Surgical units attending sarcomas in Spain are poor studied. The aim is to know the management of this pathology to identify areas of improvement through multicenter study based on a voluntary survey.
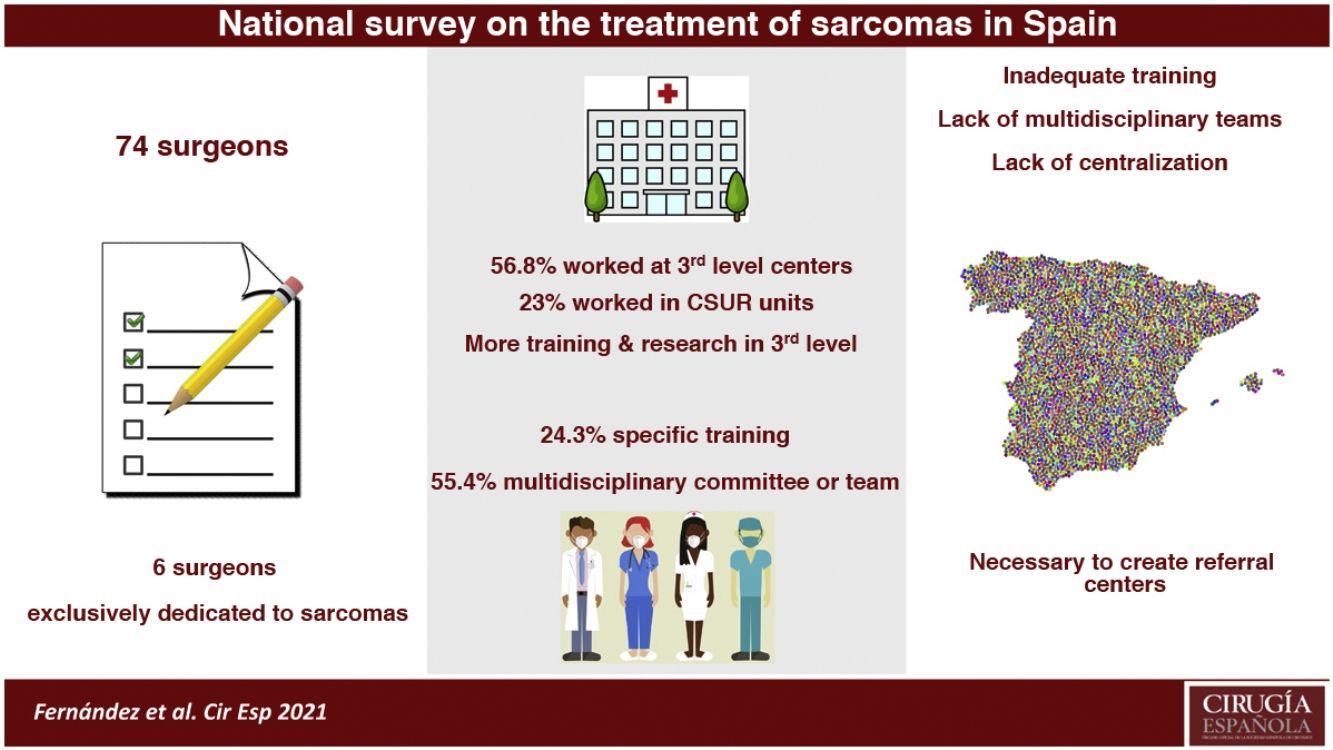
The survey was completed by 74 surgeons of different hospitals, which 32,4% is exclusively dedicated to sarcomas. Only 24.3% declared to receive specific training in sarcomas. The most frequent type of hospital was the third level (56.8%), where 38,1% of the surgeons belong to societies or working-groups in sarcoma fields vs. 9,4% in first-second levels. The number of surgeons with specific theoretical training and papers published in this field are higher in third level hospitals. 55,4% belonged to a multidisciplinary unit. A multidisciplinary team was available in 57% of third level hospital vs 28% in others.
Most services in charge of this patients are characterized by deficient specialization, low workload and the absence of a multidisciplinary team.
Las Unidades encargadas de los sarcomas en España están poco estudiadas. El objetivo es conocer el manejo de esta patología para identificar áreas de mejora mediante un estudio multicéntrico basado en una encuesta voluntaria.
La encuesta fue completada por 74 cirujanos de centros diferentes. El 32,4% se dedica exclusivamente a los sarcomas. Solo el 24,3% ha recibido formación específica. El hospital más frecuente fue el tercer nivel (56,8%), donde el 38,1% de los cirujanos pertenecen a sociedades/grupos de trabajo específicos vs. 9,4% en segundo-primer nivel. El número de cirujanos con formación teórica específica y artículos publicados en este campo es mayor en los de tercer nivel. El 55,4% pertenece a una unidad multidisciplinar. Los equipos multidisciplinares están disponibles en el 57% de los hospitales terciarios vs.28% en los demás.
La mayoría de los servicios que atienden esta patología presentan escasa especialización, baja carga de trabajo y carecen de equipos multidisciplinares.
Sarcomas are a very heterogeneous group of tumors, with more than 150 histological types and subtypes, which can develop anywhere in the anatomy. Half are found in the extremities and one-third in the abdomen, pelvis and retroperitoneum1. This histological and anatomical diversity greatly limits the acquisition of sufficient experience to properly manage these patients. Each of them has a very different prognosis and treatment1–5. These are tumors that account for 1% of all cancers but are responsible for 2% of global mortality2,6.
In recent years, organizations like the European CanCer Organization (ECCO) have indicated the need to improve the care of patients with sarcoma by drawing up a list of minimum requirements for their management7. Likewise, in 2017 the European Parliament, through the Sarcoma Policy Checklist2,8, created a list of priority areas on which politicians should act to improve the management of sarcoma. In general, they insist on the need to centralize the diagnosis and treatment of these patients in referral centers (RC) that treat a high volume of cases and have multidisciplinary teams (MDT) of specialists and surgeons specially trained for their management. Centralization through the creation of national referral networks is considered critical to obtain good results2,8.
In Spain, the Ministry of Health has certified 7 national referral centers (Referral Centers, Units and Services [CSUR, its acronym in Spanish]) to date for the management of sarcomas2,8. However, there are still measures that need to be implemented to guarantee excellent treatment in the national territory.
The objective of this study is to better understand the management of sarcomas in our country based on a national survey, particularly to determine the resources, capacities and limitations that exist in the surgical services that manage these patients. Lastly, based on the information obtained, we will develop a series of recommendations to improve the performance of surgeons, which will benefit these patients.
MethodsWe conducted a cross-sectional, multicenter, observational study developed by the Mesenchymal Tumors-Sarcomas Working Group of the Spanish Association of Surgeons (AEC) based on the completion of a survey. The survey, which was voluntary and anonymous, was completed during the months of May to July 2020 on the AEC website at http://www.survio.com/survey/d/abordaje-multidisciplinar-sarcomas, supported and maintained by Im3dia Comunicación®.
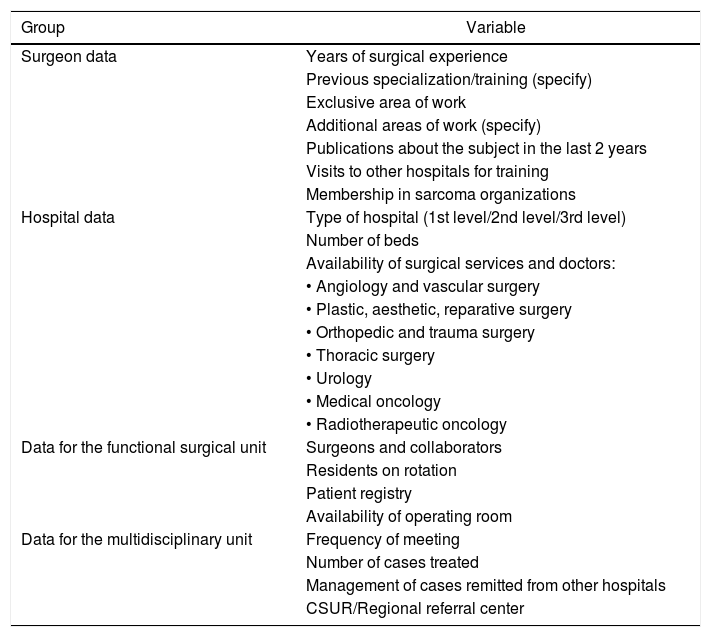
All members of the AEC were invited to participate. Only one response per hospital was collected, and incomplete surveys were invalidated by the program. The survey is divided into 4 groups of questions for a total of 18 variables (Table 1): general surgeon data; hospital data; data about the surgical unit managing these patients; and data from the hospital multidisciplinary unit where the patients are assessed. The questions included in the survey were prepared following the recommendations set out in Table 2.
Variables analyzed by the survey, grouped by characteristics.
| Group | Variable |
|---|---|
| Surgeon data | Years of surgical experience |
| Previous specialization/training (specify) | |
| Exclusive area of work | |
| Additional areas of work (specify) | |
| Publications about the subject in the last 2 years | |
| Visits to other hospitals for training | |
| Membership in sarcoma organizations | |
| Hospital data | Type of hospital (1st level/2nd level/3rd level) |
| Number of beds | |
| Availability of surgical services and doctors: | |
| • Angiology and vascular surgery | |
| • Plastic, aesthetic, reparative surgery | |
| • Orthopedic and trauma surgery | |
| • Thoracic surgery | |
| • Urology | |
| • Medical oncology | |
| • Radiotherapeutic oncology | |
| Data for the functional surgical unit | Surgeons and collaborators |
| Residents on rotation | |
| Patient registry | |
| Availability of operating room | |
| Data for the multidisciplinary unit | Frequency of meeting |
| Number of cases treated | |
| Management of cases remitted from other hospitals | |
| CSUR/Regional referral center |
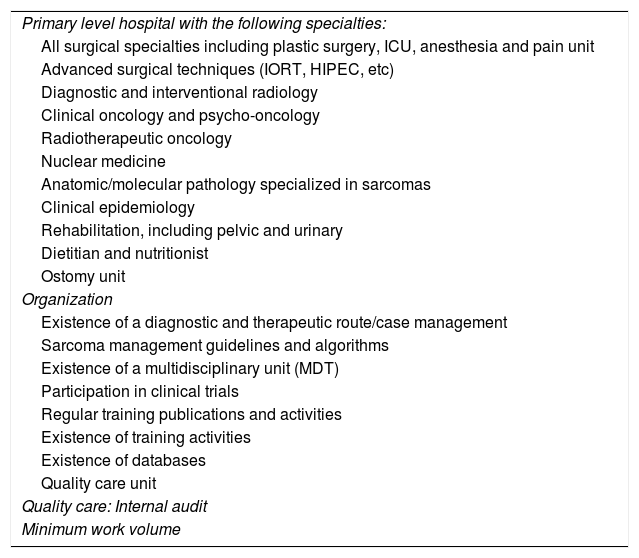
Characteristics of a sarcoma referral center according to La Società Italiana di Chirurgia Oncologica (SICO)10.
| Primary level hospital with the following specialties: |
| All surgical specialties including plastic surgery, ICU, anesthesia and pain unit |
| Advanced surgical techniques (IORT, HIPEC, etc) |
| Diagnostic and interventional radiology |
| Clinical oncology and psycho-oncology |
| Radiotherapeutic oncology |
| Nuclear medicine |
| Anatomic/molecular pathology specialized in sarcomas |
| Clinical epidemiology |
| Rehabilitation, including pelvic and urinary |
| Dietitian and nutritionist |
| Ostomy unit |
| Organization |
| Existence of a diagnostic and therapeutic route/case management |
| Sarcoma management guidelines and algorithms |
| Existence of a multidisciplinary unit (MDT) |
| Participation in clinical trials |
| Regular training publications and activities |
| Existence of training activities |
| Existence of databases |
| Quality care unit |
| Quality care: Internal audit |
| Minimum work volume |
HIPEC: Hyperthermic intraperitoneal chemotherapy; IORT: intraoperative radiotherapy.
We performed a descriptive and analytical study of the data obtained (means and percentage of the total) as well as a comparison of all the variables between the tertiary level hospitals and primary-secondary care centers using the chi-squared test for qualitative variables. After applying the Kolmogorov-Smirnov test to analyze the normality of the quantitative variables, the Student’s t-test was used for normal variables and the Mann-Whitney test for non-normal variables. P < .05 was considered statistically significant. The statistical study was carried out with the SPSS v.24.0 program for Windows (SPSS, Inc, Chicago, IL, USA).
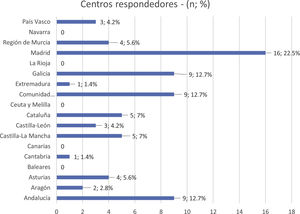
ResultsOverviewThe survey was completed in its entirety by 74 surgeons, so these 74 surveys comprise the basis for these results, each of which is from a different hospital. Online completion of the survey took an average time of 2−5 min in 65% of survey participants. The autonomous community with the highest participation was Madrid (16 surveys [22.5%]), followed by Andalusia, Valencia and Galicia, each of them with 9 surveys (12.7%) (Table 3).
Surgeon characteristicsSurgeons who completed the survey mostly had ≥20 years of experience (40 cases [54%]), followed by those with ≥10 and <20 years of experience (19 cases [26%]) and those with <10 years of experience (15 cases [20%]). Only 24.3% (18 cases) of the surgeons stated that they had undergone any specific training for the management of these tumors: in 17 cases (23%) of a theoretical nature, of a practical nature in only one case, and with training stays at specialized centers in only 3 cases (4%). Only 8.1% (6 cases) of the surgeons stated that they were dedicated exclusively to the management of sarcomas, while the vast majority (91.9%) stated that they combined this activity with another type of surgery: esophagogastric (25%), hepatobiliary-pancreatic (23%), coloproctological (23%) and oncological/carcinomatosis (15%). Only 16% of the surgeons stated that they had published scientific articles in the field of sarcomas, and only 25.7% stated that they belonged to a related society or organization.
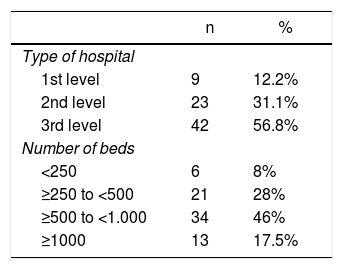
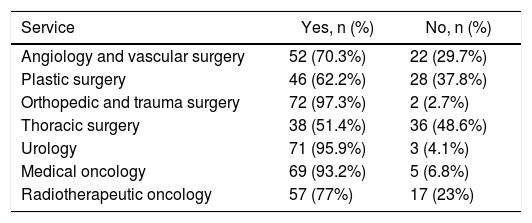
Hospital characteristicsThe main characteristics of the hospitals of the surgeons who completed the survey are listed in Table 4. The most frequent type of hospital was the tertiary care level (42 hospitals [56.8%]), followed by the secondary care (23 hospitals [31.1%]) and primary (9 hospitals [12.2%]). In 46% of the cases (34 hospitals), the centers had ≥500 and <1000 beds, followed by hospitals with a number of beds ranging from ≥250 to <500 (21 hospitals [28%]), while a smaller percentage were hospitals with >1000 beds (13 hospitals [17.5%]) and those with <250 beds (6 hospitals [8%]). The availability of medical and surgical services of interest in the management of sarcomas in these hospitals, apart from general surgery, is shown in Table 5, where an availability of less than 90% stands out in the angiology and vascular surgery services (70.3%), plastic surgery (62.2%), thoracic surgery (51.4%) and radiation oncology (77%).
Availability of medical and surgical services of interest in the multidisciplinary approach of sarcomas and mesenchymal tumors.
| Service | Yes, n (%) | No, n (%) |
|---|---|---|
| Angiology and vascular surgery | 52 (70.3%) | 22 (29.7%) |
| Plastic surgery | 46 (62.2%) | 28 (37.8%) |
| Orthopedic and trauma surgery | 72 (97.3%) | 2 (2.7%) |
| Thoracic surgery | 38 (51.4%) | 36 (48.6%) |
| Urology | 71 (95.9%) | 3 (4.1%) |
| Medical oncology | 69 (93.2%) | 5 (6.8%) |
| Radiotherapeutic oncology | 57 (77%) | 17 (23%) |
In only 24 cases (32.4%) did the surgeons declare the existence of a surgical unit in their service dedicated exclusively to the management of sarcomas and mesenchymal tumors, since in the vast majority of cases (50 cases [67.6%]) there was no such unit. In 45.8% of the cases, these units had at least two permanent surgeons, 50% with at least one collaborating surgeon and 62% with a permanent rotating resident doctor. 87.5% of these units maintained a prospective patient registry. Only 45.8% of these units had a permanent operating room, normally one a week.
According to 55.4% of participants, there is a mesenchymal tumors/sarcoma committee at their hospital, which meets once a week in 54% of the cases and 1–2 times a month in the remaining 46% of cases. The activity of these units involves assessing <10 cases per session in 81% of cases. Only 9% of these units evaluate ≥10 cases per session. Of the cases evaluated, only 21.2% were ≥5 new cases evaluated per session. These hospital units are referral units for other hospitals in 72.7% of cases, although 90.9% of the cases assess patients from other hospitals even without being their referral units. Only 23% of the cases were CSUR units, while 50% of the units were regional RC, although not CSUR.
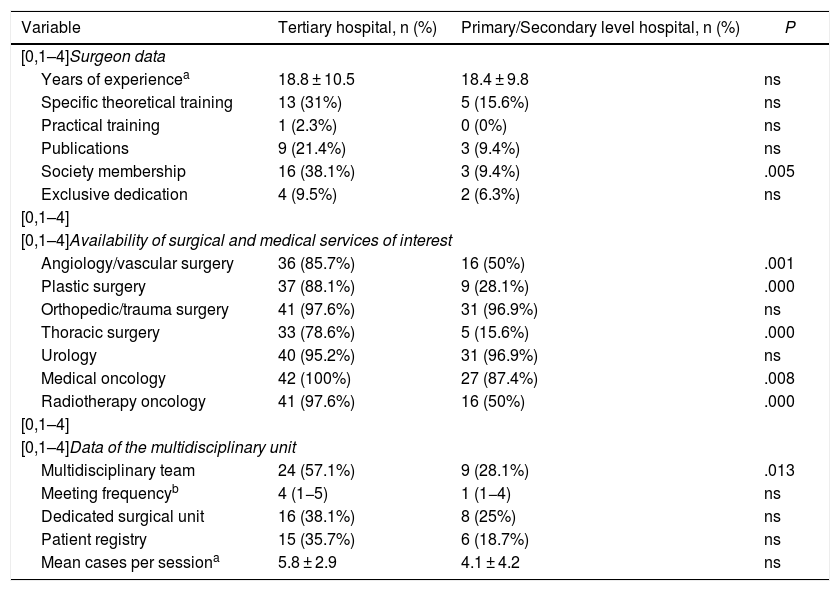
Comparison between tertiary vs primary/secondary care hospitalsWhen we compared tertiary hospitals with primary/secondary care centers (Table 6), there were no statistically significant differences in the years of experience of the surgeons, their exclusive dedication, or the completion of training courses. It is relevant that tertiary hospitals have twice as many surgeons who have received specific theoretical training and have published research articles on the subject compared to primary/secondary hospitals (31% vs 15%, and 21.4% vs 9.4%, respectively), although this was not statistically significant. Membership in societies or working groups in the field of sarcomas was 38.1% in tertiary hospitals vs 9.4% in the primary/secondary centers (P = .005). The availability of medical or surgical services of interest in the management of sarcomas was significantly higher (P < .05) in tertiary care hospitals compared to primary/secondary centers, specifically the presence of angiology/cardiovascular surgery, plastic surgery, thoracic surgery, medical oncology and radiation oncology departments. No differences were observed regarding the availability of a urology or orthopedic and trauma surgery department. The availability of an MDT was reported in 57% of tertiary hospitals vs 28% (P = .013) in primary/secondary care hospitals. The frequency of this team’s meetings and the number of cases assessed per session was much higher in tertiary level hospitals (4 vs 1 and 5.8 vs 4.1, respectively), although without statistical significance. We also observed the presence of a patient registry in 35.7% of tertiary hospitals compared to 18.7% in primary/secondary care hospitals, although this was not significant.
Differential characteristics between tertiary and primary/secondary care hospitals.
| Variable | Tertiary hospital, n (%) | Primary/Secondary level hospital, n (%) | P |
|---|---|---|---|
| [0,1–4]Surgeon data | |||
| Years of experiencea | 18.8 ± 10.5 | 18.4 ± 9.8 | ns |
| Specific theoretical training | 13 (31%) | 5 (15.6%) | ns |
| Practical training | 1 (2.3%) | 0 (0%) | ns |
| Publications | 9 (21.4%) | 3 (9.4%) | ns |
| Society membership | 16 (38.1%) | 3 (9.4%) | .005 |
| Exclusive dedication | 4 (9.5%) | 2 (6.3%) | ns |
| [0,1–4] | |||
| [0,1–4]Availability of surgical and medical services of interest | |||
| Angiology/vascular surgery | 36 (85.7%) | 16 (50%) | .001 |
| Plastic surgery | 37 (88.1%) | 9 (28.1%) | .000 |
| Orthopedic/trauma surgery | 41 (97.6%) | 31 (96.9%) | ns |
| Thoracic surgery | 33 (78.6%) | 5 (15.6%) | .000 |
| Urology | 40 (95.2%) | 31 (96.9%) | ns |
| Medical oncology | 42 (100%) | 27 (87.4%) | .008 |
| Radiotherapy oncology | 41 (97.6%) | 16 (50%) | .000 |
| [0,1–4] | |||
| [0,1–4]Data of the multidisciplinary unit | |||
| Multidisciplinary team | 24 (57.1%) | 9 (28.1%) | .013 |
| Meeting frequencyb | 4 (1−5) | 1 (1−4) | ns |
| Dedicated surgical unit | 16 (38.1%) | 8 (25%) | ns |
| Patient registry | 15 (35.7%) | 6 (18.7%) | ns |
| Mean cases per sessiona | 5.8 ± 2.9 | 4.1 ± 4.2 | ns |
The results of this survey show that the surgical management of sarcomas in Spain presents important deficiencies. Its management is not centralized, and more than 40% of these patients are treated in primary/secondary care hospitals that are not specially dedicated to this pathology, which treat few cases and usually do not have an MDT. In addition, the surgeons who handle these cases lack adequate training and experience. This situation is very negative and coincides with that of other countries in our setting2,8.
The great histological and anatomical heterogeneity of these tumors1 explains why it is very difficult for health professionals to acquire adequate specialized training, which results in late and/or erroneous diagnoses. Moreover, the treatments applied do not always follow the existing guideline recommendations (which happens one-third of cases) and only half of the patients are adequately treated surgically2,8. Patient access to specialized care is very limited, and current research deficiencies make it difficult to access specific treatments for each type of sarcoma2,8–10.
Internationally, important efforts have been made to improve this situation2. Thus, the ECCO7 published a list of essential requirements for sarcoma management, the Sarcoma Patient EuroNet (SPAEN) developed a series of patient-guided recommendations for sarcoma care11, and the European Reference Network (ERN) on Rare Adult Cancers (EURACAN) has also been created, with a specific domain for sarcoma5. In February 2017, the Sarcoma Policy Checklist document was published, which attempted to answer the question: What is most needed to improve sarcoma care? The authors identified 5 key actions: creation of accredited RC in each country; further professional training for healthcare professionals involved in the treatment of sarcoma; patient management should be multidisciplinary; greater incentives for research and innovation; together with faster access to more effective treatments8,12. In short, these patients should be treated in RC with a high volume of cases, normally in tertiary level hospitals, and managed in the framework of an MDT. In Spain, the Sarcoma Action Plan 2019−202013, prepared jointly by the Spanish Sarcoma Research Group (Grupo Español de Investigación en Sarcomas, or GEIS), the Spanish Association of Patients with Sarcoma (Asociación Española de Afectados por Sarcomas, or AEAS) and the Mari Paz Jiménez Casado Foundation (FMPJC) have identified three priorities to reduce erroneous diagnoses and incorrect treatments: a) creation of RC with sufficient resources and expert specialists, in addition to the establishment of protocols and action protocols for the Primary Care setting; b) implementation of a rapid referral circuit and appropriate treatment protocol; and c) development of a network of expert pathologists to improve the diagnostic quality of sarcomas.
The need to designate RC is related with the difficulty to acquire sufficient experience in a rare pathology, and the centralization of patients in high-volume centers has been shown to improve the quality of their care14,15. In Spain, the GEIS demonstrated the benefit provided by RC, showing greater recurrence-free and overall survival, even in patients affected by metastatic sarcomas16,17. Based on the experience of RareCareNet, the Italian Society of Oncological Surgery (SICO)10 provides a list of characteristics that all centers must meet to be considered specialized or having ‘expertise’ (Table 2). Logically, these centers must undergo a process, not only of accreditation but also of continuous evaluation, to guarantee the continuity of quality care1,2,8. To date, the Spanish Ministry of Health has approved 7 RC for sarcoma (CSUR)18, selected based on the existence of MDT with adequate diagnostic and therapeutic routes, with a minimum annual volume of work and an expert pathology department. These RC, in a limited number, must be well coordinated with other non-reference centers but with some experience in the management of these patients, in the form of a network19, allowing patients to be referred and managed in accordance with the strategic decisions of the MDT in charge of the case11,19. The coordination and referral of patients are of great importance and should be managed through an RC case manager, as a delay of >3 months in their referral increases their risk of death by 1.4 fold16,20. Furthermore, a Swedish study21,22 showed that the existence of easy-to-complete patient referral guidelines increased the referral of patients up to 80%23, with a reduction in costs in terms of local recurrence rates, improved surgical results, and general patient outcomes.
A reliable, precise pathology diagnosis is key in patient management2,8; however, the error rate reaches 40%–60% in Europe2,8,24,25. The review of cases by an expert pathologist, as in France with the Sarcoma Pathological Reference Network (RRePS)26,27 or in Spain with the IMPERAS project28, developed by the soft tissue tumor working group of the Spanish Society of Pathological Anatomy (Sociedad Española de Anatomía Patológica, or SEAP), will help improve diagnostic precision and, consequently, therapeutic strategies and final results.
The volume of patients treated per year is considered the most important factor that determines the expertise of an RC29,30. The National Institute for Health and Care Excellence Improving Outcomes Guidance (NICE-IOG)31 establishes an annual minimum of 100 soft tissue sarcomas and 50 bone sarcomas; the ECCO7 suggests a minimum of 100 sarcomas per year, while the Sarcoma Alliance32 establishes the minimum at 50 sarcomas per year (1–2 per week). In 2007, Gutierrez et al.33 considered that a high-volume hospital is one with more than 5–24 surgeries per year. Similarly, the ECCO sets this limit at 30–40 surgeries per year7. In Spain, the designation of CSUR requires an annual case volume of at least 80 patients with soft tissue sarcoma, 10 retroperitoneal and 10–12 bone18. Regardless of the figure adopted, it is clear that the greater the number of cases, the greater the experience, not only in the surgical field but for all the professionals involved30. This greater experience correlates with a clear improvement in the results of retroperitoneal sarcoma surgery: higher R0 rates, lower rehospitalization rates, lower 30- and 90-day mortality, lower rates of local and distant recurrence, better 5-year survival and lower risk of death34,35. The results of our survey reveal that only 45.8% of participants reported having a set weekly operating room, which gives an idea of the volume of surgical work of these groups. As we have seen, this situation is not specific to our environment alone.
One of the most important elements in the management of these patients is their assessment within the MDT2,8,36,37 for better communication and coordination between health professionals, which facilitates agreed-upon, consistent and continuous treatments with greater cost-effectiveness, especially in the more uncommon sarcomas where clinical practice guidelines (CPG) are not available, and greater access to participating in clinical trials9,38. For this reason, the current recommendations16 stress the need for the organization of sarcoma patient care to fall back on the MDT, which is considered an essential criterion when selecting RC. It is estimated that the evaluation of a patient by an MDT can change the treatment in up to 52% of cases39, ensure greater compliance with CPG and be associated with a reduction in local recurrence rates2,8. It is currently recommended that the sarcoma MDT include at least 7 professionals (general surgery, plastic surgery, traumatologist, medical oncologist and radiation therapist, radiologist and pathologist) and that at least 90% of cases be reviewed2,8,9. However, the clinical reality is quite different, and the survey data could not be more discouraging: only 44.6% of hospital have MDT, with very infrequent meetings and a small workload. On the other hand, the existence of databases, typical and characteristic of MDT, is valuable40. Although there is no national sarcoma registry in Spain, various groups and institutions, such as the GEIS or the AEC Sarcoma Working Group itself, have favored their use in several national projects (GEIS 55) that will undoubtedly favor sarcoma research projects.
MDT manage patients on a case-by-case basis in accordance with the CPG developed by different organizations36,37 and are considered crucial in the management of these patients41. It has been shown that CPG compliance is much higher in RC with MDT than in non-expert centers41–44, and adherence and compliance are associated with better results42,45.
To function optimally, the location of RC and their MDT should preferably be established in tertiary care hospitals9,10 since they provide the full range of specialties and technologies necessary for the management of these patients. Despite this, up to 43% of patients are treated in primary/secondary level hospitals, with clear structural and service deficiencies that make it impossible to meet the minimum requirements to treat to these patients.
What is clearly observed in the data of our survey is that the majority of the departments are essentially dedicated to patient treatment. These units do not publish and do not usually belong to sarcoma-related groups or organizations, nor do they have research programs in this field. Thus, many oncologists and surgeons do not receive any formal training on sarcomas as part of their general university education or in their specialized academic training2,8. The few specialized training programs available today are essentially surgical, such as those of the European School of Soft Tissue Sarcoma of the European Society of Surgical Oncology (ESSO)46, or the Italian-French eSurge program47. In this context, surgical research in sarcomas is, logically, very deficient.
Finally, we should mention that the main limitation of this study is that it is based on a voluntary survey and, therefore, does not reflect the national experience in its entirety. This implies the existence of a significant selection bias, as it is very likely that the completion of the surveys by professionals from experienced centers or with greater interest in this pathology has been favored, so the reality that the survey tries to reflect could actually be much worse.
In the management of sarcomas in Spain, there are minimum quality standards that are required but not yet available for most patients. A high percentage of the hospitals where these patients are treated lack specialization in sarcomas. Thus, they do not have an adequate volume of experience, and decisions are made outside the context of an MDT within an RC. The creation of CSUR is an opportunity to establish a network to improve the care of patients with sarcomas in our country. Increased referral to these highly specialized centers and greater collaboration with regional referral centers are of vital importance to guarantee access to the best available treatment for all patients, regardless of their place of residence.
FundingThis article has received no funding.
Conflict of interestsNone.
Coordinator: Vicenç Artigas Raventós, Departamento de Cirugía, Universidad Autónoma de Barcelona, Barcelona. Vicens.artigas@uab.cat
Secretary: Sonia Cantín Blázquez, Hospital Universitario Miguel Servet, Zaragoza.
Members: Juan Ángel Fernández Hernández. Hospital Universitario Virgen de la Arrixaca, Murcia. José Manuel Asencio Pascual, Hospital Universitario Gregorio Marañón, Madrid. Luis Ocaña Wilhemi, Hospital Universitario Virgen de la Victoria, Málaga. Elena García Somacarrera, Hospital Universitario Marqués de Valdecilla, Santander. Gerardo Blanco Fernández, Complejo Hospital Universitario, Badajoz. Francisco Cristóbal Muñoz Casares, Hospital Universitario Virgen del Rocío, Sevilla. Luis Secanella Medayo, Hospital Universitario de Bellvitge, Hospitalet de Llobregat, Barcelona. Evaristo Varo Pérez, Complejo Hospital Universitario, Santiago de Compostela, A Coruña. Juan Francisco Orbis Castellanos, Hospital Universitario La Fe, Valencia. José Antonio González López, Hospital Universitario de la Santa Creu i Sant Pau, Barcelona. Esteban Martín Antona, Hospital Universitario San Carlos, Madrid. Pablo Sanz Pereda, Hospital Universitario Virgen de la Candelaria, Santa Cruz de Tenerife.
The names of the members of the Sarcoma and Mesenchymal Tumor Workgroup of the Spanish Association of Surgeons (AEC) are listed in Appendix A.
Please cite this article as: Fernández JÁ, Pérez BG, Cantín S, Asencio JM, Artigas V. Encuesta nacional sobre el tratamiento de los sarcomas en España. Cir Esp. 2022;100:193–201.