Incisional hernia (HI), in open and laparoscopic surgery, is a very frequent complication. HI located in the umbilical region are called M3. The main aim of this study is to compare HI produced by the placement of an umbilical laparoscopic trocar (M3T) with those located in M3 in open surgery (M3O) in terms of basal characteristics, complications and recurrences; and secondarily the identification of risk factors.
MethodCross-sectional observational study based on the national prospective registry EVEREG during the period of July 2012–June 2018. The main variables were recurrences and postoperative complications. Both groups (M3T and M3O) were compared. Multiple logistic regression was performed to identify the risk factors of the entire cohort.
Results882 had a follow-up time longer than 12 months. M3O group presented superior ASA-Class, more complex HI and previous repair. It also presented a higher recurrence rate at 12 and 24 months (8.6% vs. 2.5%; P < 0,0001 and 9.3% vs. 2.9%; P < 0.0001) and higher postoperative complications rate (21.9% vs. 14.6 %; P = 0.02).
Previous repair, intervention length and associated procedures requirement were identified as risk factors for postoperative complications. Absence of a specialist present during surgery, previous repair, and the absence of complications were identified as risk factors for recurrence. In the PSM analysis no differences were detected in of complications and recurrences.
ConclusionsHI M3O is more complex than M3T. The complexity is not related to the origin of the hernia but to its characteristics and those of the patient.
La hernia incisional (HI) es una complicación frecuente. El objetivo principal de este estudio es comparar, las características, complicaciones y recurrencias de las HI producidas por la colocación de un trocar laparoscópico umbilical (M3T) con la de misma localización tras cirugía abierta (M3O); y de forma secundaria la identificación de factores de riesgo.
MétodoEstudio observacional transversal analizando al registro EVEREG durante el periodo entre Julio 2012 y Junio 2018. Las variables principales fueron recurrencias y complicaciones postoperatorias. Se compararon ambos grupos (M3T y M3O). Se realizó regresión logística múltiple para identificar los factores de riesgo de la cohorte completa.
ResultadosSe incluyeron un total de 882 casos. El grupo M3O presentó un ASA superior, HI con criterios de mayor complejidad para la reparación, mayor número de recurrencias a los 12 y 24 meses (8,6%vs. 2,5%; P < 0,0001 y 9,3% vs. 2,9%; P < 0,0001 respectivamente) y complicaciones postoperatorias (21,9% vs. 14,6%; P = 0,02). Se identificaron como factores de riesgo para la aparición de complicaciones postoperatorias la reparación previa, la duración de la intervención y el requerimiento de procedimientos asociados, y para las recidivas: la ausencia de especialista de pared abdominal, la reparación previa y la aparición de complicaciones. El análisis por puntuación de propensión no detectó diferencias significativas en complicaciones y recurrencias.
ConclusionesLas HI M3 de trocar umbilical son menos complejas que las originadas por cirugía abierta. La complejidad no se relaciona con el origen de la hernia sino con sus características y las del paciente.
Incisional hernias (IH) are abdominal wall defects associated with a surgical incision.1,2 They are a frequent complication after both open and laparoscopic surgery.3,4 This leads to an increase in morbidity, mortality, and healthcare costs. Reports in the literature have extensively defined risk factors,5 recommendations on the optimal surgical technique for abdominal wall closure to prevent their appearance,6,7 and even prophylactic measures.8,9
Trocar-site hernias occur at the insertion points of the trocars used for laparoscopic approaches. While many authors underestimate their incidence, (TSH), few published data are available10,11 their incidence has increased with the expanded use of minimally invasive techniques.4,10,11 Likewise risk factors for TSH have been identified,12 prophylactic measures have been proposed in high-risk patients.13,14
Umbilical IH is the most common TSH given the weakness of the linea alba in this area.15–18 In the classification by the European Hernia Society,19 the term ‘M3’ is used to define all hernias located in this area and either 3 cm above or below the navel.
Registries of surgical interventions are a very useful tool for determining the characteristics of patients, pathologies, treatments and their results in a wide variety of procedures.20,21 Also, based on their findings, these registries help plan future studies and improvements in applied treatments.
The Spanish incisional hernia registry (EVEREG) compiles IH repairs performed in Spain from July 2012 to the present and has demonstrated its usefulness for understanding the situation and treatment.22,23 Previous EVEREG-based studies have shown a better prognosis (lower frequency of complications and recurrences) in TSH compared to other IH types.23
The objective of this study is to analyze (using data from the EVEREG registry) the characteristics of a patient cohort treated surgically for IH in the M3 location (M3T) and to compare them with IH of a similar location associated with open surgery (M3O), in order to determine the causes of the differences in the results detected in previous studies and to know the different prognostic factors that influence the appearance of recurrences and/or complications in the postoperative period of IH repair surgery.
MethodsThis is a cross-sectional cohort study that includes all patients diagnosed with IH located in M3 treated surgically between July 2012 and June 2018, excluding cases that lacked postoperative follow-up data for the analysis of complications or had a follow-up of less than one year for the analysis of recurrences.
For comparison, the cases were divided into 2 patient cohorts: one group whose hernias were the result of laparoscopic surgery using an umbilical trocar (M3T), and the other group whose hernias were a result of other types of laparotomy (M3O).
Data were obtained from the EVEREG Registry, whose IH data collection protocol is authorized by the Clinical Research Ethics Committee of the Parc de Salut Mar (2012/4908/I) and complied with the regulations of Spanish Data Protection Law 15/1999.
We collected variables related to patient characteristics: age, sex, body mass index (BMI), smoking, chronic obstructive pulmonary disease (COPD), diabetes mellitus (DM), immunosuppression, cancer, and grade according to the American Society of Anesthesiologists (ASA) classification. Hernia characteristic variables were: defect diameter/area, and presence of previous repair. Characteristics of the repair procedure included: duration, approach, indication, outpatient surgery (OS), type of surgeon, access, and technique-related factors (intestinal resection, separation of components, mesh, type of sutures, defect closure, associated procedures). The main study variables were the postoperative complications during the first month, with their associated characteristics and postoperative recurrences after 6, 12 and 24 months.
Statistical analysisThe statistical analysis was conducted with the IBM SPSS software package for Windows version 23.0 (IBM Corp, Armonk, NY). Continuous variables are described as mean and standard deviation (SD), and categorical variables are reported as absolute numbers and percentages. The chi-squared test was applied for the comparison of categorical variables (or the Fisher test, if appropriate) and Student’s t-test (or Mann–Whitney test) for the comparison of continuous variables.
A multivariate analysis was performed to identify risk factors for the development of complications and recurrences in the group of patients with hernias located at M3 (M3T + M3O). The predictive capacity of each variable and its independence from the other predictor variables were analyzed using a binomial logistic regression model, sequentially introducing the variables with an F of 0.5.
Propensity score matching was performed to homogenize the groups and eliminate the probability of attributing certain results to the intrinsic characteristics of the patients and the hernias in the groups (M3T and M3O).
For the sample size, 171 patients were estimated to be necessary for each group (M3T and M3O, respectively), using the GRANMO program (GRANMO sample size calculator, version 7.12, Institut Municipal d'Investigació Mèdica, Barcelona, Spain) and the approximation of the arcsin (accepting an alpha risk of 0.05 and a beta risk of 0.2 in a bilateral contrast).
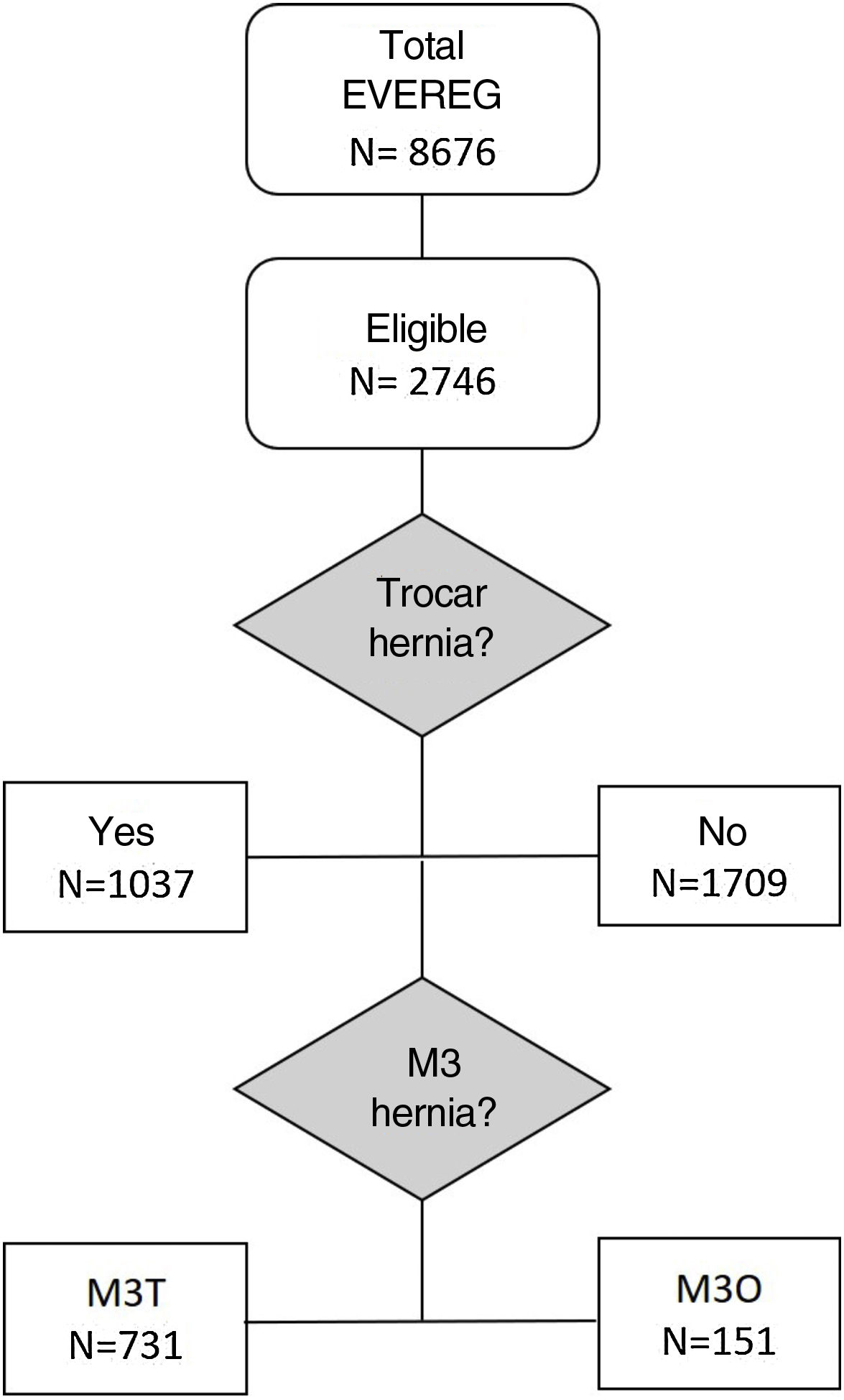
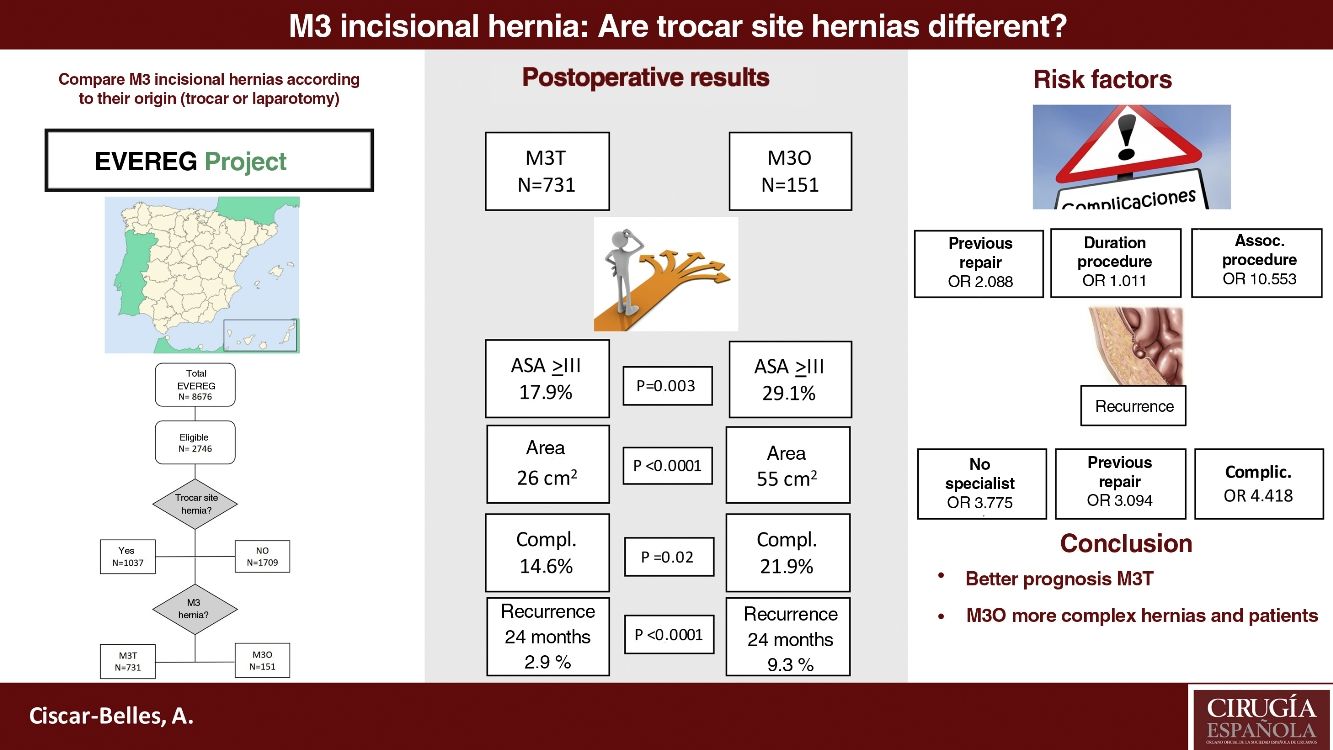
ResultsBy June 2018, 8676 patients had been registered, 1037 of which were TSH. A total of 882 (731 M3T and 151 M3O) were valid for the study (Fig. 1).
Table 1 shows the characteristics of the patients in both groups. Homogeneity was observed in terms of: age, sex, BMI and comorbidities. In contrast, in the M3O group there was a greater number of patients (P = .003), with high surgical risk (ASA III-IV).
Patient characteristics and comparison between groups.
| M3T n = 731 | M3O n = 151 | P | |
|---|---|---|---|
| Age (SD) | 65.9 (13.6) | 67.53 (12.1) | 0.19 |
| Sex M/F, n (%) | 226/505 (30.9/69.1) | 56/95 (37.1/62.9) | 0.20 |
| BMI (SD) | 30.35 (5) | 30.93 (5.2) | 0.92 |
| Obese BMI > 30, n (%) | 362 (49.5) | 83 (55) | 0.25 |
| Overweight, BMI > 25, n (%) | 645 (88.2) | 135 (89.4) | 0.79 |
| Smoking, n (%) | 47 (20.1) | 34 (22.5) | 0.58 |
| COPD, n (%) | 85 (11.6) | 25 (16.6) | 0.12 |
| Diabetes mellitus, n (%) | 142 (19.4) | 34 (22.5) | 0.58 |
| Immunosuppression, n (%) | 12 (1.6) | 4 (2.6) | 0.61 |
| Cancer, n (%) | 71 (9.7) | 22 (14.6) | 0.10 |
| ASA III/IV, n (%) | 131 (17.9) | 44 (29.1) | 0.003 |
M3T, trocar-related umbilical incisional hernia; M3O, non-trocar umbilical incisional hernia; BMI, body mass index; COPD, chronic obstructive pulmonary disease; ASA, American Society of Anesthesiologists classification; SD, standard deviation.
Regarding the intrinsic characteristics of umbilical IH (Table 2), the M3O group presented significantly larger diameters and areas (6.9 vs 4.8 cm, P < .0001; 6.6 vs 4.4 cm, P < .0001; 55.1 vs 26 cm2, P < .0001, respectively). The M3O group also had a higher percentage of patients with previous IH repair (33.8% vs 10.4%; P < .0001).
Comparison of hernia characteristics.
| M3T n = 731 | M3O n = 151 | P | |
|---|---|---|---|
| Diameter, longitudinal, cm (SD) | 4.8 (2.9) | 6.9 (3.7) | <0.0001 |
| Diameter, transversal, cm (SD) | 4.4 (2.4) | 6.6 (3.6) | <0.0001 |
| Area, cm2 (SD) | 26 (36.9) | 55.1 (56.5) | <0.0001 |
| Previous repair, n (%) | 76 (10.4) | 51 (33.8) | <0.0001 |
M3T, trocar-related umbilical incisional hernia; M3O, non-trocar umbilical incisional hernia; SD, standard deviation.
The characteristics of the hernia repair (Table 3) were similar in terms of type of approach, performed by a specialist, use of component separation, mesh repair, and its position. However, in the M3O group, the procedures lasted longer (80.52 vs 58.4 min; P < .0001) and were performed in a lower percentage in an outpatient setting (8.9% vs 30.8%; P < .0001) and required intestinal repair/resection more frequently (2% vs 0.1%; P = .02). Laparoscopic surgery was more common for repair in the M3O group (19.9% vs 9%; P < .0001), and they also required associated procedures in a higher percentage of cases (17.9% vs 5.6%; P < .0001).
Procedure data and comparison between groups.
| M3T n = 731 | M3O n = 151 | P | |
|---|---|---|---|
| Duration (SD) | 58.4 (29.9) | 80.52 (41.5) | <0.0001 |
| Type of approach, n (%) | 0.80 | ||
| Elective | 708 (96.9) | 146 (96.7) | |
| Urgent | 2.3 (3.1) | 5 (3.3) | |
| MAS, n (%) | 225 (30.8) | 13 (8.9) | <0.0001 |
| Specialist present, n (%) | 168 (46.8) | 31 (51.7) | 0.49 |
| Access type, n (%) | |||
| Open | 665 (91) | 121 (80.1) | <0.0001 |
| Laparoscopic | 66 (9) | 30 (19.9) | |
| Intestinal repair/resection, n (%) | 1 (0.1) | 3 (2) | 0.02 |
| Separation of components, n (%) | 21 (2.9) | 6 (4) | 0.44 |
| Mesh repair, n (%) | 704 (96.3) | 149 (98.7) | 0.20 |
| Double mesh, n (%) | 35 (4.9) | 15 (10) | 0.015 |
| Mesh position, n (%) | |||
| Onlay | 221 (31.4) | 46 (30.9) | 0.85 |
| Intraperitoneal | 181 (25.7) | 45 (30.2) | 0.30 |
| Inlay | 39 (5.5) | 7 (4.7) | 0.84 |
| Sublay | 260 (37) | 51 (34.2) | 0.51 |
| Suture, n (%) | 613 (86.8) | 97 (66.4) | <0.0001 |
| Staples, n (%) | 78 (11.2) | 40 (27.8) | <0.0001 |
| Closure of the defect, n (%) | 540 (74.4) | 95 (62.9) | 0.003 |
| Associated procedures, n (%) | 41 (5.6) | 27 (17.9) | <0.0001 |
M3T, trocar-related umbilical incisional hernia; M3O, non-trocar umbilical incisional hernia; SD, standard deviation; MAS, major ambulatory surgery.
Regarding the results of surgery (Table 4), the M3O group presented a higher number of complications (21.9% vs 14.6%; P = .02), while intestinal obstruction and ‘other complications’ were the only ones that showed statistically significant differences. The M3O group also presented a higher frequency of recurrence after 6, 12 and 24 months, although only the last two periods presented statistically significant differences (3.3% vs 1.4%, P = .07; 8.6% vs 2.5%, P < .0001; and 9.3% vs 2.9%, P < .0001, respectively).
Postoperative complications and recurrences.
| M3T n = 731 | M3O n = 151 | P | |
|---|---|---|---|
| N | 731 | 151 | |
| Complications, n (%) | 107 (14.6) | 33 (21.9) | 0.02 |
| SSE* | 88 (12) | 25 (16.6) | 0.1 |
| Wound infection | 17 (2.3) | 6 (4) | 0.3 |
| Hematoma | 15 (2.1) | 3 (2) | 1 |
| Seroma | 63 (8.6) | 2 (1.3) | 0.6 |
| Wound necrosis | 4 (0.5) | 2 (1.3) | 0.3 |
| Intestinal obstruction | 2 (0.3) | 4 (2.6) | 0.01 |
| Other complications | 59 (8.1) | 21 (13.9) | 0.03 |
| N | 731 | 151 | |
| Recurrence, n (%) | |||
| >6 months | 10 (1.4) | 5 (3.3) | 0.07 |
| >12 months | 18 (2.5) | 13 (8.6) | <0.0001 |
| >24 months | 21 (2.9) | 14 (9.3) | <0.0001 |
M3T, trocar-related umbilical incisional hernia; M3O, non-trocar umbilical incisional hernia.
In propensity score matching (PSM) (Table 5), statistically significant differences were observed in the duration of the intervention, use of staples, and requirement of associated procedures, all of which were higher in the M3O group. On the other hand, in the application of the outpatient surgery regimen, mesh suture and defect closure were superior in the M3T group. In contrast, no differences were observed between the two in terms of complications and recurrences.
Propensity score matching (PSM).
| M3T n = 149 | M3O n = 149 | P | |
|---|---|---|---|
| Patient characteristics | |||
| Age (SD) | 68.1 (12.6) | 67.5 (12) | 0.67 |
| Sex, M/F n (%) | 46/103 (45.5/52.3) | 55/94 (54.4/47.7)) | 0.27 |
| BMI (SD) | 31.7 (5.5) | 30.95 (5.2) | 0.22 |
| Obese, BMI > 30 n (%) | 90 (60.4) | 82 (55) | 0.35 |
| Overweight, BMI > 25 n (%) | 135 (90.6) | 133 (89.3) | 0.7 |
| Smoking, n (%) | 22 (14.8) | 33 (22.1) | 0.1 |
| COPD, n (%) | 20 (13.4) | 25 (16.8) | 0.42 |
| Diabetes mellitus, n (%) | 39 (26.2) | 33 (22.1) | 0.4 |
| Immunosuppression, n (%) | 3 (2) | 4 (2.7) | 0.7 |
| Cancer, n (%) | 13 (8.7) | 21 (14.1) | 0.14 |
| ASA III/IV, n (%) | 49 (32.9) | 43 (28.9) | 0.4 |
| Hernia characteristics | |||
| Area, cm2 (SD) | 48.5 (66.6) | 55.1 (56.5) | 0.36 |
| Diameter, transverse, cm (SD) | 6 (3.2) | 6.6 (3.6) | 0.1 |
| Diameter, longitudinal, cm (SD) | 6.44 (4) | 6.9 (3.7) | 0.3 |
| Previous repair, n (%) | 43 (28.9) | 51 (34.2) | 0.3 |
| Procedure data | |||
| Duration, minutes (SD) | 68.5 (32.3) | 81 (41.4) | 0.004 |
| Type of approach, n (%) | |||
| Elective | 144 (96.6) | 144 (96.6) | 1 |
| Urgent | 5 (3.4) | 5 (3.4) | 1 |
| MAS, n (%) | 27 (18.1) | 13 (8.7) | 0.017 |
| Specialist present, n (%) | 26 (44.1) | 31 (51.7) | 0.4 |
| Type of access, n (%) | |||
| Open | 129 (86.6) | 119 (79.9) | 0.1 |
| Laparoscopic | 20 (13.4) | 30 (20.1) | |
| Intestinal repair/resection, n (%) | 1 (0.7) | 3 (2) | 0.3 |
| Separation of components, n (%) | 6 (4) | 6 (4) | 1 |
| Mesh repair, n (%) | 144 (96.6) | 148 (99.3) | 0.099 |
| Double mesh, n (%) | 12 (8.1) | 15 (10.1) | 0.5 |
| Mesh position, n (%) | |||
| Onlay | 47 (32.6) | 45 (30.2) | 0. |
| Intraperitoneal | 38 (26.4) | 45 (30.2) | 0.47 |
| Inlay | 8 (5.6) | 7 (4.7) | 0.74 |
| Sublay | 50 (34.7) | 51 (34.2) | 0.9 |
| Suture, n (%) | 118 (84.3) | 96 (66.2) | <0.001 |
| Staples, n (%) | 20 (14.5) | 40 (28) | 0.006 |
| Defect closure, n (%) | 113 (75.8) | 94 (63.1) | 0.017 |
| Associated procedures, n (%) | 6 (4) | 27 (18.1) | <0.001 |
| Postoperative complications and recurrences | |||
| SSE, n (%) | 20 (13.4) | 25 (16.8) | 0.42 |
| Complications, 1 month, n (%) | 25 (16.8) | 32 (21.5) | 0.3 |
| Prolonged ileus, n (%) | 1 (0.7) | 4 (1.3) | 0.17 |
| Hematoma, n (%) | 2 (1.3) | 3 (2) | 0.6 |
| Necrosis, n (%) | 1 (0.7) | 2 (1.3) | 0.5 |
| Infection, n (%) | 5 (3.4) | 6 (4) | 0.78 |
| Seroma, n (%) | 17 (5.7) | 15 (5) | 0.7 |
| Obstruction, n (%) | 1 (0.7) | 4 (2.7) | 0.17 |
| Other complications, n (%) | 16 (10.7) | 20 (13.4) | 0.48 |
| Recurrence, n (%) | |||
| >6 months | 3 (2) | 5 (3.4) | 0.47 |
| >12 months | 5 (3.4) | 13 (8.7) | 0.052 |
| >24 months | 6 (4) | 14 (9.4) | 0.06 |
M3T, trocar-related umbilical incisional hernia; M3O, non-trocar umbilical incisional hernia; BMI, body mass index; SD, standard deviation; COPD, chronic obstructive pulmonary disease; ASA, American Society of Anesthesiologists classification; MAS, minor ambulatory surgery; SSE, surgical site events.
In the multivariate analysis performed on the group of patients (M3T and M3O), previous repair (OR 2.088 [95% CI 1.052-4.143; P = .035]), duration of the intervention (OR 1.011 [95% CI 1.003–1.019; P = .005]), and the requirement for associated procedures (OR 10.552 [95% CI 1.215–91.6; P = .033]) were identified as risk factors for the appearance of complications one month after surgery (Table 6).
Variables associated with postoperative complications and recurrence.
| Postoperative complications | |||
|---|---|---|---|
| OR | CI | P | |
| Previous repair | 2.088 | 1.052−4.143 | 0.035 |
| Duration of the intervention | 1.011 | 1.003−1.019 | 0.005 |
| Associated procedures | 10.553 | 1.215−91.6 | 0.033 |
| Recurrence | |||
|---|---|---|---|
| OR | IC | P | |
| Surgeon not specialized | 3.775 | 1.314−10.842 | 0.014 |
| Previous repair | 3.094 | 1.167−8.205 | 0.023 |
| Absence of complications | 4.418 | 1.757−11.11 | 0.002 |
OR, odds ratio; CI, confidence interval.
Risk factors for recurrence included: surgery performed by a non-specialized surgeon (OR 3.775 [95% CI 1.314–10.842; P = .014]), previous repair (OR 3.094 [95% CI 1.167–8.205; P = .023]), and the appearance of complications one month after surgery (OR 4.418 [95% CI 1.757–11.11; P = .002]) (Table 6).
DiscussionSurgery for IH repair is a very common situation that generates many complications and healthcare costs.23,24 With the advent of laparoscopic surgery, it was believed that, by reducing the size of the incision, the problem of IH would be less.12,13 However, an increase in the frequency of TSH is being observed, which also coincides with the expansion of indications for laparoscopic surgery in recent years.10,25
The reported incidence of TSH ranges from 0.3% to 31.9%,10 although reports of higher percentages seem more realistic, especially in more complex surgery.4 Also, in many cases this may be underestimated given the few symptoms that many patients present, insufficient follow-up periods, and the lack of prospective studies with adequate imaging techniques published in the literature. Likewise, the figures offered by hernia registries show a significant percentage of repairs related to TSH22; hence the importance of knowing in detail the circumstances related to repair, and whether there are differential characteristics of patients with similar hernias originating in a laparotomy that explain the lower frequency of complications and recurrences.23 In other words, whether the origin of the hernia (laparoscopy or laparotomy) influences the surgical results, or whether other factors are involved.
In our study, the comparison of the individual characteristics between the patients of the two groups did not show differences in their general characteristics: age, sex, BMI, smoking and comorbidities. However, the M3O group had a higher anesthetic risk than the M3T group. This fact could be related to the presence of more general complications that the M3O group also presented and could be a consequence of selection bias for primary surgery of patients who are candidates for laparoscopic surgery. TSH are probably not more frequent in ASA I-II patients, but instead a greater number of patients with lower anesthetic risk are considered candidates for minimally invasive surgery.
Regarding the characteristics of IH itself (M3), we observed that the M3O group presented hernias with larger diameters and, consequently, larger areas than the M3T group. This could be related to the size of the initial incision, since in laparoscopic surgery the incision is limited to the diameter of the trocar (10–12 mm), while the M3O group came from larger laparotomies located in the umbilical region (M3), which would explain these differences in the dimensions of the IH. The M3O group presented a higher percentage of previous repairs and is probably one of the causes of the higher frequency of recurrences detected during follow-up, as shown by the multivariate analysis. All these data indicate that the hernias of the M3O group were more complex and would support the hypothesis that TSH have a better prognosis due to their size.
When analyzing the characteristics of the intervention for hernia repair, some significant differences were also identified. The M3O group required a longer surgical time, intestinal resections were performed more frequently, and the hernia defect was less frequently completely closed. These data again indicate more complex hernias and repairs. The M3O group presented a lower percentage of interventions in an outpatient setting, which is another fact that seems to be related to the complexity of the repair surgery. Furthermore, as mentioned above, these patients have a higher anesthetic risk.
The M3O group presented a higher number of complications in general and particularly in terms of intestinal obstruction and other complications. More wound-related complications were also observed, although these findings were not significant.
Regarding recurrences, the group of M3O patients presented a higher incidence in all follow-up periods, reaching statistical significance at one year. Again, these data point to a greater complexity of hernias originating from laparotomies and is related to the higher risk of patients.
To bolster this hypothesis, the PSM was performed to eliminate the bias due to the confusion of the variables of the subjects on the final result. In this study, it was applied to find out whether the differences between the results (higher rate of complications and recurrences in the M3O group) were due to the individual patient characteristics or the surgical technique used (laparotomy). What initially suggested that M3O hernias could produce worse results because they were caused by laparotomies was discarded when we conducted the PSM, as the peculiarities of each group of patients were eliminated (for example, the fact that there were more patients with ASA III in the M3O group), which made the differences between results disappear. In other words, the surgical origin of IH, laparoscopy or laparotomy does not influence the appearance of complications and subsequent recurrences. What does have an influence are the intrinsic characteristics of the patients.
Second, this analysis identified risk factors for the appearance of recurrences and complications in the total patient cohort (M3T and M3O). Recent studies have identified obesity, DM, smoking, and hernia size26–28 as risk factors for complications, although in our cohort only previous repair, duration of the operation, and the requirement for associated procedures were identified as risk factors for the appearance of complications. Although the bivariate analysis showed that M3O had a higher percentage of complications in the multivariate analysis, M3T did not show to be a protective factor for the development of complications.
When the repair was not performed by a team specialized in abdominal wall surgery, the risk of recurrence was almost 4 times higher in either of the two groups analyzed. This fact seems logical, since, as other studies indicate, specializing in wall surgery reduces the frequency of recurrences.29 Moreover, this would support the proposal that procedures with complexity criteria should be referred to specialized centers or surgical teams.24,26,29
The finding of prior repair as a risk factor for complications and recurrences has already been identified previously,23 and, according to our data, it was also shown to be a risk factor for recurrence, as was the appearance of postoperative complications.
One of the limitations of the study is the bias due to loss of follow-up of 2492 subjects who presented IH in the M3 location (783 M3T and 1709 M3O), and only 882 (731 M3T and 151 M3O) presented complete data and a follow-up of up to 24 months. If a larger number of cases had complete data available, the power of the conclusions could have been greater. In addition, the EVEREG registry is a national prospective data entry registry based on different specialties in the Spanish territory, and we cannot determine the clinical and/or radiological criteria; this could create limitations for the diagnosis of IH, recurrence and some of the complications. Likewise, all data related to hernias are not thoroughly registered or are difficult to retrieve, so some of them could not be analyzed (diagnosis of the initial intervention, length of the initial laparotomy, type of trocar used, etc). The strengths of the study are that it is multicenter, the data were collected prospectively, and the 24-month follow-up time is similar to that of other registry-based studies.30
Finally, we can conclude that umbilical IH caused by trocar placement are less complex than incisional hernias that appear in the same location after laparotomy. This is due to their size and because they affect patients with lower surgical risk, so they are less likely to develop postoperative complications and recurrences when treated with the same surgical techniques. Although the initial surgical technique (laparoscopy or laparotomy) influences the size and complexity of IH, we must take into account the bias produced by the fact that patients with M3O have more comorbidities and are not considered candidates for the laparoscopic approach in their initial surgery.
Therefore, we believe that these patients with high anesthetic risk, whenever possible, should undergo laparoscopic surgery so that, if a hernia develops, both it and its repair would be less complex.
The lower complexity that accompanies M3T hernias allows us to suggest that, for the most part, if no complexity criteria are present, these hernias can be repaired in non-specialized hospitals. However, M3O hernias, even those that are small in size, should be treated by specialized abdominal wall units.
FundingB. Braun.
Conflict of interestsThe authors have no conflict of interests to declare.
The authors would like to thank Silvia Martínez and Xavier Masramón, SAIL (Servicio de Asesoría a la Investigación y Logística), and Silvia Glahn (B. Braun).
Antonio Utrera González, Hospital Juan Ramón Jiménez, Huelva.
José M, Capitán Vallvey; Complejo Hospitalario de Jaén, Jaén.
Matías Pradas, Hospital Comarcal de Ronda, Ronda.
Daniel Pérez Gomar, Hospital Universitario Puerta del Mar, Cádiz.
Manuel Bustos, Hospital Virgen del Rocío, Sevilla.
Francisco Antonio Herrera Fernández, Hospital Comarcal Santa Ana, Motril.
Juan A, Blanco, Hospital Civil de Málaga.
Joaquim Robres Puig, Consorci Sanitari Integral de l’Hospitalet, Barcelona.
Rafael Villalobos, Hospital Arnau de Vilanova, Lleida.
Dolors Güell Puigcercos, Hospital de Terrassa, Terrassa.
José María Puigcercós Fusté, Hospital Dos de Maig, Barcelona.
Vicente Ayuso Osuna, Hospital Espíritu Santo, Santa Coloma Gramanet.
Marta Piñol, Hospital Espíritu Santo, Santa Coloma Gramanet.
Carles Olona Casas, Hospital Joan XXIII, Tarragona.
Francisco Martínez Ródenas, Hospital Municipal de Badalona, Badalona.
Jordi Comajuncosas, Hospital Parc Sanitari Sant Joan de Deu, Sant Boi.
Enric Sebastián Valverde, Hospital Parc Sanitari Sant Joan de Deu, Sant Boi.
Sara Amador, Hospital de Granollers.
Jaume Gelonch, Hospital de Palamós.
Helena Vallverdú, Hospital de Vic.
Magda Abelló Sala, Hospital Pius, Valls.
Antonio Veres Gómez, Hospital de la Cerdaña.
Rosa Gamón, Hospital General de Castellón.
Pedro García Peche, Hospital General Universitario Reina Sofía, Elche.
Miguel González Valverde, Hospital General Universitario Reina Sofía, Elche.
Miguel Ángel Martín Blanco, Hospital de Vinaroz.
Ramón J Ferri, Hospital Lluís Alcanyís, Valencia.
Elena Martí Ciñat, Hospital Malvarrosa, Valencia.
Providencia García Pastor, Hospital Universitario La Fe, Valencia.
Carlos Montero, Hospital Virgen de los Lirios, Alcoy.
Miguel Ángel Lorenzo Liñán, Hospital General de Onteniente.
Vicente Barbero, Complejo Hospitalario Virgen de la Salud, Toledo.
Miguel Ángel Morlan, Complejo Hospitalario Virgen de la Salud, Toledo.
José María Jover, Hospital de Getafe.
Isabel Delgado Lillo, Hospital Clínico San Carlos, Madrid.
María Mercedes Sanz Sánchez, Hospital General Universitario Gregorio Marañón, Madrid.
Leire Zarain Obrador, Hospital General Universitario Gregorio Marañón, Madrid.
Alejandro Lusilla, Hospital General Universitario Gregorio Marañón, Madrid.
Juan Jesús Cabeza Gómez, Hospital Clínico San Carlos, Madrid.
Antonio López, Hospital Nuestra Señora del Prado, Talavera de la Reina.
Teresa Butrón, Hospital Universitario 12 de Octubre, Madrid.
Guillermo Supelano Eslait, Hospital Universitario 12 de Octubre, Madrid.
José Luis Álvarez Conde, Complejo Hospitalario de Palencia.
Baltasar Pérez Saborido, Hospital Rio Ortega, Valladolid.
Mario Rodríguez López, Hospital Rio Ortega, Valladolid.
Santiago Revuelta Álvarez, Hospital Universitario Marqués de Valdecilla, Santander.
Pedro Trillo Parejo, Complexo Hospitalario Universitario, Orense.
José Luis Rodicio, Hospital Universitario Central de Asturias, Oviedo.
Antonio Blanco, Hospital Universitario Central de Asturias, Oviedo.
Agustín Juan Cano Maldonado, Complejo Hospitalario Universitario Cartagena.
Ańgel Zorraquino González, Hospital de Basurto, Vizcaya.
Jesús Damián Turiño Luque, Hospital Civil de Málaga.
Esther Guisasola, Hospital Universitario Donostia.
Fernando Fernández, Hospital Central de la Defensa “Gómez Ulla”, Madrid.
Javier Granell, Hospital Universitario Príncipe de Asturias. Alcaláde Henares.
Juan Antonio Bellido Luque. Hospital de Riotinto, Huelva.
Juan Manuel Rueda Pérez. Complejo Hospitalario Universitario Cartagena.
Ma Pilar Anaya Reig, Hospital General de Onteniente.
Rafael Gómez Sabater, Hospital de Vinaros.
Rosa Ana García Díaz, Hospital Universitario Marqués de Valdecilla, Santander.
Verónica Alonso. Hospital Dos de Maig, Barcelona.
List of EVEREG group members.
Please cite this article as: Ciscar Belles A, Makhoukhi T, López-Cano M, Hernández Granados P, Pereira Rodríguez JA y miembros del grupo EVEREG. Hernia incisional umbilical (M3). ¿Son diferentes las hernias de trócar? Análisis comparativo del registro EVEREG. Cir Esp. 2022;100:336–344.