Approximately 70% of patients with familial adenomatous polyposis (FAP) present adenomas in the duodenum.1–4 There are several types of treatment for these lesions: endoscopic removal, local surgical resection1–4 and in certain cases the duodenum should be removed.1–4 Classically, this was done by pancreatoduodenectomy (PD), but in 1995 Chung et al. described the technique of pancreas-preserving total duodenectomy (PPTD), which offers certain advantages over PD.1–8 Only about 100 cases of PPTD were published before 2010.4,9 We present a case of duodenal polyposis treated with PPTD.
The patient is a 46-year-old woman with familial polyposis of the colon, who had been operated on in another center at the age of 14 with colectomy and ileorectal anastomosis; at the age of 25, the patient underwent resection of the rectum and ileoanal anastomosis with an ileal pouch. Her father and brother had also undergone surgery for FAP. Follow-up gastroduodenoscopy revealed multiple sessile and flat polyps in the second and third duodenal portions measuring from a few millimeters up to 2.5cm. Biopsy of the 3 larger adenomatous polyps (2–2.5cm) confirmed moderate epithelial dysplasia. Endoscopic ultrasound and capsule endoscopy confirmed the findings without observing other intestinal lesions. It was classified as a Spigelman grade IV duodenal polyposis (Johnson), and a PPTD was decided.
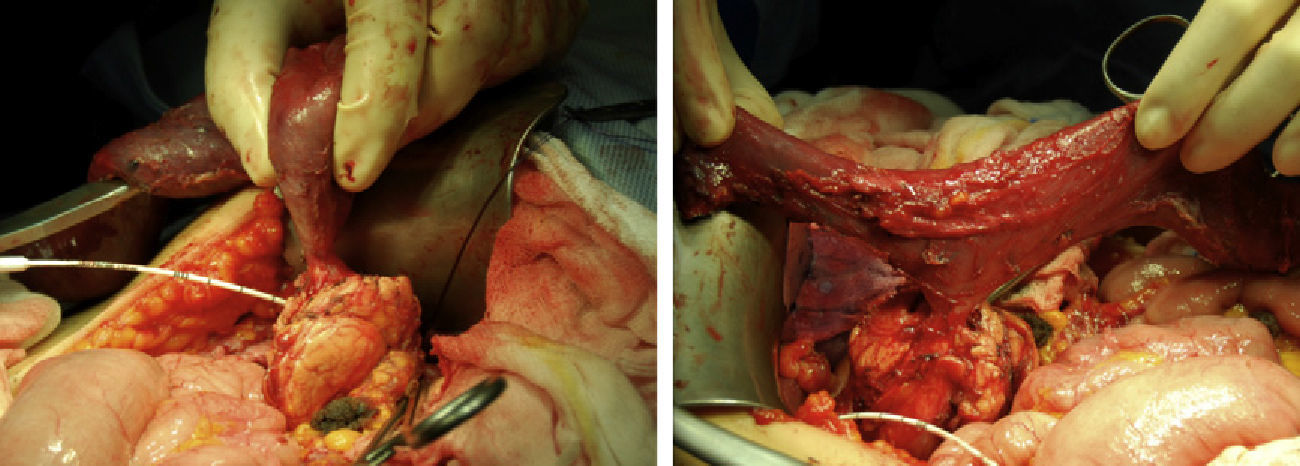
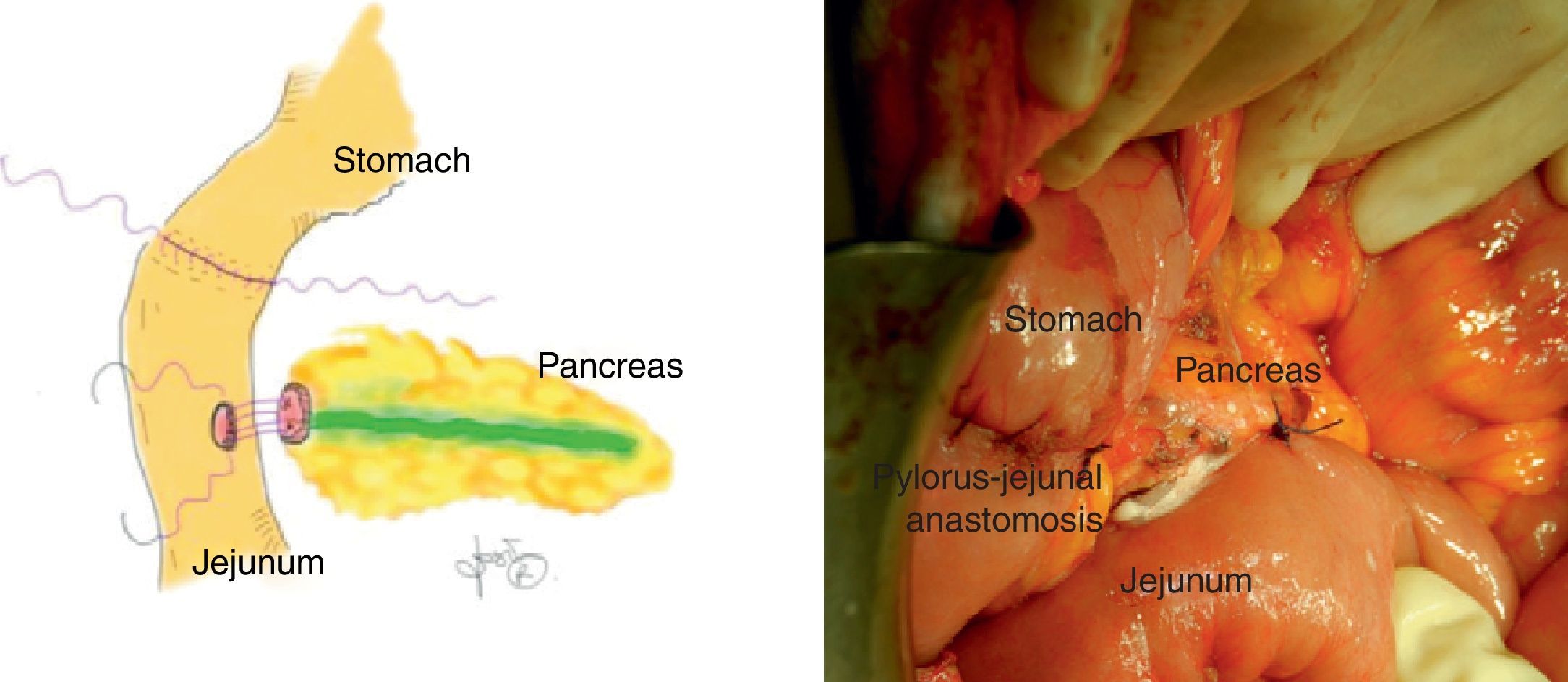
The surgical technique1,4–8 consisted of a bilateral subcostal laparotomy; the duodenum was transected with a stapler 3mm distal to the pylorus at the angle of Treitz. The distal duodenum was freed and mobilized behind the mesenteric vessels. An extensive Kocher maneuver was used to be able to free the duodenum from the retroperitoneal plane. Cholecystectomy and placement of a transcystic catheter allowed us to locate the ampulla of Vater by palpation. Careful separation was initiated of the infra-ampullary duodenum, head of the pancreas and uncinate process, transecting multiple pancreatic-duodenal branches. Afterwards, the same maneuver was done at the supra-ampullary area. One should always try to identify a possible accessory pancreatic duct, but this was not present in our patient. Finally, the pancreas and duodenum were only joined by the ampulla of Vater (Fig. 1). A small oval was created in the duodenum around the papilla in order to complete the duodenectomy. We verified that there were no polyps in the 2–3mm of duodenal mucosa surrounding the papilla. We performed a sphincterotomy to increase biliopancreatic drainage. Then, the proximal jejunum was situated in the place that was occupied by the duodenum (neoduodenum) with the mesentery located behind the pancreas, and a monoplane mucosa-mucosa ampulla-jejunal anastomosis was performed with single 4/0 PDS stitches as well as a pylorus-jejunal anastomosis (Fig. 2A and B). The jejunum was attached to the head of the pancreas with 2 stitches and a silicone suction drain was inserted close to both anastomoses. The patient initiated oral intake on the 4th day post-op. The post-operative period was uneventful, with no transfusion required, and the patient was discharged from the hospital on the 10th day post-op. The histologic study confirmed the existence of diffuse duodenal adenomatous polyposis with hundreds of polyps of different sizes (1–25mm), with mild and moderate dysplasia.
About 5% of duodenal polyposis in FAP develop duodenal cancer, a percentage which reaches 36% in patients with advanced disease.4,9 The main objective in duodenal polyposis is to prevent the appearance of cancer and avoid complications (bleeding and obstruction).9 Spigelman et al. developed a stage classification for the severity of duodenal polyposis based on the number of polyps, size, histology and degree of dysplasia.2,9,10 Stages I to III can be treated with endoscopic polypectomies or local resections if there is not a great degree of dysplasia or complications, but the rate of recurrence is high.8,9 In stages IV or III with high grade dysplasia, the duodenum should be completely removed.9,10
PPTD consists of resection of the entire duodenum with preservation of the head of the pancreas.1–8 It is indicated in neoplastic or preneoplastic lesions that diffusely affect the duodenal mucosa, but with no potential for extension to the regional lymph nodes,5,7 and it should not be performed in patients with confirmed cancer.3,4 The most frequent indication of PPTD is familial adenomatous polyposis of the duodenum (Spigelman IV or III with severe dysplasia).1,7,9 Other indications are: periampullary adenomas, multiple duodenal gastrinomas or duodenal trauma.4–7
The advantages of PPTD over PD are: more conserved intestinal function, preservation of pancreatic tissue, 2 anastomoses versus 3, avoidance of hepaticojejunostomy in a non-dilated bile duct and a pancreatojejunal anastomosis in a pancreas that is usually soft with a non-dilated pancreatic duct, shorter surgical time, less intraoperative bleeding and it allows for better endoscopic follow-up.3,4,6–9 Furthermore, PD due to duodenal polyposis presents higher morbidity than PD performed for other indications.3
The mean published morbidity of PPTD is 60%, including 25% minor and 35% major complications.2,4 The complications described are: delayed gastric emptying, fistula of the pylorus-jejunal or ampulla-jejunal anastomoses, intraabdominal abscess, acute pancreatitis and infection of the surgical wound.1,4 There have been no reports of mortality associated with this procedure.2,4 The recurrence rate after PPTD is 9%, occurring in the small post-pyloric duodenal sleeve or in the mucosa surrounding the papilla.9
In conclusion, PPTD is a complex technique with very specific indications that presents an acceptable morbidity and provides advantages over PD.
Please cite this article as: Ramia-Angel JM, Quiñones-Sampedro JE, De La Plaza Llamas R, Gomez-Caturla A, Veguillas P. Duodenectomía total con preservación pancreática. Cir Esp. 2013;91:466–468.