Peritoneal dialysis is a therapeutic alternative that is being increasingly used in patients with advanced chronic kidney disease. It requires the placement of a peritoneal dialysis catheter, which is often done by a general surgeon, and the infusion of dialysis fluid into the peritoneal cavity with the consequent increase in intra-abdominal pressure.1 Complications derived from this procedure are typically infectious or mechanical, and the appearance of a pleuroperitoneal communication is a rare entity, with an average incidence of 1.6%–10%.2 There is a long list of possible causes for its appearance, including acquired or even congenital pleuroperitoneal defects.3 The objective of our study is to present a case treated at our hospital and inform the surgical community of its occurrence in order to detect this problem earlier.
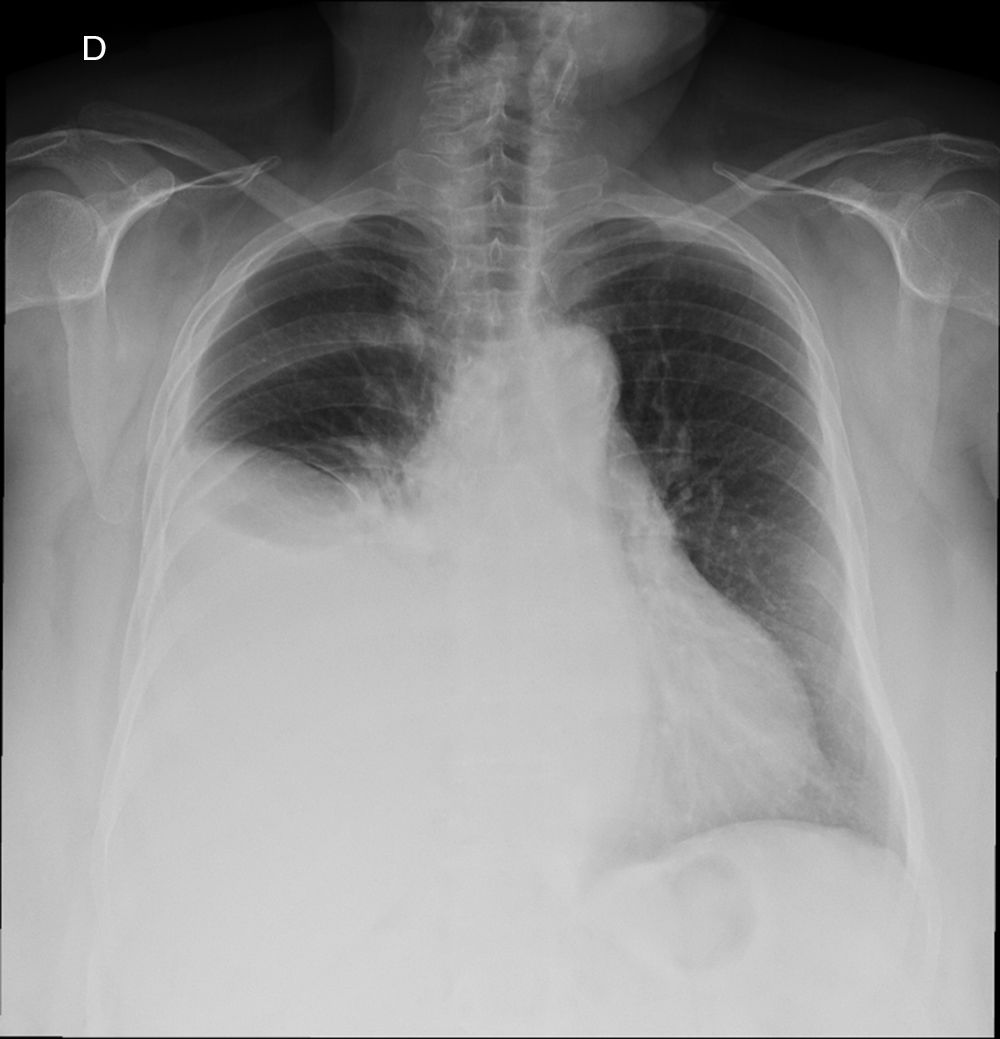
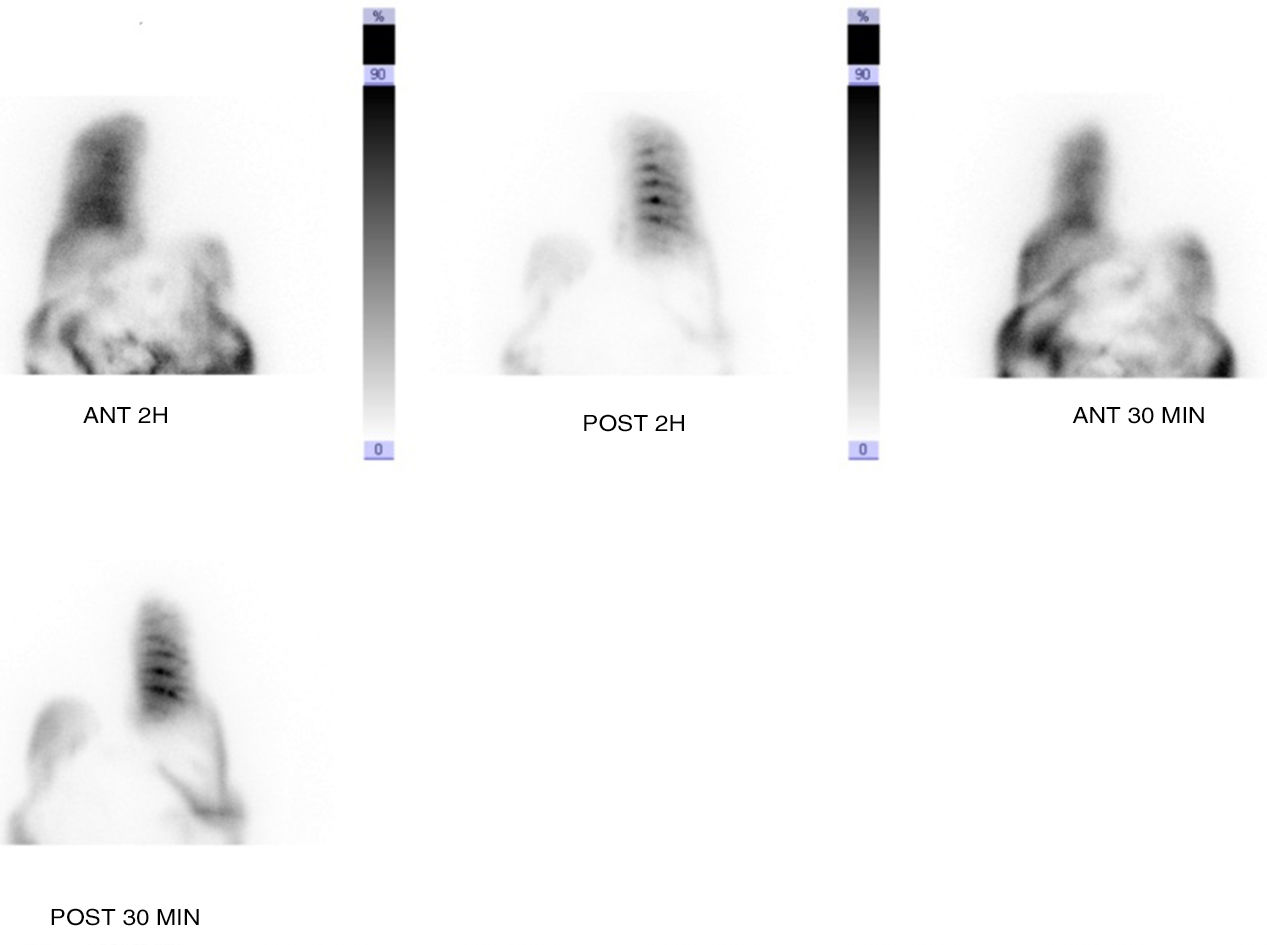
We present the case of a 70-year-old woman with a history of hypertension, type 2 diabetes mellitus, hyperlipidemia, and chronic kidney disease secondary to nephroangiosclerosis and/or diabetic nephropathy. The chronic kidney disease required peritoneal dialysis catheter placement. The catheter placement technique was done under local anesthesia and sedation, with no incidents. Three months after starting a peritoneal dialysis program, the patient came to the emergency room with dyspnea as the main symptom. A simple chest radiograph demonstrated a large right pleural effusion (Fig. 1). Thoracentesis and analysis of the sample obtained a glucose concentration higher than the plasma concentration. With a suspected diagnosis of pleuroperitoneal communication, scintigraphy with Tc-99 was requested, which confirmed the diagnosis (Fig. 2), and the patient was given a rest from dialysis and changed to hemodialysis. Given the lack of response to this approach, the catheter was definitively removed and the patient referred to a hemodialysis program.
Pleuroperitoneal communication is a rare entity in patients undergoing peritoneal dialysis. Its incidence varies according to the series (1.6%–10%), which may be due to the variable capacity to diagnose low-volume hydrothorax.3,4 Some authors report a higher incidence in women, as in the case presented, and in certain etiologies, such as polycystic kidney disease, which was not present in our patient.5 Regarding its location, the majority of cases are presented on the right side, as in the case presented, and bilateral presentations are exceptional.6 Some authors explain this finding as the existence of an embryonic remnant that allows the passage of fluids from the abdominal cavity to the right pleural space.7
This diagnosis should be suspected in patients on peritoneal dialysis who present dyspnea more or less abruptly and in whom right pleural effusion is observed on simple chest radiography.8 Analysis of the pleural fluid may show higher glucose levels than plasma glucose levels, which is a very indicative sign.9 The study is confirmed by a scintigraphy showing the passage of the radioactive isotope from the abdominal cavity to the pleural cavity.10 Treatment is fundamentally based on “peritoneal rest” and changing to hemodialysis temporarily or definitively, which may be accompanied by pleurodesis. Surgical treatment involving closure of the communication is the option least used, partially due to the limited relevance of this entity outside the scope of peritoneal dialysis.8 Similar to the case presented, most authors prefer conservative treatment, which achieves success in more than 50% of cases.3
In the case of pleurodesis, this can be done mechanically or chemically and has been shown to be a good, safe option.9 The rate of recurrence after timely treatment is high, requiring a definitive step to hemodialysis in a high proportion of cases, as occurred in the case presented.10 Some authors prefer surgical treatment of the pleuroperitoneal fistula by means of thoracoscopy as a definitive solution, thereby allowing continuous ambulatory peritoneal dialysis to resume between 2 and 4 weeks after surgery, with no reported recurrences. Thoracoscopic vision prior to any surgical approach is very useful for ensuring the existence of a visible and repairable communication.11–15 Good results have been demonstrated by direct closure at the points of the pleuroperitoneal leak with absorbable polyglycolic acid material and fibrin glue.11 Video-assisted thoracoscopic surgery (VATS) has provided definitive treatment of fistulae using collagen tissue and fibrin glue,12 while other groups opt for diaphragmatic repair and pleurodesis with hypertonic glucose, obtaining good results.13,14
Pleuroperitoneal communication is a rare pathology in patients on peritoneal dialysis that should be understood by general surgeons involved in the placement of dialysis catheters. It should be suspected in the presence of sudden dyspnea confirmed by scintigraphy. Fundamentally, treatment involves peritoneal rest accompanied or not by pleurodesis, although some groups conduct surgical treatment.
Please cite this article as: Reoyo Pascual JF, Cartón Hernández C, León Miranda R, Camarero Temiño V, Sánchez Manuel J. Comunicación pleuroperitoneal en paciente de diálisis peritoneal: un caso de interés para el cirujano. Cir Esp. 2018;96:311–312.