Descending necrotizing mediastinitis (DNM) is a serious infection which occurs as a complication of oropharyngeal infection. Its surgical management and the routine transthoracic approach remain controversial. In this article we report our experience in the management of this disease, and review the different surgical approaches that have been reported in the medical literature.
Materials and methodsA retrospective review of the clinical records of 29 patients treated between 1988 and 2009 was made. Several demographic variables were analyzed, origin of the initial infection, stage of the disease according to Endo's classification, surgical technique and outcome.
ResultsSurgical treatment consisted of both cervical and mediastinal drainage and radical debridement. The mediastinal drainage was made through a transcervical approach in 10 cases and transthoracic in 19, depending on the extent of the mediastinitis. The outcome was satisfactory in 24 patients and 5 died (mortality 17.2%).
ConclusionsAccording to our results and the conclusions of the main authors, we recommend a prompt and aggressive surgery with a transthoracic approach in cases of widespread DNM.
La mediastinitis necrosante descendente (MND) consiste en una infección grave que aparece como complicación de una infección orofaríngea. Aún existe controversia a propósito del tratamiento quirúrgico y si está indicado un abordaje transtorácico rutinario. En este artículo presentamos nuestra experiencia en el tratamiento de la mediastinitis necrosante descendente y revisamos en la bibliografía las diferentes opciones de abordaje propuestas.
Material y métodosEstudio observacional retrospectivo de los pacientes con mediastinitis necrosante descendente intervenidos entre 1988 y 2009. Se analizan variables demográficas, origen de la infección, estadio de la enfermedad según la clasificación de Endo, técnica quirúrgica realizada y evolución.
ResultadosEn dicho periodo se intervino a 29 pacientes. El tratamiento quirúrgico consistióen el drenaje y desbridamiento radical a nivel cervical y mediastínico. El drenaje mediastínico se realizópor vía transcervical en 10 casos y transtorácica en 19, en función de la extensión de la mediastinitis. De ellos, 24 presentaron buena evolución y 5 fallecieron (mortalidad 17,2%).
ConclusionesDe acuerdo con nuestros resultados y las conclusiones de los principales autores, se debe realizar un tratamiento quirúrgico precoz y agresivo que incluya un abordaje transtorácico en casos de mediastinitis extendida.
Descending necrotizing mediastinitis (DNM) is considered one of the most aggressive forms of mediastinitis. It is a serious infection of the mediastinal connective tissue that appears as a complication of an oropharyngeal or dental infection. This infection spreads through the cervical anatomic spaces to the mediastinum, favored by negative intrathoracic pressure and gravity. The diagnostic criteria defined by Estrera et al. in 19831 include the following: (1) clinical manifestation of severe infection; (2) radiological abnormalities characteristic of the disease; (3) surgical or post-mortem evidence of descending necrotizing mediastinitis; (4) correlation between oropharyngeal infection and the development of DNM. Despite being uncommon, it is a relevant disease in thoracic surgery and for all those professionals involved due to its high mortality (which can reach 40%2) and because our actions can have a decisive influence on the clinical course of patients with this pathology. Delayed diagnosis and inappropriate or insufficient mediastinal drainage are considered the main factors influencing mortality.3 The objective of this study is to show our experience in the surgical treatment of this disease and to describe the surgical technique and results.
Materials and MethodsWe present a retrospective, descriptive study of all the cases of DNM that were diagnosed and treated in our department between January 1988 and February 2009. All cases met the criteria by Estrera et al.1 for the diagnosis of this disease, as mentioned above. Excluded from the study were those patients who had acute mediastinitis secondary to other causes, such as infections after mid-sternotomy or after esophageal rupture. We analyzed demographic variables, disease period, origin of infection, disease stage according to the Endo classification, surgical technique performed and evolution, assessing survival and the appearance of complications. A descriptive study was performed with the SPSS v15 statistical package.
Diagnosis was based on symptoms, radiographic findings seen on computed tomography (CT) scan and histopathological findings. All patients underwent cervico-thoracic CT, which revealed infiltration of the mediastinal fat with the formation of abscesses and, occasionally, gas bubbles (Fig. 1). The extension of mediastinal involvement was also evaluated by CT scan. We used the classification proposed by Endo et al.4: stage I when only the superior mediastinum is affected; stage IIA when there is involvement below the carina but only of the anterior mediastinum; and, stage IIB when the posterior mediastinum is also affected.
Given the suspected diagnosis, broad-spectrum antibiotic therapy was started and surgical treatment was performed urgently together with specialists from either the Maxillofacial Surgery or Otolaryngology departments, depending on the dental or cervical origin of the infection. In all cases, collar cervicotomy was performed for cervical drainage, which entailed opening all the involved cervical spaces and draining and debriding the necrotic tissue. For the mediastinal drainage, the chosen approach depended on the extension of the mediastinitis. In cases where there was only involvement above the carina, mediastinal drainage was performed transcervically. In cases with subcarinal involvement, some type of thoracic approach was used. In the early years of the series, a median sternotomy was used, and in more recent years posterolateral thoracotomy, which is especially indicated in cases of posterior mediastinal involvement. In certain cases with affected anterior mediastinum alone, debridement was performed through the cervicotomy with the help of a subxiphoid incision.
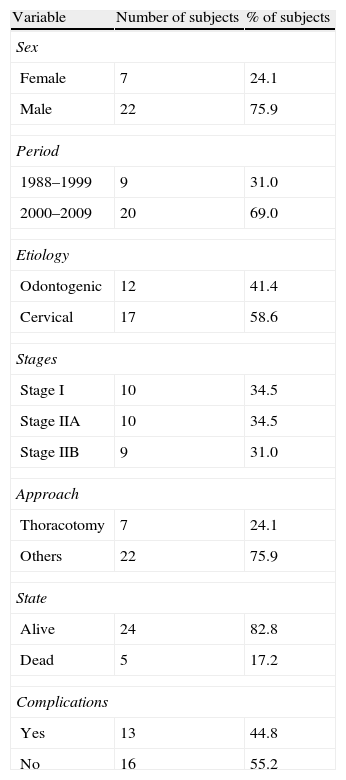
ResultsIn the period between January 1988 and February 2009, we treated 29 patients diagnosed with DNM. The results of the descriptive analysis are shown in Table 1. Mean age was 41.38 years (range 18–76), and 22 patients were males. The origin of the infection was odontogenic in 12 cases and pharyngeal in 17. CT images demonstrated that in 10 cases there was only involvement above the carina, while 19 patients had subcarinal extension. Nine of these patients also had involvement of the posterior mediastinum. In accordance with the classification by Endo et al., 10 patients were in stage I, 10 in stage IIA and 9 in stage IIB.
Descriptive Analysis of Qualitative Variables.
| Variable | Number of subjects | % of subjects |
| Sex | ||
| Female | 7 | 24.1 |
| Male | 22 | 75.9 |
| Period | ||
| 1988–1999 | 9 | 31.0 |
| 2000–2009 | 20 | 69.0 |
| Etiology | ||
| Odontogenic | 12 | 41.4 |
| Cervical | 17 | 58.6 |
| Stages | ||
| Stage I | 10 | 34.5 |
| Stage IIA | 10 | 34.5 |
| Stage IIB | 9 | 31.0 |
| Approach | ||
| Thoracotomy | 7 | 24.1 |
| Others | 22 | 75.9 |
| State | ||
| Alive | 24 | 82.8 |
| Dead | 5 | 17.2 |
| Complications | ||
| Yes | 13 | 44.8 |
| No | 16 | 55.2 |
Surgical treatment included a cervical and thoracic approach in 19 cases, and only cervical in 10. First of all, the tooth causing the odontogenic infection was extracted or the peritonsillar abscess was drained. This procedure had been previously performed at another medical center in 12 cases. In all cases, bilateral collar cervicotomy was performed, leaving 2–4 cervical drains. Tracheostomy was performed in 13 patients: 10 of them in the same intervention due to airway compression, and 3 after prolonged patient intubation in the ICU. Mediastinal drainage was carried out through the cervicotomy in 10 cases, by means of cervicotomy and subxiphoid incision in 3, by median sternotomy in 9 and by posterolateral thoracotomy in 7 cases (4 right and 3 left). Between one and five chest drains were used, distributed between the mediastinum and thoracic cavity. In cases where purulent discharge persisted after surgery, mediastinopleural irrigation was done with infusion of saline solution through the drains one or two times per day.
Two reoperations were necessary. One was due to progression of mediastinitis in a patient who was initially treated with cervicotomy, and right posterolateral thoracotomy was performed on the 4th day post-op. In another case, it was necessary to perform debridement of cellulitis of the upper right thoracic wall that the patient developed on the 3rd day post-op.
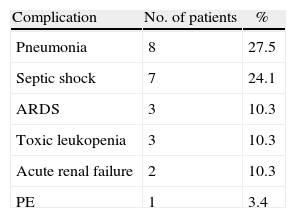
Complications appeared in 44.8% of the cases, the most frequent of which were septic shock and pneumonia (Table 2). Mortality was 17.2% (5 patients). The causes were septic shock in 3 cases, acute renal failure in one case and massive pulmonary thromboembolism in one case. Three cases were stage IIB and 2 were stage I.
If we analyze mortality by time periods, until 1999 it was 30%, which then dropped to 10% between the year 2000 and the end of the series. In this last period, thoracotomy was performed in all cases with suspected subcarinal mediastinum involvement.
DiscussionIn cases of suspected diagnosis of DNM, wide-spectrum antibiotic therapy must be initiated immediately along with appropriate life support measures, requiring admittance of the patients to the ICU in most cases. However, any measures will be insufficient if early surgical treatment is not performed to extensively debride both the cervical and mediastinal regions. Our department has been able to reduce mortality due to this disease by using multidisciplinary treatment with a surgical approach that includes thoracotomy in all cases with subcarinal involvement.
Multiple options for mediastinal drainage have been proposed in the literature, and there is still controversy about the best approach and whether or not a routine transthoracic approach is necessary. If we analyze the historical evolution, up until the 1980s mediastinal drainage was basically performed transcervically. With cervicotomy, we can approach the mediastinum through the pre-tracheal space and, with digital dissection, reach the carina.
The first important study about DNM was published by Pearse5 in 1938; it reported an overall mortality of 55% that was even higher for patients who had been treated surgically. In the antibiotic era, Estrera et al.1 published a series in 1983 of 10 patients with a mortality of 40%; these authors indicated the need for a thoracic approach in cases of mediastinal involvement below the 4th thoracic vertebra or below the carina. Along these lines, Wheatley et al.6 reviewed the literature in 1990 and observed that cervical drainage had been insufficient in 79% of patients; they therefore proposed a subxiphoid approach as a possible alternative for draining the anterior mediastinum.
In the 1990s, more and more authors defended the need for transthoracic drainage and proposed thoracotomy as the ideal approach because it provides the best access to all the mediastinal compartments, allowing for radical surgical debridement as well as the drainage of possible pleural or pericardial collections and proper placement of any chest tubes that may be required. Marty-Ane, Freeman and Corsten3,7,8 proposed thoracotomy as the best approach, regardless of the extension of mediastinitis. Corsten8 also performed a meta-analysis of 36 studies with 69 patients and found statistically significant differences in the survival of patients treated with only the transcervical approach (which was 53%) compared with those treated with a thoracic approach (81%).
Other alternative approaches to thoracotomy have been proposed for mediastinal drainage, such as median sternotomy or clamshell incision.9,10 Their advantage is that with a single incision the mediastinum and both pleural cavities can be accessed, but because of the risk of sternal dehiscence and osteomyelitis, these techniques have ceased to be widely used. Another proposed surgical approach is video-assisted thoracoscopy, which would provide the benefits of minimally invasive surgery.
Most published studies, however, include one or just a few cases. The largest published series includes 17 cases and it reported conversion to thoracotomy in 2 cases due to uncontrollable bleeding.11 The authors themselves recommend thoracotomy in cases of severe inflammation and reserve video-assisted thoracotomy for cases with little anatomic distortion. More studies are probably necessary to determine the role of video-assisted thoracoscopy; meanwhile, most authors continue to defend thoracotomy as the best approach for mediastinal debridement, although it might not be really necessary in all cases.
In 1999, Endo et al.4 created a mediastinitis classification based on extension: in stage I, only the superior mediastinum is affected; in stage IIA, there is involvement below the carina but only of the anterior mediastinum; and stage IIB is when the posterior mediastinum is also affected. According to the conclusions of this author, transcervical drainage would be sufficient in stage I, in stage IIA the mediastinum could be drained through a subxiphoid incision, and in stage IIB thoracotomy should be performed in all cases.
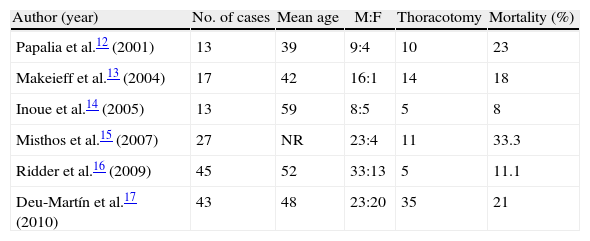
Table 3 shows some of the largest series published in the last decade. For most authors, the approach depends on the extent. Some authors, as in our case, use the Endo et al. classification. Others differentiate between localized and extended mediastinitis in terms of whether or not there is involvement below the carina. In cases of extended mediastinitis, thoracotomy is recommended, preferably on right side. According to the conclusions of these studies, the most important factors that will influence mortality are delayed diagnosis and insufficient or inadequate mediastinal drainage. Some authors also point out the importance of the medical history of the patient, especially immunosuppression, such as AIDS or diabetes, as risk factors for the development of mediastinitis and a poor outcome.18 In the series published by Deu-Martín et al. including 43 patients, potential predictors of mortality were evaluated, including diabetes mellitus and comorbidity, among others. Only the presence of septic shock proved to be an independent predictor of mortality in the multivariate analysis.17,19
Mortality in Historical Series.
| Author (year) | No. of cases | Mean age | M:F | Thoracotomy | Mortality (%) |
| Papalia et al.12 (2001) | 13 | 39 | 9:4 | 10 | 23 |
| Makeieff et al.13 (2004) | 17 | 42 | 16:1 | 14 | 18 |
| Inoue et al.14 (2005) | 13 | 59 | 8:5 | 5 | 8 |
| Misthos et al.15 (2007) | 27 | NR | 23:4 | 11 | 33.3 |
| Ridder et al.16 (2009) | 45 | 52 | 33:13 | 5 | 11.1 |
| Deu-Martín et al.17 (2010) | 43 | 48 | 23:20 | 35 | 21 |
NR: no recorded in the study; M:F=males:females.
For the reasons above, we conclude that DNM continues to be an aggressive and sometimes lethal disease, even though mortality rates of 40% no longer apply as they have been reduced to 15.5% in last decade.16 Early diagnosis and treatment by a multidisciplinary team are essential, which should include aggressive surgical treatment, taking into account the extension of the disease and the clinical condition of each patient. Last of all, in cases of extended mediastinitis, a transthoracic approach is recommended.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Bayarri Lara CI, Sevilla López S, Sánchez-Palencia Ramos A, Alkourdi Martínez A, Hernández Escobar F, Quero Valenzuela F, et al. Tratamiento quirúrgico de la mediastinitis necrosante descendente. Cir Esp. 2013;91:579–583.