Laparoscopic cholecystectomy is a common procedure in general surgery, and in complex cases it is important for the surgeon to know all the alternatives with low associated morbidity. Laparoscopic subtotal cholecystectomy should be considered as an option when a critical view of safety cannot be obtained, because it has a low complication rate and gives the advantages of minimally invasive surgery.
MethodsRetrospective study of laparoscopic subtotal cholecystectomies in an eight years period.
ResultsA total of 1059 laparoscopic cholecystectomies were performed; 22 were subtotal cholecystectomies, without conversion. Biliary fistula (9%) and intraabdominal collections (4.5%) were the most common complications described. No iatrogenic bile duct injuries or deaths were reported. Our follow-up period was 32 months, no recurrences were reported.
ConclusionsLaparoscopic subtotal cholecystectomy is a safe and effective procedure. It should be considered as an option in complex cases.
La colecistectomía laparoscópica es uno de los procedimientos quirúrgicos realizados con más frecuencia a nivel mundial en el campo de la cirugía general, por lo que es fundamental que el cirujano conozca las diferentes alternativas al momento de enfrentarse con un caso complejo. Bajo esta premisa, es importante considerar la colecistectomía laparoscópica subtotal como una opción, cuando después de una adecuada disección, no se logra identificar las estructuras anatómicas y no se obtiene la visión crítica de seguridad. Este procedimiento cursa con baja morbilidad y con las ventajas ampliamente conocidas de la cirugía mínimamente invasiva.
MétodosEstudio retrospectivo de pacientes a quienes se les realizó colecistectomía laparoscópica subtotal en un periodo de 8 años.
ResultadosSe realizaron 1.059 colecistectomías laparoscópicas. De estas, 22 correspondieron a colecistectomías subtotales. No se registraron lesiones de vía biliar ni conversiones. Las complicaciones más frecuentes fueron la fístula biliar (9%) y la colección intraabdominal (4,5%). No hubo mortalidad asociada al procedimiento. Durante un periodo de seguimiento promedio de 32 meses, no se observó recurrencia de sintomatología.
ConclusionesLa colecistectomía laparoscópica subtotal es un procedimiento efectivo, seguro y reproducible. Debe ser considerada como una opción en casos complejos.
Since the introduction of laparoscopic cholecystectomy in the field of general surgery and our understanding of the many advantages it offers, this approach has quickly established itself as the treatment of choice in patients with cholelithiasis, as it is considered an effective procedure and with low morbidity and mortality rates.1–4
During laparoscopic cholecystectomy, surgeons are often faced with complex situations, such as Mirizzi's syndrome, severe cholecystitis and liver cirrhosis, where anatomical structures cannot be properly identified and the critical view of safety cannot be achieved. This leads to greater surgical risk and the possibility of bile duct injury.5–7 In these cases, the following options have been proposed: conversion of the procedure, cholecystostomy or subtotal laparoscopic cholecystectomy.8,9
Conversion to open surgery resolves the problem in a single operation. However, it does not guarantee adequate identification of anatomical structures, and therefore does not eliminate the risk of injury to the bile duct. Furthermore, with conversion, the advantages of laparoscopic surgery are lost. Cholecystostomy can be done laparoscopically, but the problem is not resolved in a single operation, so the patient must undergo another surgical procedure. On the other hand, laparoscopic subtotal cholecystectomy not only provides the advantage of maintaining the benefits of minimally invasive surgery, but it also resolves the problem in a single procedure, making this technique an ideal tool in complex cases.8,9
This procedure has been previously described as a safe alternative in cases of complex cholecystectomies, where the critical view of safety cannot be achieved.8–22
In this study, we report the experience of our department with this procedure.
MethodsThis is a retrospective study that included patients with indications for laparoscopic cholecystectomy but who underwent laparoscopic subtotal cholecystectomy because of intraoperative findings over a period of 8 years in the Surgery Service III at the Caracas University Hospital. Excluded from the study were those patients whose initial approach was by laparotomy and who underwent an additional surgical procedure during the same operation.
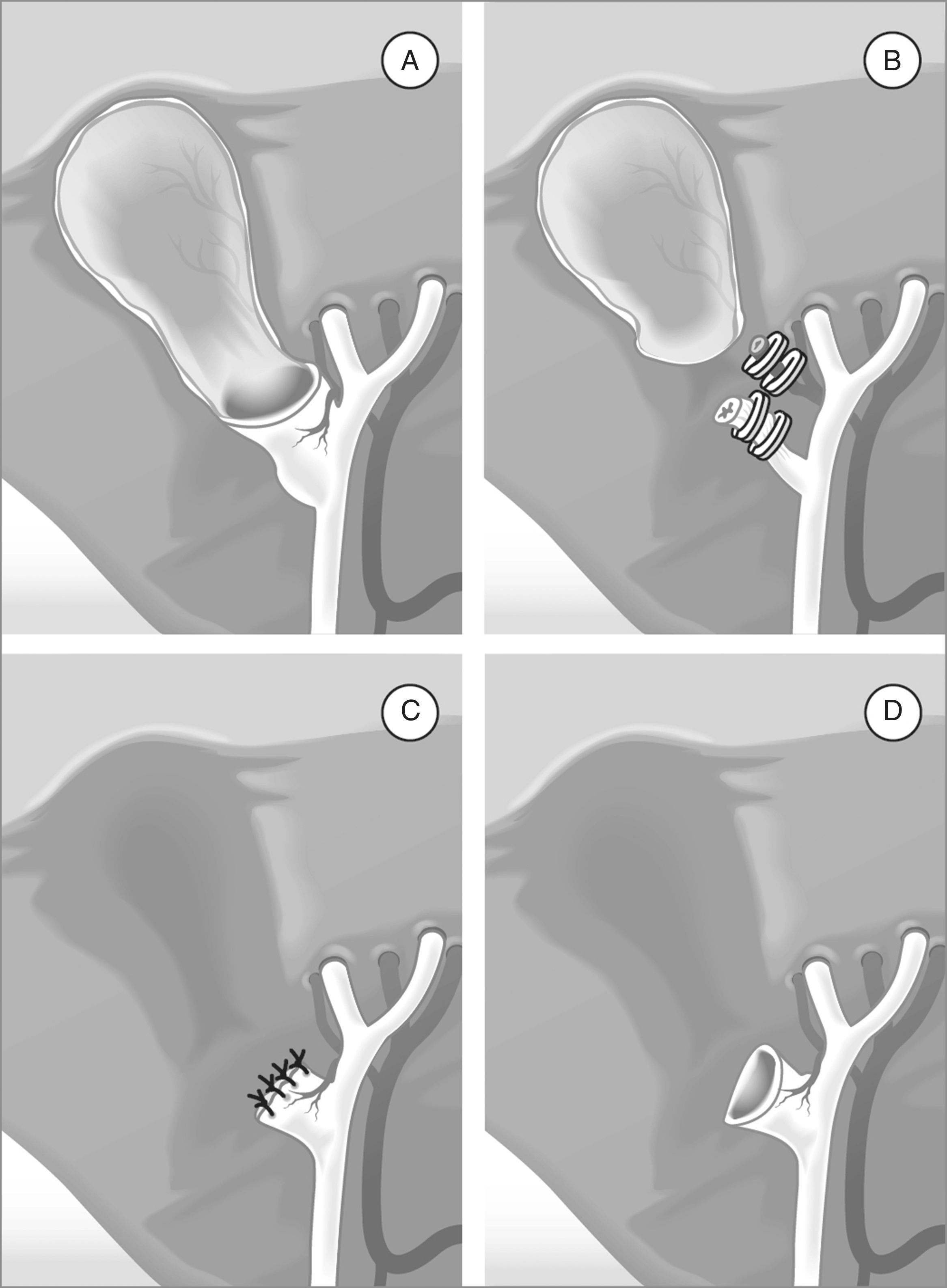
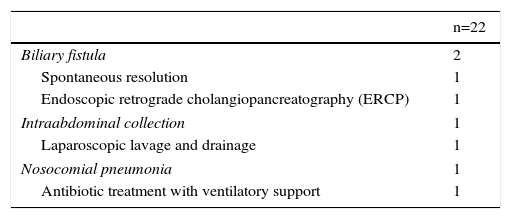
Subtotal cholecystectomy consists of the removal of most of the organ, usually with dissection at the infundibulum.10 According to the classification by Henneman et al., there are four types depending on the preservation of the posterior wall, the area of the dissection and the management of the remaining structures. Type A is based on preserving the posterior wall, which would be attached to the gallbladder bed, without closing the gallbladder remnant; type B involves preserving the posterior wall by closing the gallbladder remnant; type C involves making the dissection at the infundibulum of the gallbladder, with closure of the gallbladder remnant; similarly, in type D, the division is made at the area of the infundibulum of the gallbladder, although it is not closed8 (Fig. 1).
Types of subtotal cholecystectomy: (A) preservation of the posterior wall of the gallbladder with open remnant; (B) preservation of the posterior wall of the gallbladder with closed remnant; (C) closure of the gallbladder remnant without preservation of the posterior wall; (D) open gallbladder remnant without preservation of the posterior wall.
Description of the technique: The patient is placed in a supine position, with the laparoscopic tower located towards the right shoulder. The surgeon and the camera assistant stand on the left side, and the assistant on the right side. Pneumoperitoneum is created following the technique chosen by the surgeon, and trocars are placed. The trocar in the umbilical region is occupied by the camera; the second trocar is placed in the epigastrium; the third trocar along the mid-clavicular line approximately 2cm below the ribcage. These latter two trocars are used by the head surgeon, while the last trocar, placed along the anterior axillary line below the ribcage, is for the assistant. However, it is necessary to mention that these latter two can vary according to the criteria of the surgeon after defining the location of the gallbladder.
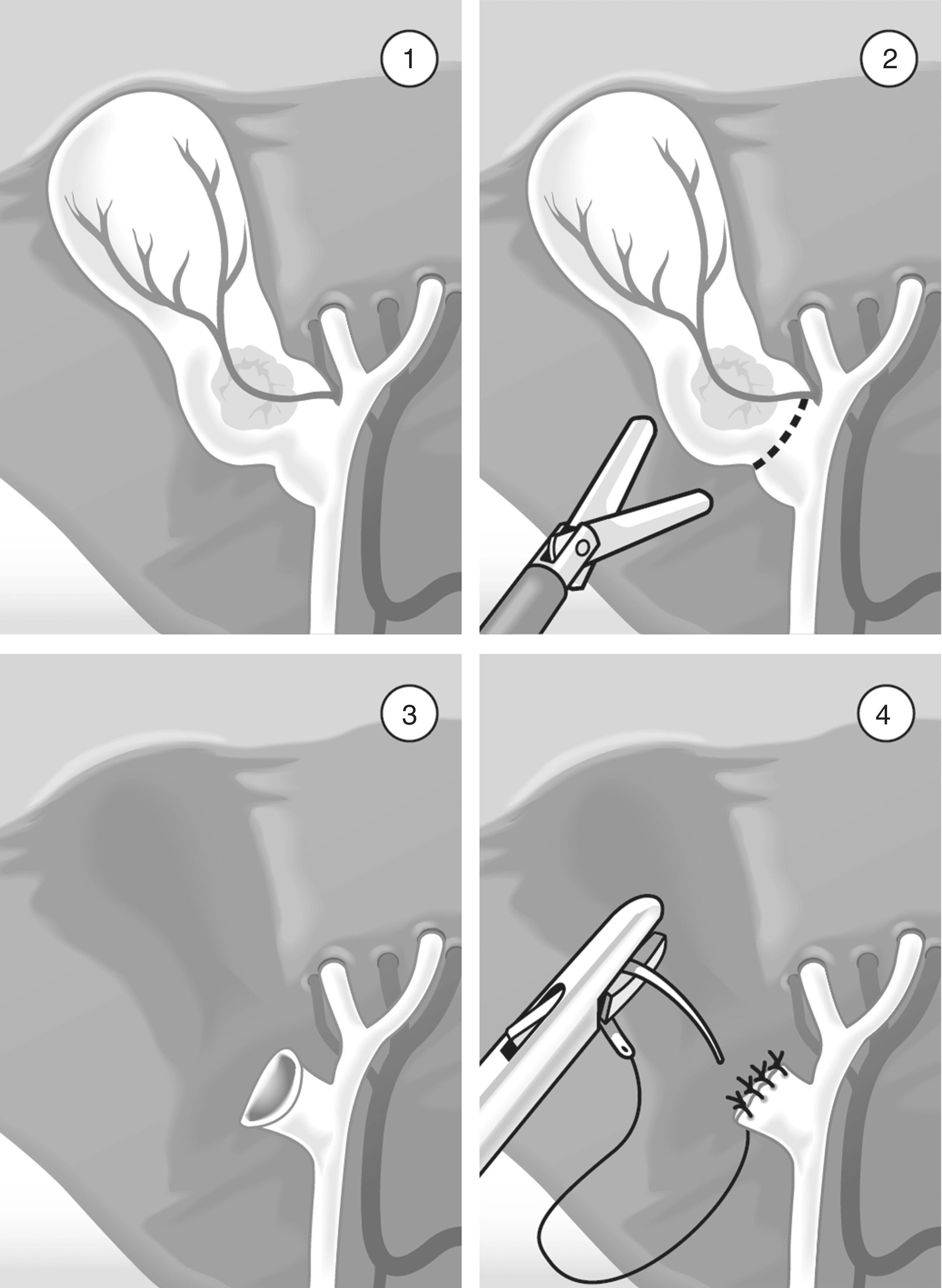
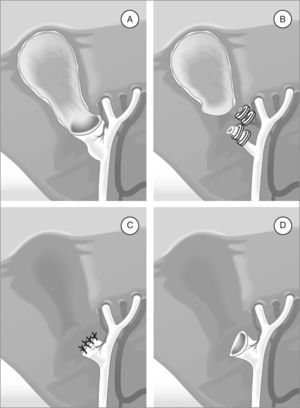
The procedure begins with the traction of the bottom of the gallbladder in the cranial direction towards the right shoulder of the patient to expose the infundibulum and initiate the dissection and identification of the structures of the cystohepatic triangle. The infundibulum of the gallbladder is identified and lateral traction is performed; afterwards, the peritoneum is dissected on the anterior and posterior sides of the gallbladder, with release of the infundibulum from the gallbladder bed; with this maneuver, more lateral traction is achieved, which is essential to achieve the critical view of safety. If critical view is not possible, division is carried out at the infundibulum with monopolar or ultrasonic energy (depending on availability). The absence of gallstones in the gallbladder remnant is confirmed under direct vision, then closed by interrupted sutures with 2-0 polyglactin 910, and subsequently the placement of a subhepatic drain tube is used systematically (Fig. 2).
Surgical technique of laparoscopic subtotal cholecystectomy: (1) there is no critical vision after adequate dissection; (2) dissection at the infundibulum; (3) identification of remaining calculi under direct vision, followed by extraction; (4) closure of the infundibulum with suture and extracorporeal knot-tying.
All perioperative, morbidity and follow-up data were registered in a database on Filemaker PRO (FileMaker Inc.), where they were obtained for tabulation in Excel.
The statistical analysis was performed with the StatCalc program (AcaStat Software Inc.) and based on descriptive statistics, using measures of central tendency for the quantitative variables and proportions for the qualitative variables.
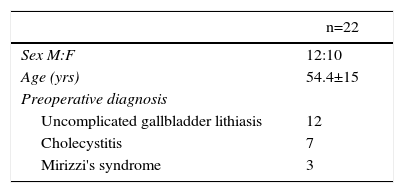
ResultsIn an 8-year study period (2008–2016), a total of 1059 laparoscopic cholecystectomies were performed, 22 (2%) of which were subtotal. The patients who underwent subtotal laparoscopic cholecystectomy were mostly male, ranging in age from 16 to 87. Regarding the type of intervention, 14 patients (64%) underwent elective surgery and eight patients (36%) required emergency interventions (Table 1).
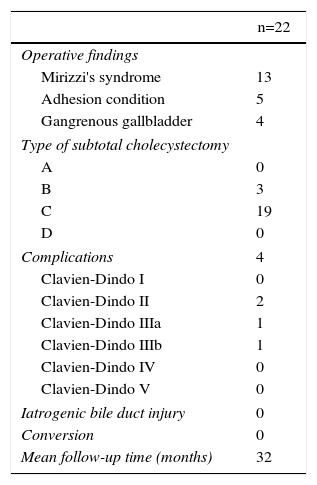
Operative findings that led to the decision to perform subtotal cholecystectomy included: Mirizzi's syndrome in 13 patients (59%), a severe adhesion condition in five patients (23%), which made it difficult to dissect the cystohepatic triangle, and obstructed and gangrenous gallbladder in four patients (18%), which made it difficult to identify anatomical structures (Table 2).
Details of the Surgery.
| n=22 | |
|---|---|
| Operative findings | |
| Mirizzi's syndrome | 13 |
| Adhesion condition | 5 |
| Gangrenous gallbladder | 4 |
| Type of subtotal cholecystectomy | |
| A | 0 |
| B | 3 |
| C | 19 |
| D | 0 |
| Complications | 4 |
| Clavien-Dindo I | 0 |
| Clavien-Dindo II | 2 |
| Clavien-Dindo IIIa | 1 |
| Clavien-Dindo IIIb | 1 |
| Clavien-Dindo IV | 0 |
| Clavien-Dindo V | 0 |
| Iatrogenic bile duct injury | 0 |
| Conversion | 0 |
| Mean follow-up time (months) | 32 |
According to the classification by Henneman et al.,8 the types performed were type C in 86% of cases (19 patients) and less frequently type B (14%); no type A or D subtotal cholecystectomies were performed. The material used for the closure of the gallbladder was 2-0 polyglactin 910 suture in 95% of cases. None of the patients required conversion.
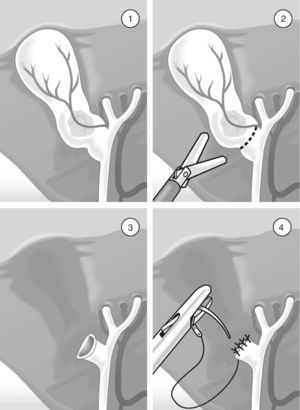
As for the postoperative complications, the most common was biliary fistula, which was present in two patients (9%) and low discharge, requiring endoscopic retrograde cholangiopancreatography with sphincterotomy in one of the patients due to persistence of the fistula. Another complication observed was intra-abdominal collection, which presented in one patient (4.5%), requiring laparoscopic lavage and drainage (Table 3). No bile duct injury was present. Within the general complications, nosocomial pneumonia was detected in one of the cases, which evolved satisfactorily with medical treatment and no ventilatory support.
Postoperative Complications and Additional Procedures.
| n=22 | |
|---|---|
| Biliary fistula | 2 |
| Spontaneous resolution | 1 |
| Endoscopic retrograde cholangiopancreatography (ERCP) | 1 |
| Intraabdominal collection | 1 |
| Laparoscopic lavage and drainage | 1 |
| Nosocomial pneumonia | 1 |
| Antibiotic treatment with ventilatory support | 1 |
During the mean follow-up of 32 months, there was no evidence of recurring symptoms.
DiscussionLaparoscopic cholecystectomy is the treatment of choice for gallstones. However, in complex cases with fibrosis, inflammation and hindered critical view of safety, subtotal laparoscopic cholecystectomy is a minimally invasive, effective option with low morbidity.
Subtotal cholecystectomy is not a new procedure. It was initially described for the one-step approach of patients with severe inflammatory processes, thereby omitting cholecystostomy as a necessary prior stage.10–12 Currently, subtotal laparoscopic cholecystectomy is considered a rescue procedure with low morbidity and mortality that provides effective, safe resolution of complex cases, while retaining the advantages of minimally invasive surgery.8–18
Recent studies with high levels of evidence8,9 demonstrate that laparoscopic subtotal cholecystectomy is an effective and safe technique. In 2013, Henneman et al.8 reported that it is feasible in 90% of patients, as 10% require conversion due to inflammation, adhesions, fibrosis and vascular lesions, which make the procedure difficult. In our study, none of the patients required conversion, and the laparoscopic approach provided satisfactory resolution.
The reports by Henneman et al.8 and Elshaer et al.9 show evidence that the preoperative diagnosis that most frequently required subtotal cholecystectomy was acute cholecystitis, due to firm adhesions and inflammation that made it difficult to dissect and correctly identify the structure. In this same paper, Mirizzi syndrome was observed in 8% of cases. In our study, several patients initially presented episodes of previous cholecystitis without a timely surgical resolution, which may have led to the inflammation in the area of the cystohepatic triangle, causing adhesions and fibrosis that made the procedure difficult to perform. On the other hand, many patients in our study were elderly males, a factor that could delay or diminish symptoms and hide an inflammatory or infectious process, later resulting in a difficult cholecystectomy.
As for the type of subtotal cholecystectomy performed, no differences were observed in patient progress if the gallbladder stump was left open or closed according to the different studies.8,9 However, in our department, we prefer closing the stump and only leave it open in those cases in which the fibrosis impedes closure.
With regard to complications inherent to the procedure, the most frequent are biliary fistula and intra-abdominal collections (biloma). The frequency of biliary fistulae recorded in the literature is 10%–18%.8,9 In our study, 9% of patients presented a low-flow fistula, an only one patient required endoscopic retrograde cholangiopancreatography with sphincterotomy due to persistence of the fistula, showing satisfactory progression. Biloma was presented by 4.5% of our patients (similar to reports in the literature8), and biloma was the most frequent cause of reoperation observed in this study. This could be explained by the edema of the gallbladder wall, which stops once the inflammatory process has been resolved, causing the sutures to lose tension and leak bile. On the other hand, manipulation of the infundibulum during the procedure could facilitate the migration of a calculus towards the bile duct, causing increased pressure and consequent filtration. Therefore, when opening the infundibulum, it is vitally important to identify and extract the observed stones, reason why we insist on the need to always insert an active subhepatic drain.
It is important to mention that the recurrence of the symptoms due to the presence of the infundibulum is very low, reported at about 2% in the study by Henneman et al.8 In the present study, no cases of symptomatic recurrence were reported in an average follow-up period of 32 months.
Likewise, we should emphasize that we are not proposing laparoscopic subtotal cholecystectomy as a replacement procedure for total cholecystectomy. Instead, it should be used as a rescue procedure when the risks of total cholecystectomy surpass possible benefits, for instance in complex cases in which the identification of anatomical structures and critical view of safety cannot be achieved and there is a high risk of bile duct injury.
In short, laparoscopic subtotal cholecystectomy has proven to be a safe and effective technique that retains the advantages of laparoscopic surgery, with a low number of complications. The long-term patient evolution has demonstrated that it is not always necessary to complete the cholecystectomy, and the subtotal approach is a procedure that resolves the problem in a single operation.
AuthorsG.J.: data collection, analysis and interpretation of the results, article composition.
J.R.: study design, data collection.
W.B.: study design, data collection.
L.V.: data collection.
O.R.: study design, analysis and interpretation of the results, critical review and approval of the final version.
R.S.: analysis and interpretation of the results, critical review and approval of the final version.
A.S.: analysis and interpretation of the results, article composition, critical review and approval of the final version.
Conflict of InterestThe authors have no conflict of interests to declare.
Please cite this article as: Jara G, Rosciano J, Barrios W, Vegas L, Rodríguez O, Sánchez R, et al. Colecistectomía laparoscópica subtotal como alternativa quirúrgica segura en casos complejos. Cir Esp. 2017;95:465–470.