Central venous catheterization is a very common procedure that is performed on a daily basis in clinical practice. It is used for hemodynamic management and for the administration of drugs that are toxic or irritating to peripheral veins, administration of parenteral nutrition or perioperative fluid management.1–3 Nonetheless, catheterization may lead to complications, such as arterial puncture (with or without local, cervical or mediastinal hematoma), venous thrombosis, pneumothorax, cardiac arrhythmias, misplaced catheter, air embolism, catheter/guidewire rupture and embolism, and puncture of neighboring structures. These complications are associated any thing such as with the catheter (type of material, caliber), patient (anatomical alterations, coagulopathy), insertion site (internal jugular vein, subclavian vein) or with the technique itself.1
We present the case of a patient who developed a cervical-mediastinal hematoma due to iatrogenic injury of the carotid artery. This complication appeared after catheterization of the right internal jugular vein during anesthetic management of liver transplantation and was satisfactorily resolved with the placement of a stent.
The patient is a 52-year-old male with a prior history of type II diabetes mellitus, chronic renal insufficiency due to membranous glomerulonephritis requiring kidney transplantation in September 1995, and diagnosis of liver cirrhosis due to HCV in September 1992. He had been hospitalized on several occasions due to fluid retention and had episodes of upper gastrointestinal bleeding due to esophageal varices, with clinical stage Child–Pugh B and a MELD score of 15 at the time liver transplantation was indicated.
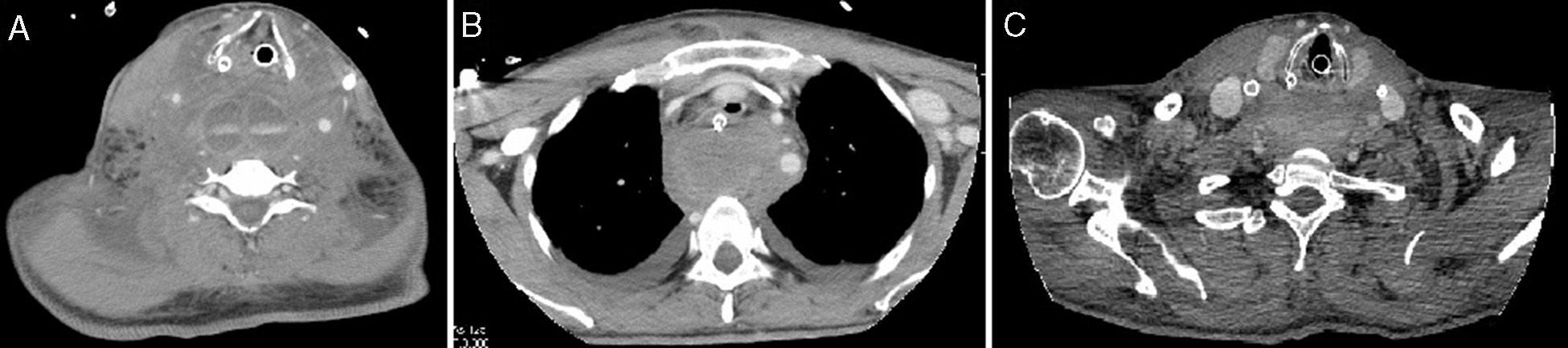
The patient underwent liver transplantation with standard anesthetic management (central venous line, Swan–Ganz, arterial line), with a surgical time of 4h and the following workup results after surgery: prothrombin time 56%; hemoglobin 8g/dL; 62000 platelets. Upon admittance to the ICU, a right-side cervical mass was observed, along with high pressures on the respirator (>33.1mmHg). Cervical ultrasound demonstrated a large right cervical hematoma and displacement of the trachea toward the left. Cervical-thoracic CT (Fig. 1 A and B) with intravenous contrast detected a large right cervical hematoma and an active bleeding point from the posteromedial wall of the right common carotid artery that was 2.5cm from the carotid bifurcation. The hematoma extended toward both sides of the neck and toward the posterior mediastinum along its entire length through the retrotracheal space and retropharynx. The diameter of the hematoma in the retrotracheal region was 7–8cm (transversal) and 4cm (anteroposterior).
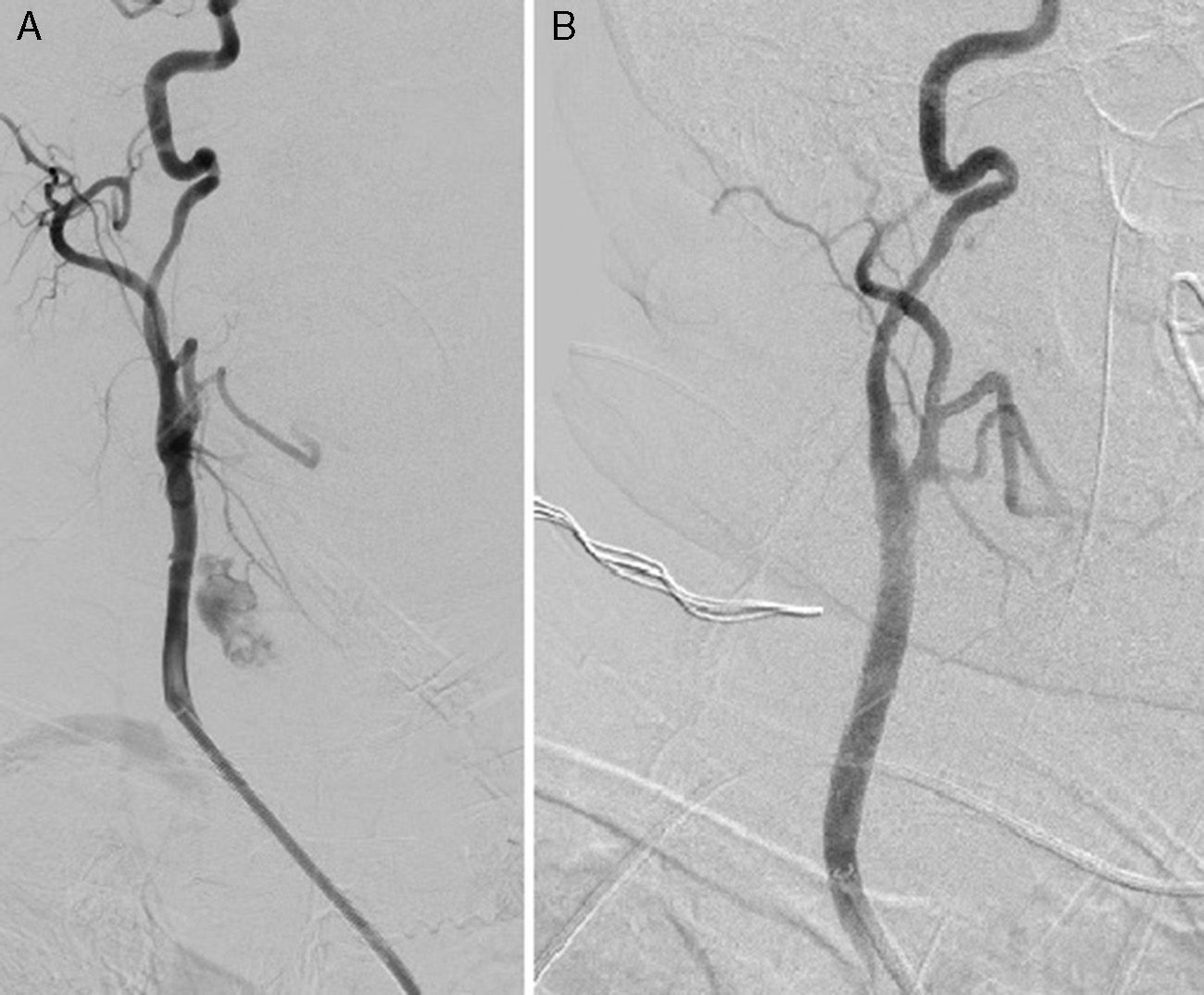
After 2h of clinical observation and given the progression of the hematoma, selective arteriography was indicated, using the Seldinger technique. This confirmed the origin of the hemorrhage at the right common carotid artery (Fig. 2A), at which time we placed a coated 7mm ViaBahn stent at the site of the arterial wound. The follow-up radiography series demonstrated the hemostatic effectiveness of the stent (Fig. 2B).
On a follow-up CT on the fourth day after hospitalization (Fig. 1C), no ischemic brain lesions were observed, and the size of the hematoma had diminished in the cervical and thoracic regions. On the fifth day post-op, the patient was able to be extubated. Good oxygen saturation and gas exchange levels were achieved with nasal cannula, and liver function was normal. The patient was therefore moved to the hospital ward on the following day and discharged from the hospital 20 days after transplantation. The patient is currently asymptomatic and the hematoma has been completely reabsorbed.
The Seldinger technique is habitually used to obtain central venous access. It basically involves the percutaneous insertion of a needle into a blood vessel, followed by the introduction of a guidewire into the blood vessel through the needle and later insertion of the catheter along the guidewire.4 Classically, the place for insertion of central venous lines has been determined by palpation or visualization of anatomical reference structures that have a known relationship with the vein to be catheterized. In recent years, however, the use of ultrasound-guided vascular punctures has become more widespread. Although several prospective studies2,3,5–10 have supported the use of ultrasound as a precise technique (higher percentage of insertion on the first attempt) that is quick and useful for preventing complications of central venous catheterization, its use has still not become widespread in clinical practice due to the insufficient number of ultrasound devices and/or the lack of trained professionals, as in our case.
This case report supports the systematic use of ultrasound during central venous cannulation in order to prevent or minimize the appearance of complications associated with the technique.
Please cite this article as: Llàcer-Millán E, Ramírez P, Sanmartín J, Zamarro J, Parrilla P. Hematoma cervical y mediastínico por herida carotídea al canalizar la vena yugular resuelta mediante stent. Cir Esp. 2015;93:342–344.