Intraoperative molecular analysis for sentinel lymph node (SLN) metastases using the OSNA (one-step nucleic acid amplification) method has been already validated in breast cancer. The authors compared the cost of OSNA versus the conventional postoperative histopathologic evaluation in patients with breast cancer.
MethodologyPatients with operable breast cancer and clinically and sonographic negative evaluation of the axilla, and who subsequently were operated on between the 15th of October 2008 and the 15th of December 2009 were included in this retrospective cost-benefit analysis. The SLN was assessed by conventional postoperative histological evaluation in Group 1 (45 patients), and by OSNA in Group 2 (35 patients). The following variables were analysed: age, tumour size, histological type, number of SLNs, biopsy result, duration of surgery, days in hospital, postoperative complications, positive lymph nodes in the case of axillary lymphadectomy, cost per patient, hospitalisation cost, and cost per operation.
ResultsThe duration of surgery of the first operation in Group 1 was significantly shorter, but the total time was also higher in this group. The mean hospital stay was longer in Group 1 (P<.001). The mean cost of the hospital stay was higher in Group 1 compared to Group 2 (P<.001), with a mean difference of 199.69€. The mean cost of the surgery was higher in Group 1 (P<.001), with a mean difference of 157.49€. The mean cost per SLN analysis was significantly higher in Group 1, with a mean difference of 162.5€. The cost per patient was significantly higher in Group 1 (P<.005). A mean saving of 439.67€ per patient was achieved by using the OSNA method.
ConclusionIntraoperative molecular analysis for SLN metastases using the OSNA method reduces the number of admission days, duration of surgery, and achieves a saving of 439.67€ per patient.
El análisis molecular intraoperatorio del ganglio centinela con el método one-step nucleic acid amplification (OSNA) es una técnica ya validada para la detección de metástasis ganglionares en el cáncer de mama. Los autores comparan el coste económico de este nuevo método frente al estudio histopatológico convencional diferido.
MetodologíaEstudio retrospectivo de análisis coste-beneficio que incluyó a pacientes con cáncer de mama operable y axila clínica y ecográficamente negativa que fueron intervenidas desde el 15 de octubre de 2008 hasta el 15 de diciembre de 2009. El análisis del ganglio centinela se realizó en el Grupo 1 (45 pacientes) mediante estudio histopatológico convencional diferido, mientras que en el Grupo 2 (35 pacientes) se realizó según el método OSNA. Se analizaron las siguientes variables: edad, tamaño tumoral, tipo histológico, número de ganglios centinela, resultado de la biopsia, tiempo quirúrgico, días de hospitalización, complicaciones postoperatorias, ganglios positivos en caso de linfadenectomía axilar, coste por paciente, coste por hospitalización y coste por intervención.
ResultadosEl tiempo quirúrgico de la primera intervención en el Grupo 1 fue significativamente menor, pero el tiempo total fue mayor en el Grupo 1. La estancia media fue mayor en el Grupo 1 (p < 0,001). El coste medio de la estancia hospitalaria fue mayor en el Grupo 1 frente al Grupo 2 (p < 0,001), con una diferencia de medias de 199,69€. El coste medio de la intervención fue mayor en el Grupo 1 (p<0.001), con una diferencia de medias de 157,49€. El coste medio por análisis de ganglio centinela fue significativamente mayor en el Grupo 1, con una diferencia de medias de 162,5€. El coste total por paciente es significativamente mayor en el Grupo 1 (p<0,005). La aplicación del método OSNA consigue un ahorro medio de 439,67€ por paciente.
ConclusiónEl análisis molecular intraoperatorio del ganglio centinela mediante el método OSNA reduce los días de ingreso, el tiempo quirúrgico y proporciona un ahorro de 439,67€ por paciente.
The most efficient method for detecting metastases in sentinel nodes has not been clearly established. Various diagnostic techniques have been proposed, from cytology to the haematoxylin-eosin staining of serial histological sections of the entire lymph node, with or without the support of immunohistochemical techniques. It has been shown that the more thorough the study, the greater the number of metastases diagnosed.1 This can be performed during or after surgery. The first option has the advantage of allowing an axillary lymphadenectomy during the same intervention if metastases are detected. However, some studies have shown a percentage of false negative that can approach 52%.2 This is why a deferred histological examination is preferable, as it has greater sensitivity and is more definitive. Its main disadvantage is the need for reoperation if metastases are found in the sentinel node, in order to perform axillary lymphadenectomy. This requires readmission, which determines clinical efficiency, costs, and above all, the patient's psychological response.
The one-step nucleic acid amplification (OSNA) assay is a molecular technique that quantitatively measures the levels of cytokeratin 19 (CK19) messenger ribonucleic acid (mRNA), which is considered a marker for the presence of tumour cells in the lymph node. This method, which has been validated,3,4 allows for an intraoperative analysis of the sentinel node, with high sensitivity and specificity.
Once its effectiveness is established, we intend to analyse the economic benefit of this method compared to deferred histological examination of the sentinel node. The aim of this study is to analyse the economic costs of intraoperative application of the OSNA assay compared to the conventional deferred histological and immunohistochemical assay carried out in our hospital.
Material and MethodThis is a retrospective cost-benefit analysis. Patients were recruited from an Access® database that recorded all sentinel node biopsies (SNBS) reported by the pathology department since the implementation of this technique in our hospital in 2002 for the study of sentinel nodes in breast cancer patients. The following inclusion criteria were applied: patients with breast cancer stages pT1/2 N0 M05 with clinically and ultrasound negative axillary lymph nodes, who underwent SNBS along with appropriate breast cancer surgery in the same intervention by the breast unit of our hospital, during the period between 15 October 2008 and 15 December 2009. Patients signed an informed consent for performing this procedure.
Exclusion criteria were as follows: patients who had received neoadjuvant treatment, those who refused to sign the informed consent, patients who could not undergo the planned surgery due to high anaesthetic risk, patients who underwent previous extensive breast surgery, patients who underwent a SNBS with local anaesthesia before the definitive breast surgery (as they were candidates for immediate reconstruction or for receiving neoadjuvant chemotherapy with clinical N0 in order to reduce tumour size), pregnant women and males.
Based on these criteria, we had a series of patients who were grouped according to the type of histological analysis performed on the sentinel node. For group 1, SNBS were performed using conventional deferred histological technique (15 serial sections with alternating staining of haematoxylin-eosin and immunohistochemistry for cytokeratins), which included those patients operated on between 15 October 2008 and 14 May 2009. For group 2, lymph node analysis was performed using the OSNA assay during the period of time between 15 May 2009 (date on which the OSNA assay was implemented in our centre) and 15 December 2009.
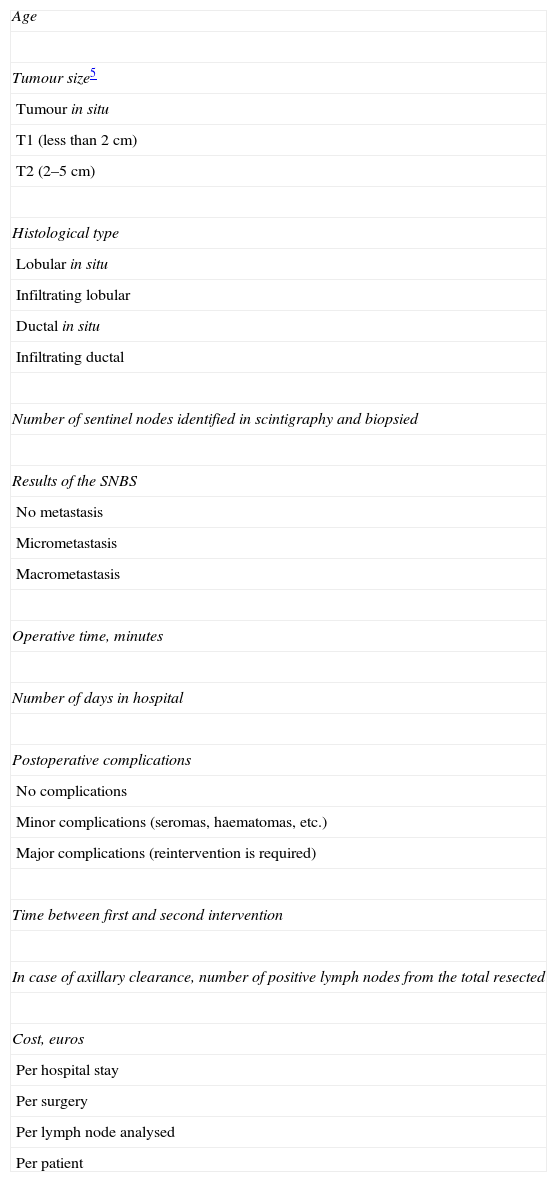
The analysed variables for both groups are shown in Table 1. Surgery times and admission dates were collected from medical records. The length of intervention was calculated from the initiation of anaesthesia to the exit from the operating room, reviewing the anaesthesia graphs.
Variables Analysed in the Study.
| Age |
| Tumour size5 |
| Tumour in situ |
| T1 (less than 2cm) |
| T2 (2–5cm) |
| Histological type |
| Lobular in situ |
| Infiltrating lobular |
| Ductal in situ |
| Infiltrating ductal |
| Number of sentinel nodes identified in scintigraphy and biopsied |
| Results of the SNBS |
| No metastasis |
| Micrometastasis |
| Macrometastasis |
| Operative time, minutes |
| Number of days in hospital |
| Postoperative complications |
| No complications |
| Minor complications (seromas, haematomas, etc.) |
| Major complications (reintervention is required) |
| Time between first and second intervention |
| In case of axillary clearance, number of positive lymph nodes from the total resected |
| Cost, euros |
| Per hospital stay |
| Per surgery |
| Per lymph node analysed |
| Per patient |
SNBS, selective sentinel node biopsies.
Breast cancer diagnoses were performed in our outpatient clinics, scheduling operations within 2 weeks after assessing the preoperative anaesthesia. The morning of the surgery, patients attended our nuclear medicine centre, where the breast lesions were located via ultrasound or stereotaxis. Radio-guided needles were placed at the centre of the lesions, through which a radiopharmaceutical agent was injected (0.5mCi to 1mCi of 99mTc albumin nanocolloid). After 2–3h, control lymphoscintigraphies were performed. Subsequently, patients were admitted to our hospital to complete the preparation for surgery, which would be performed on that same afternoon. The intervention involved a nuclear medicine specialist who traced the axillary region using a gamma detection probe. The sentinel node was defined as that which had an activity greater than 10% of the maximum activity detected. The operation then proceeded to the removal of this node.
Histological Study of the Sentinel Node (Group 1)After initial preparation of the lymph node using 4mm sections fixed in formalin and embedded in paraffin, 15 four-micron thick serial sections were cut and stained with haematoxylin–eosin and immunohistochemistry for cytokeratins. All preparations were examined by a pathologist using a conventional optical microscope, establishing the following stages5: negative (no metastatic cells), isolated tumour cells (focus of malignant cells ≤0.2mm), micrometastasis (>0.2mm and ≤2mm) and macrometastasis (>2mm).
Results were obtained within two weeks after surgery. If metastasis was found, a new operation for axillary lymphadenectomy was scheduled with readmission of the patient.
Sentinel Node Study Using the One-Step Nucleic Acid Amplification Assay (Group 2)The sentinel node was sent fresh to the pathology department (if there were more than one lymph node then all were sent at once). The fat was separated from the lymph node and sectioned if it weighed more than 600mg. The samples were then lysed by adding 4ml of the reagent Lynorhag® and centrifuged. The liquid phase of the mixture was placed in the OSNA RD100i, an analysis machine for automatic pipetting, amplification and detection.6 Results were obtained in approximately 30min. Data are expressed quantitatively according to the number of CK19 mRNA copies per tumour cell: no metastasis (<2.5×102 CK19 mRNA copies per μl), micrometastasis (from 2.5×02 to 5×103 CK19 mRNA copies per μl) and macrometastasis (>5×103 CK19 mRNA copies per μl). Once the sentinel node was extracted, breast surgery was performed according to preoperative indications. If OSNA metastasis was found, we proceeded to axillary clearance.
Cost AnalysisData were obtained from information provided by the accounting department of our hospital. The department's main purpose is to precisely know at all times the resources expended in the production of a product or department. Additionally, they measure and assess this production, monitor compliance with estimates and study the organisation's performance, and foresee and check its results so that, based on the development of the Proyecto Signo I (Sign I Project), the cost per department can be calculated, breaking down costs by procedures performed in them. In this particular case, we calculated the cost per procedure based on its specific DRG:
- -
The average cost of one day in hospital in the department of general and digestive surgery was 133.29€/day.
- -
The cost per minute of intervention (including the operating room, standard instruments, nursing staff, assistants, orderlies, two surgeons and an anaesthesiologist) was 9.93€/min.
- -
Sentinel node analysis, according to the conventional technique (cost includes consumables, but not the cost of pathology department personnel as they are paid by days worked, not by time [minutes] spent), has the same cost for both groups: 235€/lymph node.
- -
The cost of the sentinel node analysis using the OSNA assay2 is 190€/4 samples.
Considering that it was a financial/management assessment study of the quality of care, to achieve an accuracy rate of 0.14 and a 0.50 compliance rate (which ensures the necessary number of cases for 95% confidence), a sample size of 49 cases for each group would be necessary for its implementation to be feasible. Since the sample universe (No.=total cases/time period) is small (some 110 cases/year) and our sample is greater than 10% of No., we calculated a smaller sample size (n′), which maintains the same accuracy and confidence (n′=35), using the formula:
Data analysis was performed using the SPSS version 16.0 and IQUAL programs. We calculated the mean as a descriptive measure of central tendency, and used the standard deviation as a measure of data dispersion.
We used the Fisher's exact test for the analysis of qualitative dichotomous variables, ANOVA for continuous variables with homogeneous variance and Welch's correction when variances were not homogeneous. Statistical significance was established at P<.05.
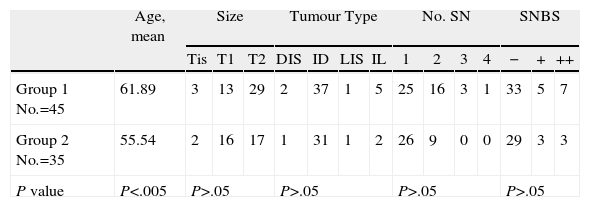
ResultsThere were no statistically significant differences in the general variables analysed in the study (tumour size, histological type, number of sentinel nodes (SN) and SNBS results [Table 1]), except for age (P<.005), which was greater in group 1 than in group 2. Table 2 shows the clinico-pathological characteristics of the two groups.
Characteristics of Each Group Analysed.
| Age, mean | Size | Tumour Type | No. SN | SNBS | |||||||||||
| Tis | T1 | T2 | DIS | ID | LIS | IL | 1 | 2 | 3 | 4 | − | + | ++ | ||
| Group 1 No.=45 | 61.89 | 3 | 13 | 29 | 2 | 37 | 1 | 5 | 25 | 16 | 3 | 1 | 33 | 5 | 7 |
| Group 2 No.=35 | 55.54 | 2 | 16 | 17 | 1 | 31 | 1 | 2 | 26 | 9 | 0 | 0 | 29 | 3 | 3 |
| P value | P<.005 | P>.05 | P>.05 | P>.05 | P>.05 | ||||||||||
−, negative; +, micrometastasis; ++, macrometastasis; SNBS, selective sentinel node biopsies; ID, infiltrating ductal; DIS, Ductal in situ; IL, infiltrating lobular; LIS, lobular in situ; No. SN, number of sentinel nodes; Tis, tumour in situ.
Operative time was lower for group 2 (Table 3). The mean total time difference for group 1 (mean: 78min; standard deviation: 48.02) compared to group 2 (mean: 62.14min; standard deviation: 21.93) was statistically significant (P<.005), with a difference between means of 15.86min. However, when only considering the operative time of the first intervention of group 1 compared to the time of group 2, the mean time is greater in the OSNA group (62.14min; standard deviation: 48.02) than in group 1 (57.11min; standard deviation: 23.93), although this difference was not statistically significant (P=.15).
Intervention Time and Days Hospitalised (and Cost) by Group.
| Intervention Time, Minutes | Days in Hospital | ||||||
| 1st Operation | 2nd Operation | Total | 1st Admission | 2nd Admission | Total | Cost (133.29€/day) | |
| Group 1 | |||||||
| Absolute no. | 2570min | 940min | 3510min | 81 days | 29 days | 110 days | 14 661.90€ |
| Mean | 57.11min | 78.33min | 78min | 1.8 days | 2.41 days | 2.44 days | 325.22€ |
| Group 2 | |||||||
| Absolute no. | 2175min | – | 2175min | 54 days | – | 54 days | 7197.66€ |
| Mean | 62.14min | – | 62.14min | 1.54 days | – | 1.54 days | 205.53€ |
min, minutes.
Mean hospital stay after the first intervention in group 1 was 1.8 days (range: 1–13; standard deviation: 2.04), while hospital stay for the second intervention was 2.41 days (range: 1–6; standard deviation: 1.29, over 12 patients), resulting in an overall calculation of 2.44 days for group 1 (standard deviation: 3.003), Table 3. Mean hospital stay was greater in any case to that found in group 2 (mean: 1.54 days; range: 1–4; standard deviation: 0.78), which was a statistically significant difference (P<.001). There were no statistically significant differences if one only considers the mean stay of the first admission of group 1 compared to the stay of the OSNA group (P>.1).
Hospital CostsOne day in hospital in the unit of the department of general and digestive surgery has a mean cost of 133.29€. Therefore, taking into account the average stay of both groups, group 1: 2.44 days, and group 2: 1.54 days, the cost for hospital stay has an average value of 325.22€ (standard deviation: 400.26) and 205.53€ (standard deviation: 133.96), for both groups, respectively. This difference, 119.69€, is statistically significant (P<.001).
One minute in the operating room is valued at 9.93€/minute. Therefore, in terms of surgery costs (Table 4), the mean cost per patient for group 1 was 774.54€ (standard deviation: 476.83) and 617.05€ for group 2 (standard deviation: 217.76). The difference was 157.49€, which was statistically significant (P<.001).
Cost per Minute of Intervention and Cost per Sentinel Node Analysis.
| Minutes in Operating Room (9.93€/minute) | Lymph Node Analysis | |||
| Minutes | Cost | No. SN | Cost (235€/Lymph Node) | |
| Group 1 | ||||
| Absolute no. | 3510min | 34 854.43€ | 70 lymph nodes | 16 450€ |
| Mean | 78min | 774.54€ | 1.5 lymph nodes | 352.50€ |
| Minutes | Cost | No. SN | OSNA cost (190€/4 samples) | |
| Group 2 | ||||
| Absolute no. | 2175min | 21 597.75€ | 44 lymph nodes | 6650€ |
| Mean | 62.14min | 617.05€ | 1.25 lymph nodes | 190€ |
SN, sentinel node; OSNA, one-step nucleic acid amplification.
With regard to costs for laboratory analysis of sentinel nodes, group 1 had a mean of 352.50€ per patient, while group 2, using the OSNA assay, had a mean of 190€. The difference, 162.50€, is statistically significant (P<.05).
Therefore, the total cost of intervention (operating room and laboratory) was: group 1: 774.54€+352.5€=1127.04€; group 2: 617.05€+190€=807.05€. The mean savings was 319.99€ per patient per intervention.
Overall CostsThe total of the mean cost of the hospital stay, surgery, and lymph node analysis per group was: 1127.04€+352.22€=1452.25€ for group 1 and 807.05€+205.53€=1012.58€ for group 2. Therefore, the difference between means is 439.67€, which is statistically significant (P<.005) in favour of the OSNA group.
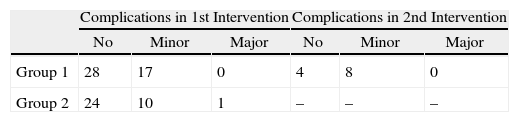
ComplicationsThe analysis of complications (minor, major and no complications) of group 1 (considering the 1st and 2nd intervention) compared to those of group 2, showed statistically significant differences (P=.015), which were lower in the OSNA group (Table 5).
LymphadenectomyAxillary lymphadenectomies were performed on 12 patients from group 1, obtaining an average of 20.66 lymph nodes (range 11–30). In four cases, another lymph node was found, which was metastatic and different from the sentinel (three cases resulted in macrometastasis and one in micrometastasis). The mean time between the two interventions in this group was 23.16 days (range 10–37).
With respect to group 2, six patients underwent lymphadenectomy, finding an average of 16.5 axillary lymph nodes (range 12–22). Only in one case another lymph node with tumour dissemination was isolated (with SNBS corresponding to macrometastasis). There were no statistically significant differences between the two groups.
DiscussionCurrently, there are two molecular tests for intraoperative analysis of sentinel nodes: GeneSearch BLN (Veridex, Warren, New Jersey, USA)7,8 and OSNA (Sysmex, Kobe, Japan).3,4 Both methods amplify and detect RNA of metastatic cells in lymph nodes. We chose the OSNA assay because it was available in our hospital.
The OSNA is a method for the analysis of RNA sequences by reverse transcription loop-mediated isothermal amplification. It is a molecular test designed for detecting mRNA in epithelial cells, which normally should not be present in lymph nodes. CK19 is expressed in most epithelial cells and many types of cancer, but not by lymphocytes in lymph nodes, peripheral blood cells or bone marrow cells. Hence, CK19 mRNA is useful for detecting metastasis in breast cancer.9
Among the main advantages of this method are: high sensitivity and specificity (95.3% and 94.7%, respectively3,4,10), speed (intraoperative use), high degree of automation, cost-effectiveness and that it does not require sterile working conditions or high temperatures for denaturation and hybridisation of nucleic acid chains.
However, this method is not appropriate for patients previously subjected to breast surgery because the CK19 expressed in epidermal cells, which migrate to the inside of the breast during surgical manoeuvres and reach the sentinel node, may be detected by the OSNA assay and interpreted as a false positive. For this reason, this patient group was not included in our study.
Given the above advantages, we opted for the inclusion of the OSNA assay in our hospital and compared its cost analysis with that of the deferred histological study of lymph nodes that was performed previously. Our hospital has no experience in intraoperative analysis of frozen sentinel nodes, and we have found only one recent study that compares it to the OSNA assay.11 The study described two cohorts of patients; an intraoperative analysis by freezing is used in one of them and an analysis using OSNA in the other. They concluded that molecular analysis using OSNA detected more micrometastases, especially in postmenopausal women with tumours that have low aggressiveness (no lymphovascular invasion). This may be due to the fact that the OSNA method analyses the entire sentinel node, while the study of frozen sections does not analyse the entire nodes. Despite this, it cannot be considered a diagnostic test study since it should be the same case evaluated by both techniques.
The two groups of patients compared had no statistically significant differences in terms of tumour stage, histological type, number of sentinel nodes found and SNBS results. It should be noted that we did find a difference in age (P<.005) although we do not believe it to be a relevant datum per se in possible biases for this variable.
Although the OSNA assay is a system already validated in other countries,3,4,10 we have not found studies in the literature that compare this new diagnostic method with other techniques in terms of time of the procedure, costs, etc., as is the objective in our study. The OSNA assay reduces the overall figure for minutes in the operating room (P<.05), which is mainly due to the lack of need for a second intervention. This is because it enables lymphadenectomy to be performed in the same surgical act in case of metastasis in the sentinel node. This means savings in surgery times, personnel costs and use of the operating room (P<.001), thereby reducing the mean cost per intervention: 774.54€ (group 1) and 617.05€ (group 2). If we also add the mean costs per patient for lymph node analysis, this results in a mean savings of 319.99€ per patient.
Furthermore, we found that the hospital stay was longer for group 1 (mean: 2.44 days) than for group 2 (mean: 1.54 days) with P<.001. This may be explained by the fact that group 1 included two interventions along with their respective postoperative periods. However, it is noteworthy that there were no significant differences when comparing mean stay for the first admission of group 1 with group 2, since we can assume that the latter was greater due to the requirement for having a more extensive surgery (lymphadenectomy in some cases).
Therefore, in terms of costs per hospital day, group 1 had a mean of 325.22€ per patient, while group 2 had a mean of 205.53€ per patient, which was statistically significant (P<.001), with a mean difference of 119.69€.
If we consider the overall mean cost of the hospital stay and the surgery by group, we would conclude that the mean cost for group 1 was significantly greater, which would mean a savings of 439.67€ per patient and per procedure when applying the OSNA assay.
By avoiding a second intervention, one also achieves a reduction in time spent caring for the patient, since cutting operative time, we reduce the time needed for patient care up to the adjuvant treatment, as well as the emotional impact caused by reoperations.
We conclude that intraoperative analysis of the sentinel node using the OSNA assay significantly reduces the costs, compared to conventional analyses. The assay can be performed within an acceptable time period, allowing for completion of axillary surgery in the same operation, if necessary. This reduces the mean hospital stay and operative time and avoids a second intervention for lymphadenectomy.
FundingThis article was funded in part by the Fundación para la Formación e Investigación Sanitaria de la Región de Murcia (foundation for healthcare research and training of Murcia, FFIS), Grupo FFIS-008.
Conflicts of InterestThe authors have no conflicts of interest to declare.
Please cite this article as: Guillén-Paredes MP, et al. El análisis molecular intraoperatorio (one-step nucleic acid amplification) del ganglio centinela como alternativa al estudio histopatológico diferido en el cáncer de mama: ana¿lisis coste-beneficio. Cir Esp. 201189:456–62.