Hemorrhoids are the most frequent proctologic disease. Their incidence, however, is difficult to establish, since many patients do not go to the doctor.1 There is a maximum incidence between the ages of 45 and 60, with a peak of 50% in people over 50. The distribution between sexes is similar.2
The initial treatment is based on dietary and hygienic or instrumental measures, but currently up to 10% of patients with clinical persistence require surgical intervention. The reference technique continues to be Milligan-Morgan hemorrhoidectomy.3
There is a significant group of patients affected by other diseases in whom the surgical treatment of hemorrhoidal disease would be inadvisable. Patients with inflammatory bowel disease (IBD) can present with hemorrhoids, with an estimated incidence of 7% in patients with Crohn's disease.4 However, many patients do not consult for hemorrhoid symptoms, blaming their discomfort on IBD. In these patients, especially in the case of presenting local inflammatory crises, hemorrhoidectomy or even ligation may entail major complications.5,6 The reported complication rates ranges from 15 to 40% in Crohn's disease (CD).7,8
Another group at risk for hemorrhoidectomy are patients with a certain degree of fecal incontinence or who have undergone anal surgery procedures, such as internal fistulotomy or sphincterotomy. The excision of the hemorrhoidal plexuses could trigger or aggravate the existing incontinence.
Other patients who are not good candidates for surgery include those who are immunosuppressed, induced either by drugs or by viral disease.
In 2014, Vidal et al.9,10 described the “Emborrhoid” technique, consisting of selective occlusion of the superior rectal artery, decreasing the hyperflow of blood in the hemorrhoidal venous cushions. It is based on the same technical principles as the selective ligation of hemorrhoid arterial pedicles detected by Doppler; however, by using endovascular treatment, anorectal manipulation is avoided.
We present the first 3 cases of patients with grade II–III internal hemorrhoids with failed conservative management who were treated with selective superior rectal artery embolization (SRAE), all with no fecal incontinence, as measured according to the Wexner scale:
- -
Case 1: a 46-year-old woman with CD, no perianal involvement and symptoms including rectal bleeding, proctalgia and intermittent prolapse, as well as frequent diarrhea.
- -
Case 2: a 43-year-old woman with ulcerative colitis (UC) and ankylosing spondylitis, with adequate rectal control using adalimumab; symptoms include daily proctalgia and rectal bleeding.
- -
Case 3: a 72-year-old male diagnosed with UC and HIV positive with adequate CD4 lymphocyte count; symptoms of rectal bleeding and prolapse requiring manual reduction.
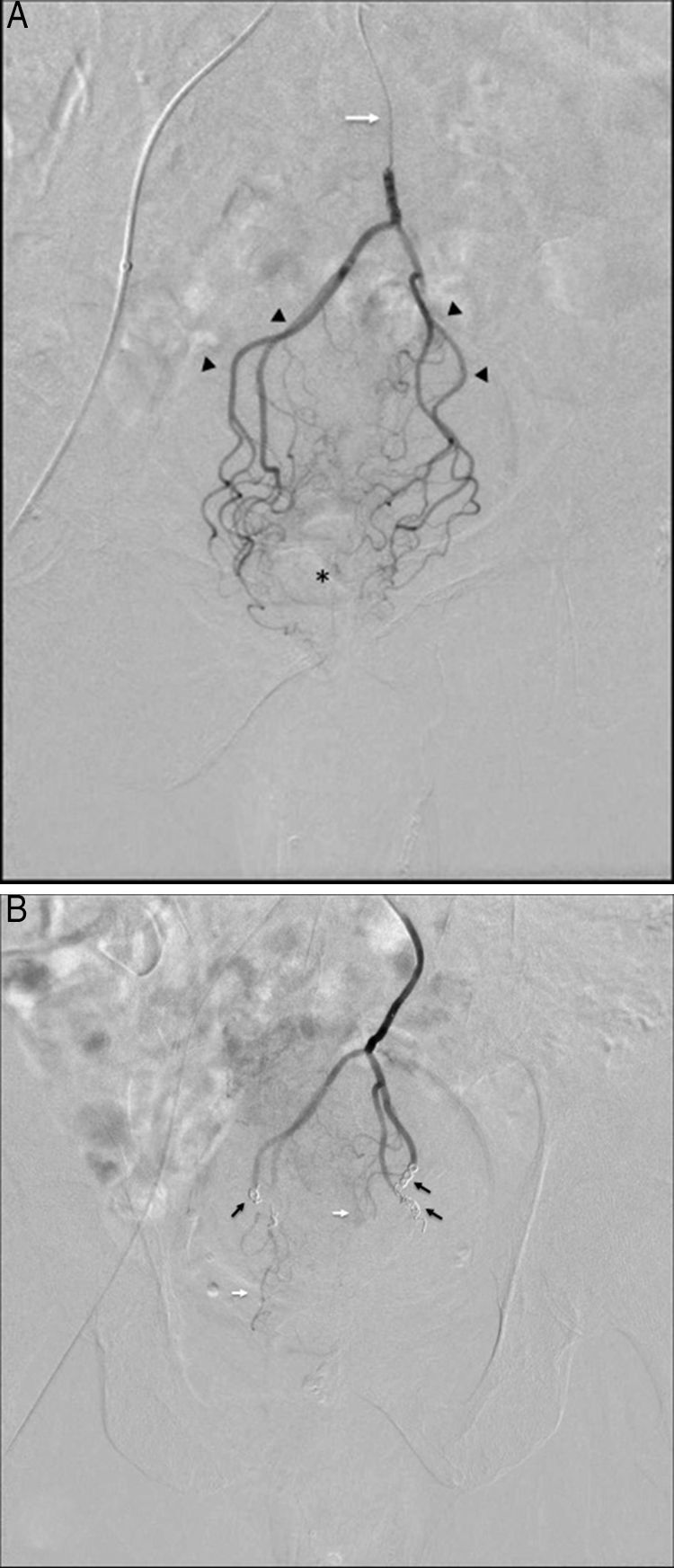
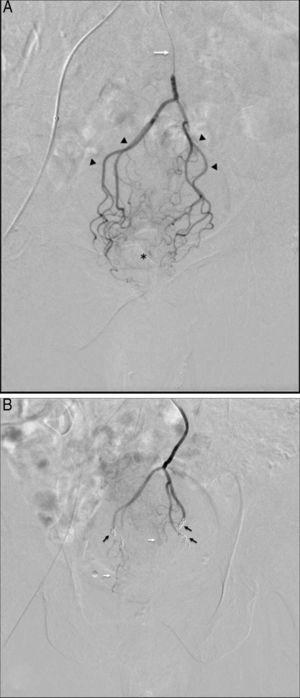
Before embolization, the 3 patients had almost daily episodes of bleeding after a bowel movement. We performed selective catheterization of the superior rectal artery with embolization of the anterior, posterior and right branches, using 0.018″ InterlockTM microcoils (Boston Scientific, USA). Fig. 1A and B show the pre- and post-embolization vascularization. The access was through the right common femoral artery. A local anesthetic, IV analgesia and conscious sedation were administered. The patients remained hospitalized for 24h. We conducted clinical follow-up during admission, at discharge and in the outpatient consultation until the 10th day. Pain was assessed using the visual analog scale (VAS), episodes of rectal bleeding and possible complications. Patients were reviewed in the outpatient surgery consultation 1, 3, and 6 months after the procedure, with clinical review and rectoscopy in cases of persistent symptoms.
(A) Selective digital subtraction arteriography via microcatheter (white arrow) at the beginning of the superior rectal artery, showing proximal branches (arrowheads) and small distal branches dependent on these arteries (asterisk); (B) post-embolization follow-up: note the absence of overall contrast uptake in the distal rectal territory after the release of the coils (black arrows) and small unobstructed remnant branches (white arrows), which help maintain sufficient blood flow to avoid ischemia.
The technical success was 100%. The branches of the superior rectal artery were correctly embolized in the 3 patients. In the evaluation of clinical success, which was defined as a significant decrease or disappearance of hemorrhoid symptoms, the results obtained were disparate during a follow-up of 3–6 months. In the first 10 days after the procedure, the 3 patients presented isolated rectal bleeding but no associated proctalgia (3–6 episodes of bleeding in first 10 days). When we assessed pain after the procedure, only patient 1 (CD) experienced discomfort (VAS 3) on the day of the embolization, which progressively diminished until disappearing completely on the 5th day. Patients 2 (UC) and 3 (UC and HIV+) did not experience any type of pain. No local inflammatory or ischemic complications were observed, nor did any complications appear at the femoral level. At the 1-month and 3-month evaluations, the first 2 patients reported a significant reduction in rectal bleeding episodes (less than one episode per week) and absence of prolapse. This evident clinical improvement was maintained during the subsequent follow-up.
At the 3-month follow-up visit, patient number 3 presented frequent episodes of rectal bleeding and associated prolapse, maintaining a clinical situation similar to before the procedure. Rigid rectoscopy showed that the rectal mucosa presented little or no inflammation, with the presence of engorged hemorrhoidal plexus and stigmata from bleeding, therefore re-embolization was indicated.
Our data do not allow us to draw conclusions. However, the Emborrhoid technique seems to be a safe alternative that achieves clinical improvement in patients (2/3) with IBD when surgery is not recommended. More studies and longer follow-ups are necessary to provide steadfast conclusions.
This study was presented as a poster at the Nacional Coloproctology Conference in 2016 after treating 2 cases.
Please cite this article as: Primo Romaguera V, Gregorio Hernández A, Andreo Hernández L, de la Morena Valenzuela E. Embolización selectiva de la arteria rectal superior, ¿alternativa a la cirugía hemorroidal? Cir Esp. 2018;96:239–241.