Paget–Schroetter Syndrome is a relatively uncommon but especially important disease as it affects healthy, young subjects.1 Its management is controversial and usually requires medical, surgical and endovascular treatment.
We present the case of a 48-year-old woman, a smoker (20 pack-years) without any other prior medical history, who came to our Emergency Department due to pain and edema in the upper right extremity of less than 24h duration. General physical examination was normal. The right upper limb presented venous congestion, also seen in the anterior chest. On venous ultrasound, no flow was observed in the right subclavian vein.
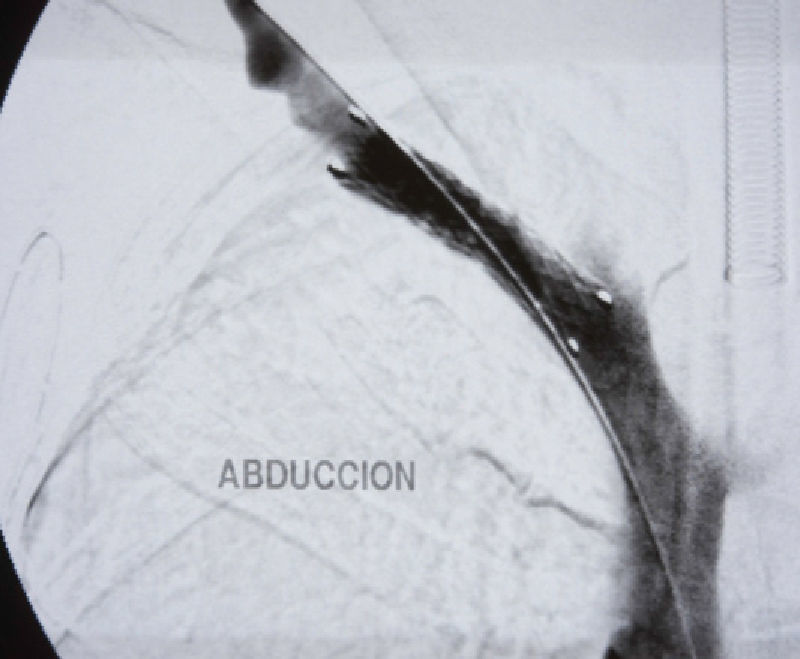
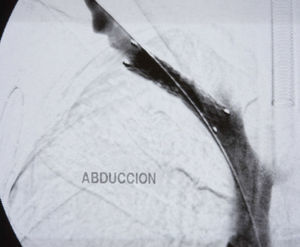
With the diagnosis of deep vein thrombosis of the upper right limb, we decided to carry out phlebography with a hollow fibrinolysis guide (0.035mm) and at the same time intra-thrombus fibrinolysis was initiated with urokinase at an initial dose of 250 000U and later 60 000U/h. We ordered a series of radiological controls to follow the evolution and to be able to reposition the catheter. Forty-eight hours afterwards, and after having confirmed the lysis of the thrombus, it was decided to suspend fibrinolysis, perform angioplasty with an 8mm×40mm balloon, and initiate anticoagulation until surgery (Fig. 1). Four weeks afterwards, decompression surgery was performed with transaxillary resection of the first rib. On the routine post-operative phlebography examination, significant residual stenosis and the presence of abundant collateral circulation were observed, and an 8mm×40mm stent was implanted to correct the stenosis (Fig. 2). Currently, one year after surgery, the patient remains asymptomatic.
Paget–Schroetter syndrome is a primary thrombosis of the subclavian vein in the subclavian-axillary junction. It is caused by compression of the subclavian vein as it passes through the triangle created by the anterior scalene muscle, the first rib and the subclavius muscle and tendon.2
The incidence of this syndrome is 2 per 100 000 inhabitants. It affects young adults (mean age 32), mainly males (2:1),3 in the dominant upper extremity. Some 80% of patients report prior important physical activity with movements of external rotation and separation.
Classical symptoms include pain, edema and sensation of heaviness in the affected limb.4 Onset is abrupt: in 85%1 of cases, the symptoms start within 24h of doing exercise.
Doppler ultrasound5 is the first diagnostic technique required. In expert hands, it is very sensitive (78%–100%) and specific (82%–100%).6 The following step is phlebography, with which thrombosis of the subclavian-axillary vein in the costoclavicular union and presence of abundant collateral circulation can be observed.1 If an obstruction is not observed, the presence of collateral circulation always indicates a certain degree of stenosis. Provocation maneuvers, such as the separation of the extremity, may help in the diagnosis.1
There is no clear consensus regarding treatment. Nowadays, most authors agree that anticoagulants as a monotherapy offers poor results,7 and it is therefore recommended to use associated fibrinolysis and surgical and/or endovascular treatment.8
Fibrinolysis with intra-thrombus urokinase or streptokinase in the acute phase (within 10 days) is very effective (up to 100%) and safe, making it the treatment of choice.5 Given that the disappearance of the thrombus does not resolve the symptoms nor does it eliminate the venous compression, decompression surgery is recommended. Prior to surgery, angioplasty or the use of a stent are not indicated as they may further damage the endothelium and the joint may obstruct or even break the stent.4
The most widely used decompression technique2 is transaxillary first rib resection as it has low morbidity and excellent esthetic results. Its main complications are injury to the long thoracic nerve, hemopneumothorax and resection of the second rib. Other approaches, such as sternal de-articulation, claviculectomy or supra/infraclavicular approaches, have also been described. One of the advantages of the latter is the possibility to perform complete venous reconstruction9 in cases with persistent symptoms or hemodynamic defects.
The timing of surgery is still a subject of debate. Some authors recommend 3 months after fibrinolysis, since the rate of complications is lower,5 while the most recent series propose immediate surgery due to the risk of recurrence before surgery, and recovery is also faster.7 Either way, patients should take anticoagulants for 3–6 months after decompression.
In the cases in which the results are suboptimal after surgery, angioplasty or stent placement can be considered, although, if possible, their use should be preferably avoided.7
In conclusion, Pager–Schroetter syndrome is an underdiagnosed pathology that affects young individuals in their dominant extremity. The most widely accepted management is fibrinolysis as soon as possible, decompression surgery and anticoagulation, after which there are fewer side effects and more than 90% of patients return to their usual activities.
Please cite this article as: Botas Velasco M, Calvín Álvarez P, Vaquero Lorenzo F, Álvarez Salgado A, Álvarez Fernández LJ. Síndrome de Paget-Schroetter. Cir Esp. 2013;91:392–393.