Breast cancer is the leading cause of cancer-related death in women. The American Cancer Society estimates that 40890 women will die of the disease within 2016 in the United States.1 Data of mortality from breast cancer has been improving over the past 25 years, mainly in relation to developments in early detection and better treatment.2 The estimated number of breast cancers diagnosed in Spain during 2014 was 26354; this number represented an adjusted rate to the European standard population of 85 per 100000 women.3 Breast cancer is heterogeneous disease, including different histological, immunological and molecular subtypes. Several studies have reported somatostatin receptors in primary breast cancers.4–7 We present the case of an unsuspected breast carcinoma with expression of somatostatin receptors diagnosed by imaging during the assessment of a hypertension study. Written informed consent for scientific use of the images was obtained from the patient.
A 46-year-old woman was referred to Nuclear Medicine Department with the suspicion of pheocromocytoma or paraganglioma. She had a 2-year history of resistant hypertension. Laboratory findings revealed increased urinary levels of norepinephrine 231μg/24h (normal range 15–80μg/24h) and vanillylmandelic acid 8.5mg/24h (normal range 2–8mg/24h), with normal serum levels of renin 10pg/ml (normal range 2–21pg/ml) and aldosterone 18ng/dl (normal range 2–23ng/ml). 123I-Metaiodobenzylguanidine whole-body scintigraphy showed a suboptimal image quality due to antihypertensive therapy. In this context, 111In-Pentetreotide scan was requested (Fig. 1). Whole-body and single photon emission computed tomography (SPECT) scans identified a focal pathological uptake in the left chest wall, although its exact location (breast or axilla) was not achieved. Left lateral thoracic planar image performed with the patient lying prone revealed the localization of the focal uptake in the breast tissue.
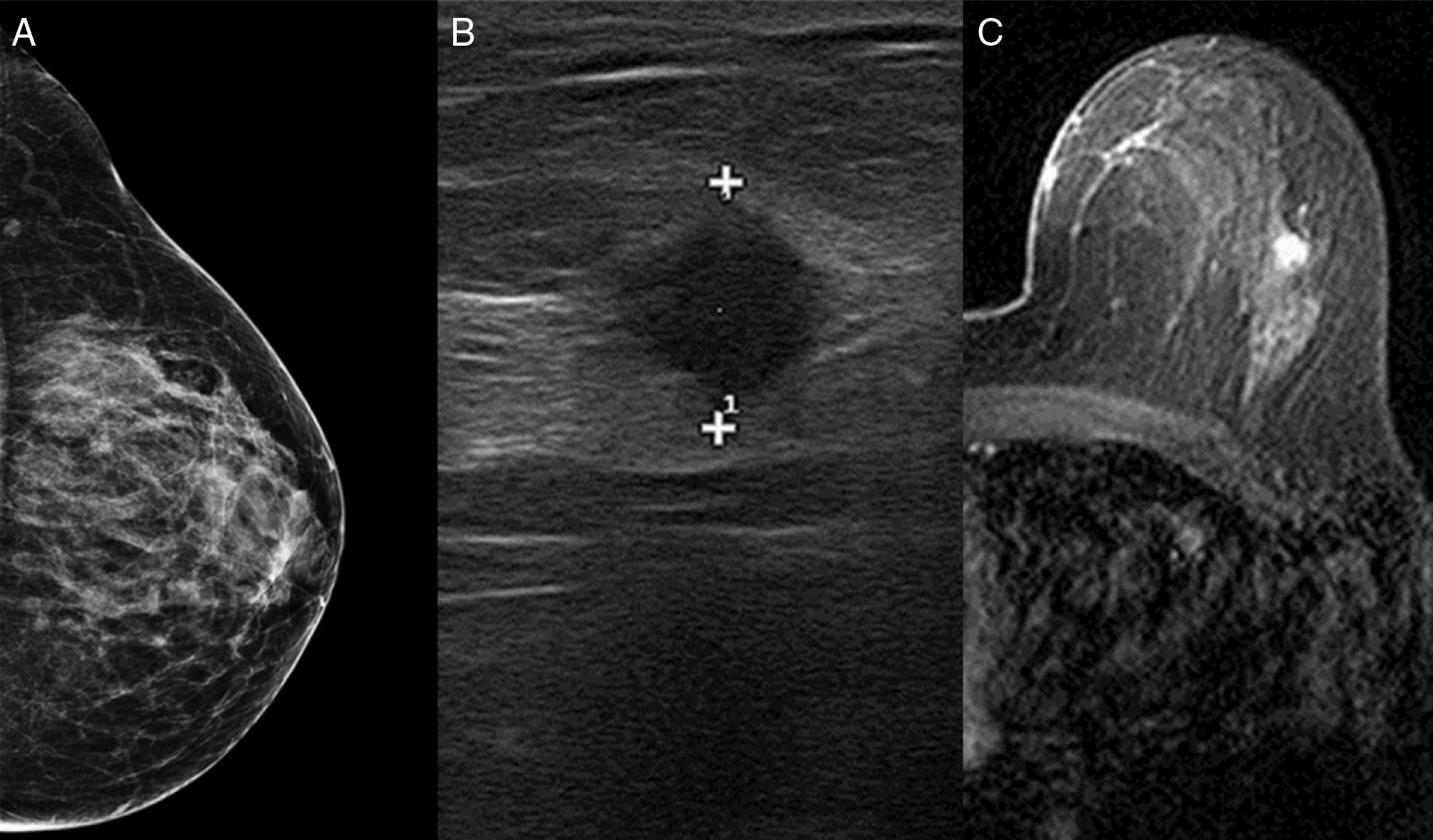
Physical examination was normal. Complementary imaging tests (Fig. 2) included mammography, ultrasound scan and magnetic resonance imaging (MRI). Mammography showed fibroglandular tissue, but focal mass was not detected. Ultrasound scan identified a hypo echoic and homogeneous nodule of 10mm in the left breast. MRI located the lesion at the upper-outer quadrant of the left breast, with kinetic malignant features. No other lesion was found. A large needle biopsy was performed. Histological result revealed ductal carcinoma, ER+++, PR+++, Cadherine-E+++, Ki-67 10% and Her-2+.
The patient underwent left lumpectomy and sentinel lymph node biopsy. After a concentric incision around areola in upper-outer quadrant, an excision of tissue with wire-guided localization was performed. Specimen size was 6×6×3cm in its length×width×height. Distance from closet margin was 5mm. Two sentinel lymph nodes were removed at axilla level II. Final pathological analysis reported an invasive ductal carcinoma of 0.8mm, Grade 1 (tubule formation, score 2; nuclear pleomorphism, score 2; mitotic count, score 1). No vascular, lymphatic or perineural invasion was observed. Immunohistochemical staining of the tumor cells were positive for neuroendocrine proteins chromogranin and synaptophysin. The two-sentinel lymph node were negative for metastases. Adjuvant hormonotherapy with Tamoxifen and radiotherapy (48Gy, with boost to the tumor bed) was also administered with good tolerance. After 9 months, she continues on treatment with Tamoxifen (20mg/24h). There is no clinical evidence of recurrence. Hypertension has been controlled with Spironolactone 25mg/48h; Amlodipine+Valsartan 10/160mg/24h; Bisoprolol 2.5mg/12h.
111In-Pentetreotide scintigraphy allows study in vivo of the presence of somatostatin receptors, mainly subtype 2, but also subtype 5. Somatostatin receptors are frequently expressed in breast cancer compared to normal breast tissue.4,5,8 Reubi et al. demonstrated somatostatin receptors in 46% of breast cancer tissues analyzed by in vitro autoradiography.6 This incidence was even higher (74%) in a series of 52 primary breast carcinomas reported by van Eijck et al, who used somatostatin receptor imaging.4 In other report, Bajc et al. found a higher incidence of somatostatin receptors in patients with breast cancer than in controls, and detected all ductal breast carcinomas greater than 20mm in size studied with 111In-Pentetreotide scan.5
Among the 5 subtypes of somatostatin receptors, the subtype 2 is predominant in breast cancer. A correlation between the tumor grade and the expression of somatostatin receptor 2 has been indicated by Orlando at al.7 These authors found that breast cancers expressing an up regulation of somatostatin receptor 2 mRNA may have a better prognosis. The presence of somatostatin receptor 2 has been also correlated with estrogen and progesterone levels.9 Frati et al.10 reported also a correlation between expression of somatostatin receptors subtype 2 and subtype 4 with luminal breast cancer, but not with triple negative or HER2 tumor marker.
We considered that the present clinical case is relevant in different aspects. First, the management of the breast lesion initially detected on somatostatin receptor imaging led up to early diagnosis of breast cancer in an asymptomatic patient from the breast point of view. Lesion size and somatostatin receptors density would be determining factors for the breast cancer imaging with somatostatin scintigraphy.8 Second, as the tumor was positive on 111In-Pentetreotide imaging, an indicator of somatostatin receptors expression, the surgical specimen was immunohistochemically tested to search neuroendocrine markers. This procedure is not routinely performed in invasive breast carcinomas. Third, the patient might benefit from treatment with somatostatin analogs, although the clinical studies still have to demonstrate the effectiveness of the use of such therapy in breast cancer patients.
Please cite this article as: Gómez-de la Fuente F-J, Jiménez-Bonilla J, Estévez J, Martínez-Rodríguez I, Banzo I. Expresión de receptores de somatostatina en cáncer de mama. Cir Esp. 2017;95:545–547.






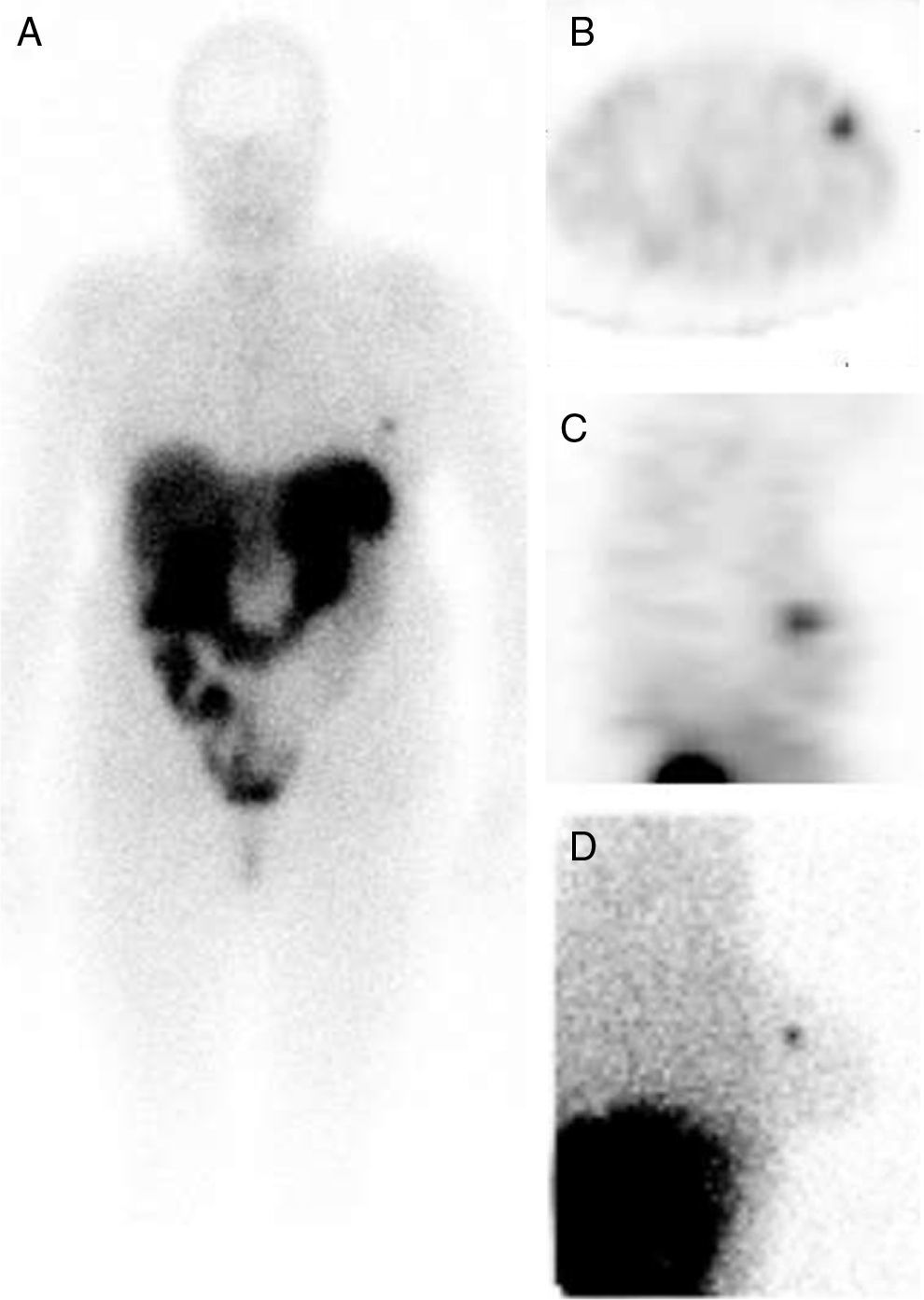
![Whole-body (A), SPECT (axial view [B], sagittal view [C]) and left lateral planar in prone position (D) images identified a focal increased uptake in the left breast. Whole-body (A), SPECT (axial view [B], sagittal view [C]) and left lateral planar in prone position (D) images identified a focal increased uptake in the left breast.](https://static.elsevier.es/multimedia/21735077/0000009500000009/v1_201712020521/S2173507717300704/v1_201712020521/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)