Chronic anal pain is a common condition related to several pathologies, from proctalgia fugax to coccydynia or anismus. Its presentation usually causes psychosocial disturbance to patients, which leads to a poor quality of life. The etiology continues to be unknown, although some findings, such as increased anal canal pressure,1 myopathy of the internal anal sphincter2 or neuropathy of the pudendal nerve caused by entrapment or perineal descent, have been described associated to certain patient groups.3 Psychological factors have also been considered as a possible etiologic factor of these symptoms, although most patients demonstrate associated depression as a result of several months of untreatable anal pain.
To date, no treatment has been shown effective for chronic anal or perianal pain. There have been reports using lateral internal sphincterotomy,4 nitroglycerin5 or botulinum toxin injection with no significant improvements reproducible by other authors.
Sacral nerve stimulation (SNS) was first used in 2007 to treat a case of idiopathic chronic anal pain6 and another study was later published7 to demonstrate its usefulness. We present 3 cases of patients with chronic idiopathic anal pain that was resistant to treatment and was treated with sacral root stimulation.
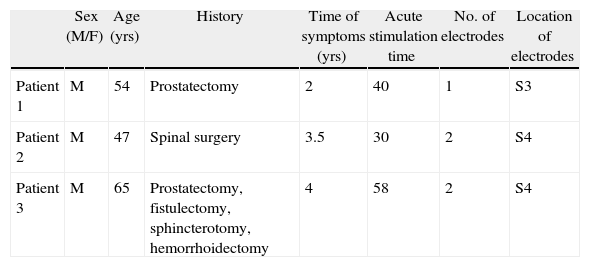
The 3 patients (Table 1) were assessed by endoanal ultrasound and rectoscopy to rule out organic pathologies responsible for the symptoms. We also ruled out suppurative disease, anal fissure, hemorrhoids or other pathologies that would explain the symptoms. Patients were assessed and treated by the Pain Management Unit and were once again referred to our department because they did not respond to medical treatment and required high doses of opioid analgesics that failed to control their symptoms.
Patient Characteristics.
| Sex (M/F) | Age (yrs) | History | Time of symptoms (yrs) | Acute stimulation time | No. of electrodes | Location of electrodes | |
| Patient 1 | M | 54 | Prostatectomy | 2 | 40 | 1 | S3 |
| Patient 2 | M | 47 | Spinal surgery | 3.5 | 30 | 2 | S4 |
| Patient 3 | M | 65 | Prostatectomy, fistulectomy, sphincterotomy, hemorrhoidectomy | 4 | 58 | 2 | S4 |
The SNS surgical technique has been previously published by the authors8 and it consists of the first stage of acute stimulation done under local anesthesia and placement of a quadripolar electrode (R 3889-28, Medtronic, Minneapolis, USA). Responses to stimulation were assessed at different voltages, leaving the stimulation electrode in the sacral foramina of the root that obtained the best sensory-motor response, which was then connected to an external current-generating device. During the second stage of subchronic stimulation, patients evaluated the effectiveness of the stimulation current using the EQ-5D and visual analog scale (VAS). The third stage, or permanent stimulation, was performed only if the results were satisfactory and involved the placement of an internal battery in a subcutaneous space in the buttocks, which is also done under local anesthesia. Definitive neuromodulator placement was decided upon when there was an improvement of at least 50% in the perception of quality of life and VAS pain scale.
The stimuli ranged from 0.5 to 1.5V, and the pulse width and frequency were constant (210ms and 25Hz, respectively). Stimulation was initially done in continuous mode and, at times, in discontinuous mode if the response was not sufficient.
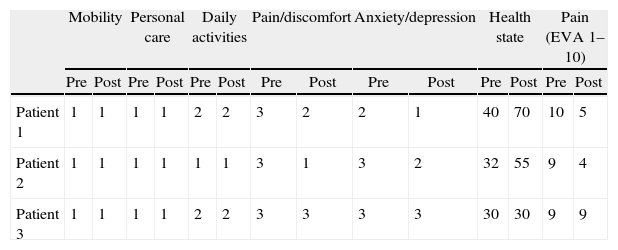
In order to measure the effectiveness of the treatment, 3 patients were given the self-administered visual analog pain scale (1 no pain, 10 maximum pain) and also the self-administered EuroQol-5D (EQ-5D) questionnaire9 before the intervention and one and six months after it (in the 2 patients with definitive implants). The EQ-5D questionnaire consists of 2 parts: the first allows the patient to define health status according to the EQ-5D multi-attribute classification system (5 dimensions: mobility, personal care, daily activities, pain/discomfort and anxiety/depression); the second part is a visual analog scale (VAS) graded from 0 (“worst imaginable health state”) to 100 (“best imaginable health state”). One-digit numbers (1, 2 or 3) are obtained to express the level selected for each dimension.
Two of the 3 patients (Table 2) obtained improvement in the perception of pain (VAS) of more than 50% and an improvement in perceived health status of more than 50% that has continued to date after a follow-up of 24 months in the first patient and 18 months in the second patient. The third patient experienced no improvement in these or other parameters; therefore, the intensity, frequency and amplitude parameters were changed, but, after no response in pain perception was detected, the placement of the definitive stimulator was not performed.
Results Before (pre) and After (Post) Subchronic Stimulation Measured With the EuroQol 5D and VAS for Pain.
| Mobility | Personal care | Daily activities | Pain/discomfort | Anxiety/depression | Health state | Pain (EVA 1–10) | ||||||||
| Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | |
| Patient 1 | 1 | 1 | 1 | 1 | 2 | 2 | 3 | 2 | 2 | 1 | 40 | 70 | 10 | 5 |
| Patient 2 | 1 | 1 | 1 | 1 | 1 | 1 | 3 | 1 | 3 | 2 | 32 | 55 | 9 | 4 |
| Patient 3 | 1 | 1 | 1 | 1 | 2 | 2 | 3 | 3 | 3 | 3 | 30 | 30 | 9 | 9 |
Treatment with SNS is effective in some patients with severe chronic anal pain. Some authors have demonstrated its cost-effectiveness because of the lower number of treatments, medical visits and sick leaves from work required by these patients.10 We believe that patients should first be studied in detail to rule out any other treatable pathology, which might resolve the cause of the pain. In those patients with no clear etiology in whom medical treatments have failed, SNS can be used empirically and, if its effectiveness is demonstrated by the use of pain scales and quality-of-life studies, the definitive stimulator should be implanted.
Please cite this article as: Soria-Aledo V, Pellicer-Franco E, Mengual-Ballester M, Valero-Navarro G, Aguayo-Albasini JL. Estimulación de raíces sacras para el dolor anal intratable. Cir Esp. 2014;92:64–65.