The aim of this study is to demonstrate our experience at a volunteer surgical program in Cameroon, which is of special interest given to the inability to adopt international treatment guidelines for thyroid surgery in areas of limited resources due to the lack of preoperative testing and to the difficulty to obtain sustitutive hormonal treatment.
MethodsThis is a prospective observational study that includes 16 cases of thyroid surgery in Dschang (Cameroon) during June 2015. The patients were previously selected by a local medical team. All patients were black, 15 women and one man, with a mean age of 41 years. The surgical technique used for the removal of unilateral disease was hemithyroidectomy with isthmectomy and bilateral subtotal thyroidectomy for bilateral disease.
ResultsFive subtotal thyroidectomies, 9 hemithyroidectomies and 2 isthmectomies were performed. Prethyroid muscles were divided only in one case. We visualized 86% of the parathyroid glands and 84% of the recurrent laryngeal nerves. The main complications observed were one symptomatic cervical hematoma that required reoperation and 2 surgical wound infections. There were no clinical episodes of hypocalemia or recurrent nerve lesion. The mean length of stay was 2.3 days. At follow-up, all bilateral thyroidectomies developed high TSH levels.
ConclusionsThyroid surgery is safe in developing countries adopting protocols and techniques we use in our environment (avoiding total thyroidectomy). Bilateral thyroidectomies should not be performed unless functional studies are available in the follow-up and a thyroid hormone supplement stock guaranteed whenever necessary.
Nuestro objetivo es describir la experiencia adquirida en un programa de cooperación dedicado a la cirugía tiroidea en Camerún. Su interés radica en la imposibilidad para seguir las guías internacionales de tratamiento en áreas de recursos imitados debido a la falta de estudios preoperatorios y a la dificultad para conseguir medicación hormonal sustitutiva de por vida.
MétodosEstudio observacional de una cohorte de 16 pacientes operados de enfermedad tiroidea en Dschang (Camerún) en junio de 2015. La técnica quirúrgica empleada fue la hemitiroidectomía con istmectomía en la enfermedad unilateral y la tiroidectomía subtotal bilateral en la enfermedad bilateral.
ResultadosTodos los pacientes eran de raza negra, 15 mujeres y un hombre, con edad media de 41 años. Se realizaron 5tiroidectomías subtotales, 9hemitiroidectomías y 2istmectomías. Cuatro pacientes presentaban componente intratorácico. Fue necesaria la sección de músculos pretiroideos en un caso. Se visualizaron las glándulas paratiroides y los nervios laríngeos recurrentes en el 86 y el 84% de los casos, respectivamente. Se dejaron drenajes en 7 casos y la mediana de duración de la intervención fue de 75min. Como complicaciones cabe destacar un hematoma cervical que precisó reintervención y 2infecciones de herida quirúrgica. No hubo hipocalcemias clínicas ni lesiones recurrenciales apreciables. La estancia media fue de 2,3 días. A largo plazo, los pacientes con tiroidectomías bilaterales presentaban niveles elevados de TSH.
ConclusionesLa cirugía tiroidea en países subdesarrollados, adaptando los protocolos y técnicas que utilizamos en nuestro medio (evitando la tiroidectomía total), tiene una tasa de complicaciones asumible. No deben realizarse tiroidectomías bilaterales salvo que se disponga de estudios funcionales y se asegure previamente la disponibilidad de la hormona tiroidea.
The World Health Organization (OMS) estimates that 43% of the African population has iodine deficiency,1 which, together with other typical goitrogenic factors of African diets (cyanogenic glycosides in cassava, thiocyanate, selenium deficiency)2,3 make goiter an endemic problem.
In Cameroon, which is 152nd out of the 187 countries classified in order of their Human Development Index according to the United Nations Program for Development report from 2014,4 there is a series of circumstances that influence the practice of thyroid surgery.
In these areas of limited resources, this type of surgery is quite a logistical challenge. It is impossible to conduct proper preoperative studies, which makes it difficult to comply with the recommendations of international treatment guidelines.5 Hence, we surgeons must adapt our methods to the circumstances. Furthermore, the difficult access to medication in cases where thyroidectomy causes sequelae (hypothyroidism, hypocalcemia) can convert thyroid surgery into a potentially dangerous surgical intervention.
A large part of the sub-Saharan African population has absolutely no possible access to this type of surgery in their countries due to the exorbitant cost compared to the income levels of this region.6 Healthcare cooperation surgical programs provide one of the few possibilities for treatment.7,8 However, participating surgeons frequently express reticence to perform thyroidectomies due to the lack of adequate preoperative testing and the possible development of serious complications, which are easily treated in the Western world but are difficult to resolve in these countries given the lack of resources.
The objective of this study is to describe the results of a series of thyroidectomies performed in Cameroon through a healthcare cooperation program. The article will explain the peculiar adaptations necessary in both the therapeutic approach and technique in order to conduct as many surgical interventions as possible and minimize postoperative complications.
MethodsWe analyzed a cohort of 16 patients treated by thyroid surgery during a program carried out in Dschang, western Cameroon, in the month of June 2015, specifically at the Notre Dame de la Sante Hospital run by the Hermanas Siervas de María religious congregation.
The expedition included 2 anesthetists, 2 experienced surgeons and 3 surgical residents, 2 pre-residency medical students and a pediatrician. The surgical activity took place over the period of 4 days. The patients with significant goiter had been previously selected by 2 Cameroonian physicians working at the hospital, who were also responsible for the patients’ long-term control. The first day was spent in the consultation reviewing the cases selected and screening them a second time to finally select 17 patients (our only exclusion criteria were suspicion of uncontrolled hyperthyroidism or the need for lymphadenectomy given the suspicion for cancer).
Surgical intervention was not contraindicated in patients with giant goiter who, in fact, were half of the patients treated.
Three patients had recent hormone studies and, in all except 2, hormone studies were done before surgery. For all patients, HIV serology was available. None of the patients had preoperative calcemia. Only 4 patients had previous ultrasound studies; in the remainder, we performed the examinations ourselves with portable ultrasound equipment, with the consequent limitations due to our moderate level of ultrasound experience. We did not have advanced imaging techniques available, such as computed tomography or isotope analysis. None of the patients had undergone fine-needle aspiration; it was not possible to perform this test as there was no pathologist available.
We scheduled 17 thyroidectomies, although in the end only 16 patients were treated because orotracheal intubation was not possible in one case. All patients signed an informed consent form that was specifically designed for our campaign.
All the patients were operated on with orotracheal intubation and under balanced anesthesia with intravenous propofol, anectine, fentanyl and rocuronium as well as inhaled oxygen, protoxide and isoflurane. Prophylactic dexamethasone was administered to all patients, and antibiotic therapy was given selectively (giant goiter, prolonged surgeries). As for the surgical technique, for cases with unilateral disease, hemithyroidectomy was planned of the side affected with isthmectomy. For cases of bilateral disease, subtotal thyroidectomy was planned for both sides in order to minimize the risk for parathyroid and recurrent nerve injury, and a thyroid remnant of 4–5g was left on each side in order to avoid life-long hormone replacement therapy. In patients with a clearly affected lobe and uncertain contralateral involvement (large goiters where one side greatly surpasses the midline), the decision was deferred until surgery and after having explored the less affected side; unilateral resection was preferred, providing the involvement of the remaining side was minimal. After surgery, the patients were transferred to a unit with continuous monitoring by nursing staff: Trousseau was done on each shift and calcemia was analyzed after 24h. Pathology studies of the surgical specimens were not possible.
Data for the following variables were collected:
- -
Preoperative: age, sex, laterality, goiter size, T4, TSH and HIV status.
- -
Intraoperative: surgical technique, visualization of parathyroid glands and recurrent laryngeal nerve, drain tubes and duration of the operation.
- -
Immediate post-op: hemorrhage, dysphonia and hypocalcemia.
- -
Late post-op: permanent dysphonia, permanent hypocalcemia, hypothyroidism.
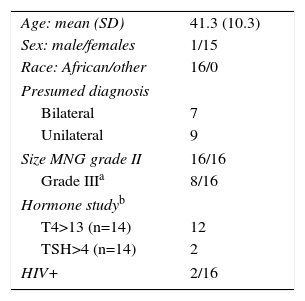
Table 1 shows the demographic data of the series. The suspected diagnosis was bilateral goiter in 7 cases and unilateral goiter in 9 (all nodules >4cm), based on clinical examination (elastic consistency, absence of palpable cervical lymphadenopathies) and ultrasound (no calcifications, no nodules with irregular edges or intranodular vascular spots). Pathology studies of the specimens were not possible due to lack of resources; therefore, there was no histological confirmation and cancer could not be ruled out.
All nodules were larger than 4cm, and all goiters were grade II according to the 1994 classification of the WHO (visible thyroid gland with the neck in normal position), although 8 would have been grade III according to the 1960 classification (goiter visible at a distance) (Fig. 1).
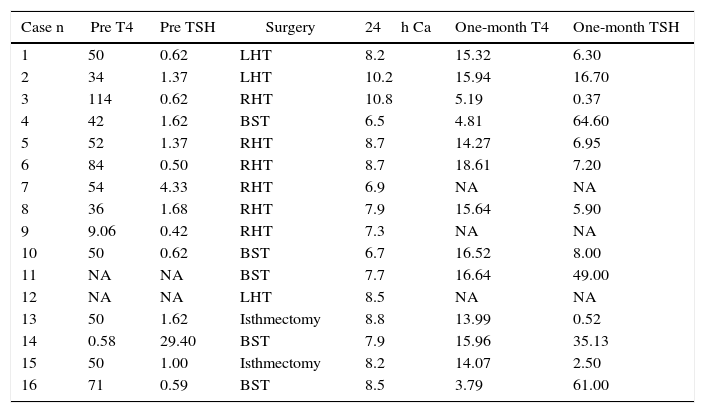
Only one case of the 14 in which hormone studies were available presented low T4 with elevated TSH (case 14). The remainder had strikingly elevated levels (between 34 and 114mU/L) of T4 (except case 9: 9.06) with normal TSH (except case 7 with minimal elevation; 4.3) (Table 2).
Pre- and Postoperative Hormone Study; 24h Calcemia.
| Case n | Pre T4 | Pre TSH | Surgery | 24h Ca | One-month T4 | One-month TSH |
|---|---|---|---|---|---|---|
| 1 | 50 | 0.62 | LHT | 8.2 | 15.32 | 6.30 |
| 2 | 34 | 1.37 | LHT | 10.2 | 15.94 | 16.70 |
| 3 | 114 | 0.62 | RHT | 10.8 | 5.19 | 0.37 |
| 4 | 42 | 1.62 | BST | 6.5 | 4.81 | 64.60 |
| 5 | 52 | 1.37 | RHT | 8.7 | 14.27 | 6.95 |
| 6 | 84 | 0.50 | RHT | 8.7 | 18.61 | 7.20 |
| 7 | 54 | 4.33 | RHT | 6.9 | NA | NA |
| 8 | 36 | 1.68 | RHT | 7.9 | 15.64 | 5.90 |
| 9 | 9.06 | 0.42 | RHT | 7.3 | NA | NA |
| 10 | 50 | 0.62 | BST | 6.7 | 16.52 | 8.00 |
| 11 | NA | NA | BST | 7.7 | 16.64 | 49.00 |
| 12 | NA | NA | LHT | 8.5 | NA | NA |
| 13 | 50 | 1.62 | Isthmectomy | 8.8 | 13.99 | 0.52 |
| 14 | 0.58 | 29.40 | BST | 7.9 | 15.96 | 35.13 |
| 15 | 50 | 1.00 | Isthmectomy | 8.2 | 14.07 | 2.50 |
| 16 | 71 | 0.59 | BST | 8.5 | 3.79 | 61.00 |
LHT, left hemithyroidectomy; RHT, right hemithyroidectomy; NA, not available; BST, bilateral subtotal thyroidectomy.
Normal values: T4: 5.0–13.0μg/dL; TSH: 0.4–4.0mIU/L.
As for surgical technique, we had planned for 7 bilateral subtotal thyroidectomies (BST), 7 hemithyroidectomies (HT) and 2 isthmectomies. However, given the intraoperative findings, the techniques that were finally done were as follows: 5 BST, 9 hemithyroidectomies and 2 isthmectomies (both cases with a 4cm central nodule and 2normal lobes). It should be mentioned that 3 of the cases with preoperative diagnosis of apparently bilateral giant goiter planned for BST (cases 2, 6 and 12) were found to be unilateral during surgical exploration and after having freed the massive growths from one side that greatly surpassed the midline over the trachea; these masses were also compressing and displacing the trachea laterally while hiding normal-appearing contralateral lobes. In all these cases, hemithyroidectomy was done of the affected side, minimizing risks. In contrast, one apparently unilateral giant case was in effect bilateral and required BST.
It was only necessary to divide the pre-thyroid muscles in one of these cases of massive right goiter. The growth of the nodules was excentric in most cases, with cervical masses that were enormous in size in half of the patients treated (8 cases). In only 4 of these patients did we observe moderate retrosternal growth.
Out of the 38 potentially locatable parathyroid glands (2 in hemithyroidectomies [2×9=18] and 4 in BST [4×5=20]), 33 were presumably visualized (86%): 17/19 (89%) superior parathyroid and 16/19 (84%) of the inferior parathyroid glands. The ipsilateral recurrent laryngeal nerve was visualized in all the hemithyroidectomies. In the bilateral surgeries, 7/10 of the potentially locatable recurrent laryngeal nerves were able to be visualized. In the 2 isthmectomies, nerve dissection was not attempted.
Suction drains were selectively used (7/16) in cases of large-size goiters to help collapse the residual cavity. The median (IQR) duration of the interventions was 75 (68.7) min (range 40–180).
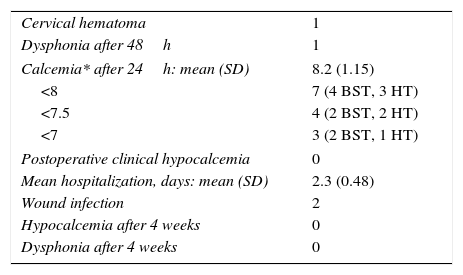
Table 3 shows the postoperative complications of the series. One patient who underwent BST the day before the end of the campaign was reoperated 12h later under sedation after having developed progressive occupation of the wound. Re-exploration was considered necessary because the surgical team was soon leaving the country, even though there was no suffocating hematoma (case 14). The patient did not have drain tubes. We evacuated a moderate hematoma and ligated a minimal blood vessel that was actively bleeding.
Complications (n=16).
| Cervical hematoma | 1 |
| Dysphonia after 48h | 1 |
| Calcemia* after 24h: mean (SD) | 8.2 (1.15) |
| <8 | 7 (4 BST, 3 HT) |
| <7.5 | 4 (2 BST, 2 HT) |
| <7 | 3 (2 BST, 1 HT) |
| Postoperative clinical hypocalcemia | 0 |
| Mean hospitalization, days: mean (SD) | 2.3 (0.48) |
| Wound infection | 2 |
| Hypocalcemia after 4 weeks | 0 |
| Dysphonia after 4 weeks | 0 |
HT, hemithyroidectomy; BST, bilateral subtotal thyroidectomy.
*Normal calcemia values 8.5–10.5mg/dL.
Mild dysphonia (hoarseness) was observed during the first 48h in one patient who completely recovered on the third day post-op, so it is not cataloged as a recurrent lesion (with the bias of not being able to evaluate more than the vocal alteration).
Although the calcemia obtained after 24h was frequently low (<8mg/dL and 7/16 patients: 3/9 hemithyroidectomies and 4/5 BST), and even <7mg/dL in 3 cases, no patients presented signs of hypocalcemia. As we did not have preoperative calcemia results or levels of ionic calcium or albumin to correct calcium levels, we decided to dismiss treatment in these patients, who progressed without developing any symptoms. Therefore, there was no need for calcium replacement.
Mean hospital stay was 2.3 days. Two patients were re-hospitalized due to purulent exudation after the accumulation of seroma.
Postoperative hormone studies are available for 13 of our patients, done 4 weeks after surgery (Table 2). T4 was slightly below normal levels in 2 patients, within normal range (5.0–13.0μg/dL) in one and slightly elevated (between 13.4 and 18.6) in the remainder, even in the patient who presented low T4 before surgery, but with levels that were far below preoperative levels. TSH was minimally low in one patient (0.37 in case 3=RHT), normal (0.4–4 mU/L) in 2 patients (the 2 isthmectomies, cases 13 and 15), slightly elevated (<10mU/L) in 5 patients (4 HT and one BST) and very elevated (>10mU/L) in another 5 (one HT and 4 BST). In 3 of these 5 latter patients (all BST), with TSH>40, including the 2 single cases with low T4, hormone treatment was initiated even though the patients were asymptomatic. The other 2 cases with TSH>10 maintain high levels of T4 and moderately elevated TSH.
DiscussionCameroon is a country that is not much smaller than Spain (475000 vs 505000km2), but it has half the population (23 vs 46 million inhabitants). Life expectancy is estimated at 54 in women and 51 in men, while the mortality rate in children <5years of age is 13.6%.9 The immense majority of the population cannot afford treatment for many diseases, as advanced technologies are only found in cities with large populations and are prohibitively expensive compared to the population's income levels.6 Thyroid surgery is not an exception and, therefore, medical cooperation campaigns are for many patients the only hope for surgical treatment.
Nonetheless, the possibility of developing permanent hypocalcemia or hypothyroidism, which can become fatal complications due to the difficulty in finding or financing replacement medication in this setting, make many surgeons reticent toward performing thyroid surgery in areas with such limited resources.
If advanced radiology techniques (CT) or cytological analysis of the nodules had been available, the indication for surgical treatment in all these cases would not have changed. If cancer had been suspected, total thyroidectomy would have been recommended, although hormone replacement would have to be ensured for life, assuming the difficulty (or impossibility) for later radioactive iodine scan or therapeutic doses.
Although we only performed 5 out of the 7 expected BST and these patients would have a real risk for developing hypocalcemia or hypothyroidism, the absence of hypocalcemia in the immediate postoperative period makes us believe that there would also be none in the future. The calcemias have very frequently been low (7/16), even in 3/9 (33%) cases of unilateral thyroidectomies, although no patients manifested clinical signs of hypocalcemia. We did not have preoperative calcium or albumin results (to verify whether they were also low) in order to correct their levels (presumably the population would have some degree of malnutrition that could explain the phenomenon). Other causes that could explain postoperative biochemical hypocalcemia could be, in addition to purely technical factors, hypomagnesemia, hypovitaminosis or functional hypoparathyroidism after stress or due to hyperthyroxinemia. For the former reasons, we decided to guide treatment according to symptoms, and calcium was not administered to any of the patients.
Hormone studies are difficult to interpret. The preoperative functional pattern seems to correspond with thyroid hormone resistance (very elevated T4 with unsuppressed TSH),10 although it does not seem reasonable to think that this rare genetic syndrome is present in such a high percentage of our patients. On the one hand, the incidence of this syndrome is not higher in Africa and, on the other, the reliability of the laboratory cannot be verified, and we also only have available total T4 levels measured by RIA, which present a level of interferences quite superior to those of free T4. As for thyroid function after 4 weeks, although T4 levels reduced to an important extent, they remained moderately elevated in 10 out of the 13 patients with hormone measurements after 4 weeks. Taking into account what has previously been reported about total T4 levels, we recommend guiding hormone replacement with TSH. We have found notable elevations (>10mU/L) in 4-week TSH in 4/5 BST, while this only happened in 1/9 hemithyroidectomies. Therefore, BST induced hypothyroidism in a very high percentage. Given the difficulties for obtaining hormone supplements, we have used very high TSH levels as a priority criterion for thyroid replacement and have given preference to women of child-bearing age (due to the severe consequences of hypothyroidism during pregnancy) or the existence of larger thyroid remains (to avoid the recurrence of goiter due to continuous stimulus). Thus, hormone therapy was initiated in the 3 patients with BST and TSH>40mU/L, including the only 2 cases with low T4 (the other case with moderate elevation), although none had evident symptoms of hypothyroidism. Therefore, we do not recommend performing any type of bilateral thyroidectomy if there is no possibility to monitor and substitute hormone function.
In conclusion, if proper diagnostic and therapeutic approaches are followed, and modifications are planned to circumvent the lack of resources, we can obtain results that are comparable to international standards, at least in terms of complications and sequelae after thyroidectomy.
Authorship/Collaboration- •
Fernando Pereira: study design, data acquisition and collection, analysis and interpretation of the results, article composition, critical review and approval of the final version.
- •
Pablo Calvo: data acquisition and collection, analysis and interpretation of the results, critical review.
- •
Alejandro Arteaga: data acquisition and collection, analysis and interpretation of the results.
- •
Joaquín M. Muñoz: data acquisition and collection, analysis and interpretation of the results.
- •
Lionel W. Nges: data acquisition and collection, analysis and interpretation of the results.
- •
Mireille Kemmoe: data acquisition and collection, analysis and interpretation of the results.
- •
Mercedes Vidal: data acquisition and collection, analysis and interpretation of the results.
- •
Francisco J. Blázquez: data acquisition and collection, analysis and interpretation of the results.
- •
Teresa Vives: data acquisition and collection, analysis and interpretation of the results.
- •
Marina Picón: data acquisition and collection, analysis and interpretation of the results.
- •
Andrés Varela: data acquisition and collection, critical review.
There are no conflicts of interests to declare.
Please cite this article as: Pereira Pérez F, Calvo Espino P, Sánchez Arteaga A, Muñoz Rodriguez JM, Nges LW, Kemmoe M, et al. Cirugía tiroidea en programas de cooperación en África subsahariana. Cir Esp. 2016;94:404–409.