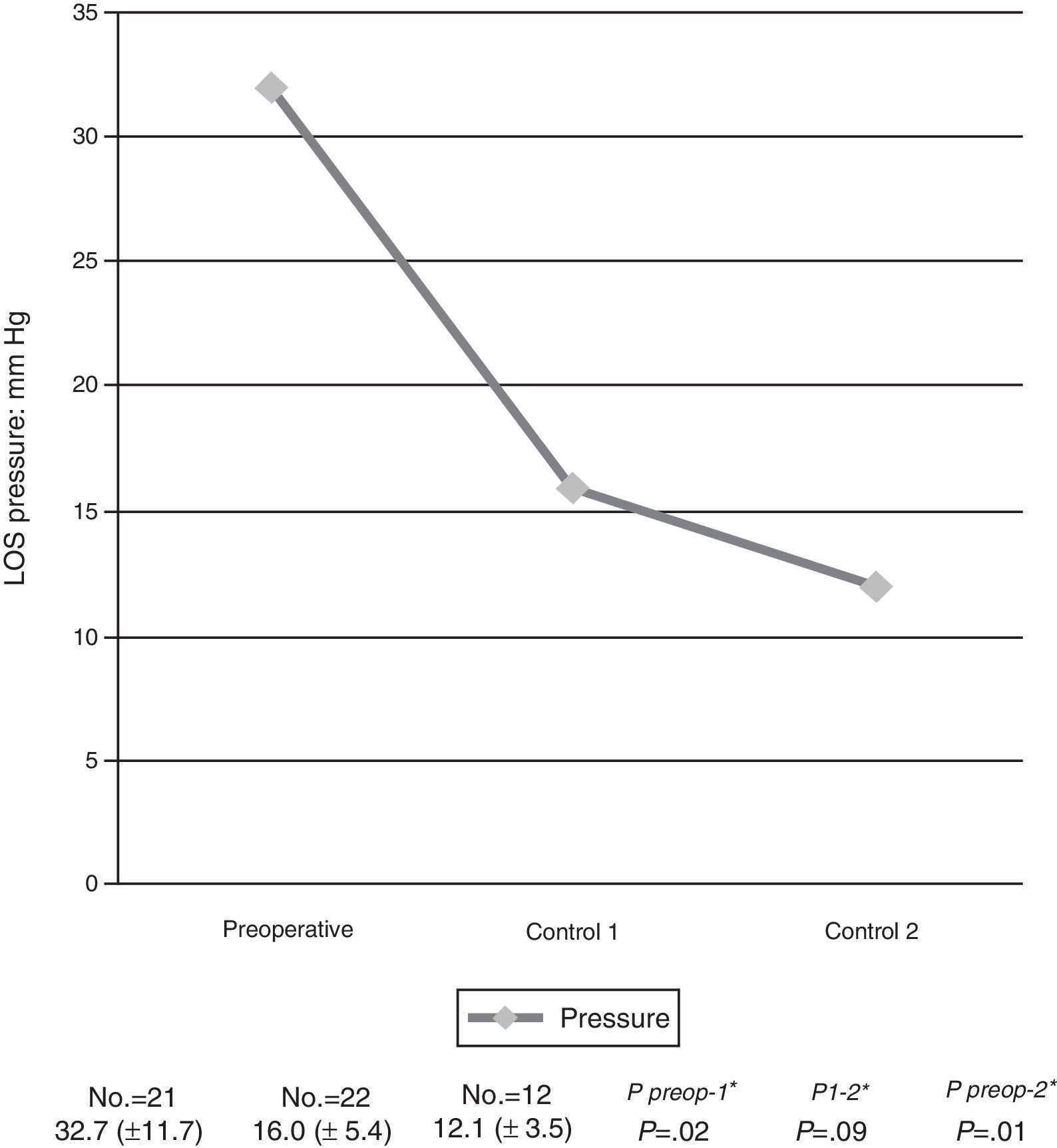
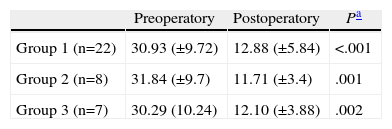
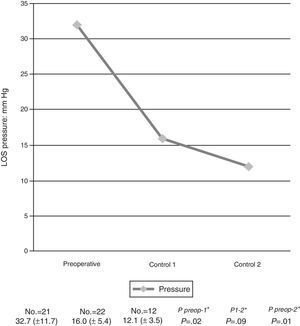
Average LOS pressure reduction in all patients ranged from 31mm Hg (range: 12–60) to 12.5mm Hg (range 4.9–30; P<.001).
In group 1 it fell from 30.9mm Hg (±9) to 12.8mm Hg (±5) (P<.001), in group 2 from 31.8mm Hg (±9) to 11.7mm Hg (±3) (P=.01), and in group 3 from 30.2mm Hg (±10) to 12.1mm Hg (±4) (P=.002).
In the prospectively controlled subgroup, pressure fell from 32.7mm Hg (±7) to 16mm Hg (±5) (P<.005) in the initial 2003 control. Pressure from these patients remained at 12.1mm Hg (±3) in the second control of 2011 (P=.09). The results are shown in Table 4 and Fig. 4.
Manometric Results According to Groups.
| Preoperatory | Postoperatory | Pa | |
| Group 1 (n=22) | 30.93 (±9.72) | 12.88 (±5.84) | <.001 |
| Group 2 (n=8) | 31.84 (±9.7) | 11.71 (±3.4) | .001 |
| Group 3 (n=7) | 30.29 (10.24) | 12.10 (±3.88) | .002 |
P<.05.
In 2011 pHmetry could be performed on 41 patients (54%). Twenty one patients (28%) rejected the procedure and another 14 (18%) could not tolerate it.
Normal pHmetry rates were 90%. Median time percentage of pH<4 in the distal canal was one.
Two patients from group 1 had abnormal pHmeter (9%) readings. No patient in group 2 had an abnormal pHmetry and in group 3 there were 2 abnormal readings (22%). Patients with abnormal pHmetries were referred for upper endoscopy. There were no signs of oesophagitis or Barrett's oesophagus. These patients were treated systematically with proton pump inhibitors.
RecurrencesRecurrence of the disease or failure of the surgical treatment was defined as a maximum postoperative dysphagia score on the DeMeester scale (grade 3), or the need for endoscopic treatment after surgery (dilatation) to alleviate dysphagia, even if scores were not maximum.
Recurrence rate was 10% (8 patients), detected at an average post-operative of 78 months (range 12–143 months). Three recurrences were identified in group 1, 2 in group 2, and 3 in group 3. Six of these patients were referred for endoscopic dilatation and 2 refused further treatment. Recurrences were included in data analysis.
DiscussionThis study confirms the excellent results of laparoscopic Heller myotomy, even in the long term. These results were seen in 3 patient groups with the same baseline characteristics, analysed at different post-operative follow-up stages. The same cohort of patients was also prospectively assessed in 2 consecutive controls, in some cases after more than 10 years from surgery. The added value of this study was that clinical symptoms, quality of life, manometric variations of LOS pressure and gastroesophageal reflux were assessed simultaneously after laparoscopic myotomy.
In this series, the total value of the DeMeester scale, dysphagia, regurgitation and chest pain diminished in the 3 groups. However, statistical significance did decrease as the follow-up period lengthened. Recurrence of dysphagia long term has already been described by the authors who analysed long term results of myotomy by the laparotomic approach.4,5 Patients with achalasia presented aperistalsis of the oesophagus, and for this reason LOS ablation alone is not a definitive solution to the disease. Analysis of the pyrosis showed an erratic evolution, since the groups with shorter follow-up periods (1 and 2) showed a reduction in symptoms, whilst in the group with a follow-up of over 10 years, the symptom worsened but without any statistical significance.
When the 2003 and 2011 prospectively monitored patient subgroup symptoms were analysed, an impairment of the clinical improvement obtained in the first control compared to the second control over 10 years later was noted, although these values were lower than the pre-operative ones. Few series in the literature have reported long term results (over 10 years) for the laparoscopic approach to achalasia. Cowgill et al.10 analysed a series of 33 patients who had undergone a laparoscopic myotomy 10 years previously, observing a long term improvement in the severity and frequency of the most characteristic symptoms of the disease. Jeansonne et al.11 also showed good results in a group of 20 patients prospectively controlled with a mean follow-up of 11.2 years. These authors reported the absence of dysphagia in 47% of the series, and in the other 47% dysphagia was considered mild to moderate. As in this study, control results were compared for over 10 years with a prior control at 27 postoperative months with no significant differences between both controls.
Achalasia alters patients’ quality of life. Since 2002 the quality of life of these patients was systematically analysed using a specific index for digestive disorders (GIQLI). Real improvement in the postoperative quality of life in all groups was observed. Moreover, in the prospectively controlled patient group, the indices remained the same in the controls undertaken 3 and 10 years after myotomy. Few publications have analysed quality of life after achalasia using the GIQLI, and none have analysed it long term. Ferulano et al.12 reported an increase of 78–115 points in a sample of 31 patients with a follow-up of 49 months (range 24–72 months). Decker et al.13 also showed an improvement in the GIQLI indices of 84 to 119 points, in a group of 40 patients at a median follow-up of 31 months.
Decreasing LOS pressure is the only effective treatment for the disease, as it provides greater oesophageal evacuation. In this study we observed that LOS pressure decreased in the 3 groups, showing that laparoscopic myotomy leads to normal sphincteric pressures in the short, medium, and long term. In the patient subgroup analysed prospectively, the decrease and normalisation of LOS pressure was maintained in the long term. These results are comparable with those obtained in the open approach long term and also provide evidence for future emerging techniques such as transluminal endoscopic myotomy.
Although it has been shown in a randomised clinical trial that anti-reflux procedures decreased the incidence of GORD after myotomy,14 controversy exists regarding which is the most appropriate. In this study a Dor anterior fundoplication was systematically performed because it provides a good barrier against acid without altering drainage of the oesophagus because it avoids posterior gastroesophageal dissection. In a recent meta-analysis15 GORD incidence measured with a pHmetry for laparoscopic myotomies was between 9% and 33% depending on the series. Studies with a longer follow-up of achalasia in the open approach studies show that one of the reasons for the patients’ clinical impairment was the incidence of GORD long term. Ortiz et al. report a rate of 23% and Csendes et al. of 28% in long term follow-up.4,5 Although the overall GORD rate in this study was 10%, in the patient group with a follow-up of over 10 years, the rate was 22%.
There were 2 limitations to this study. One was the impossibility of following up all the patients who underwent surgery. It was a great challenge to convince patients to take part in functional controls owing to the great improvement in clinical symptoms and quality of life achieved. The second limitation was that patients were analysed retrospectively. Although the classification in 3 groups according to follow-up time might cause a bias, pre and post operative assessment, the surgical team and technique used were the same for all patients. However, we could prospectively control the same group of patients on 2 occasions after surgery, one of them after more than 10 years.
To conclude, this study shows that laparoscopic approach for achalasia improves patients¿ clinical symptoms and quality of life, normalising LOS pressure to an acceptable GORD rate, even with a follow-up of over 10 years.
Conflict of InterestsThe authors declare no financial aid was received for this research study and have no conflict of interests to declare.
Please cite this article as: Marinello FG, Targarona EM, Balague C, Poca M, Mones J, Trias M. Abordaje laparoscópico de la acalasia. Resultados clínicos, de calidad de vida y funcionales a largo plazo. Cir Esp. 2014;92:188–194.