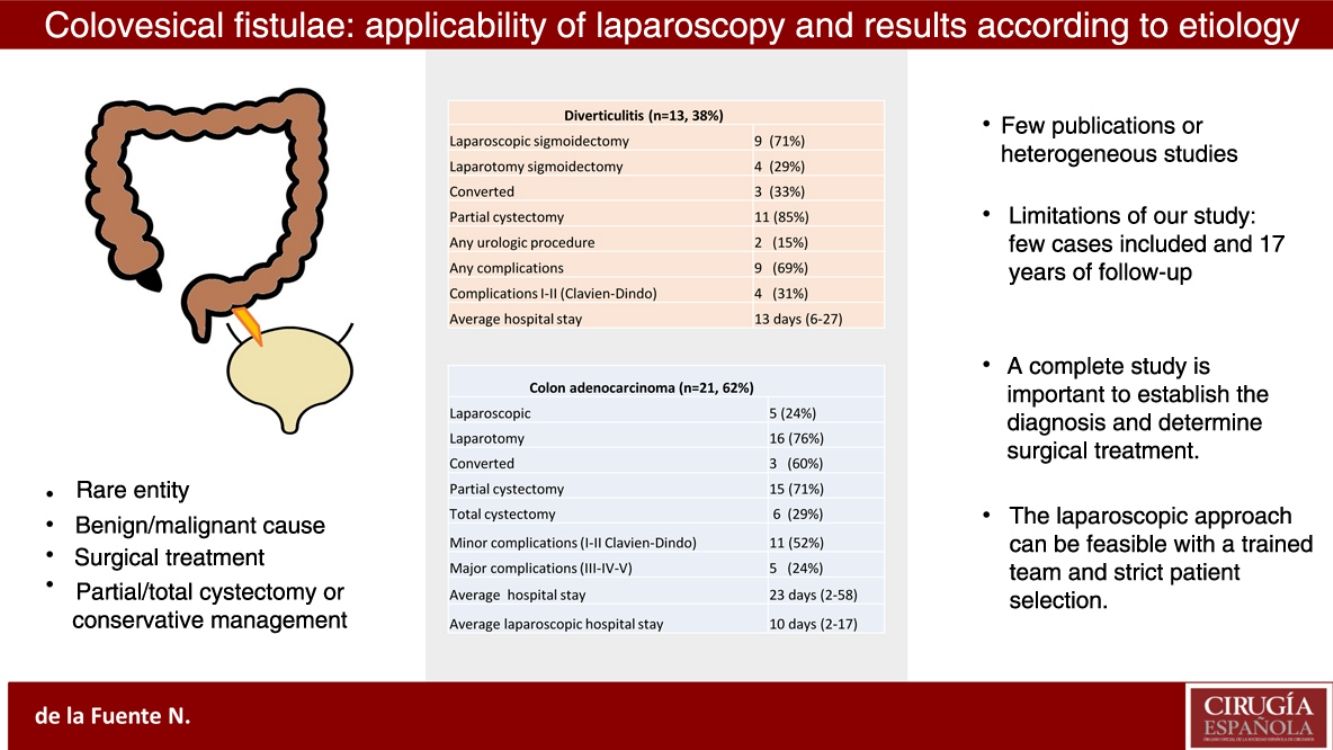
Colovesical fistulae have significant morbidity. The aim of our study was to describe a case series of benign and malignant colovesical fistulae, focusing on the viability of the laparoscopic approach.
MethodsWe reviewed the characteristics of 34 patients with diverticular and colon adenocarcinoma-related colovesical fistulae treated surgically from January 2001 to March 2018, 28 with elective surgery and 6 by urgent surgery. The diagnosis was established by abdominal CT scan, colonoscopy and cystoscopy. Clinically stable patients, with no retroperitoneal or bladder trigone invasion, were approached laparoscopically.
ResultsThere were 13 benign cases (all of them approached by sigmoidectomy), 9 performed by laparoscopy with 3 conversions. Partial cystectomy was done in 11 cases, and in two cases conservative management with urinary catheter. Five laparoscopic approaches were performed in 21 patients diagnosed with malignant colovesical fistula, with 3 conversions and 16 laparotomies. The procedures were sigmoidectomy, left colectomy, anterior resection and pelvic exenteration. All of them required partial or total cystectomy. Sixteen patients had complications, most of which were minor (Clavien-Dindo classification I–II) and with laparotomy approach.
ConclusionsThe laparoscopic approach can be feasible in well-selected and stable patients, but we have to take into consideration that the conversion rate can be high and this surgery should be performed by experienced surgeons.
Las fístulas colovesicales son una entidad poco frecuente y con una incidencia precisa desconocida. El objetivo de este estudio es describir una serie de casos de pacientes intervenidos por fístula colovesical de origen benigno y maligno y valorar la aplicabilidad del abordaje laparoscópico en ambos grupos.
MétodosRealizamos un estudio descriptivo de 34 pacientes intervenidos en nuestro centro entre enero de 2001 y marzo de 2018 con el diagnóstico de fístula colovesical. Se incluyen pacientes intervenidos de manera electiva (28) y de urgencia (6). Se categorizaron según el diagnóstico mediante pruebas complementarias por TC abdominal, colonoscopia y cistoscopia, y se realizó un abordaje laparoscópico en los pacientes sin infiltración del trígono vesical y plano retroperitoneal y con situación clínica favorable.
ResultadosEn los casos con patología benigna (13) se realizaron 4 intervenciones vía laparotómica y 9 vía laparoscópica, con 3 conversiones. En todos los casos se realizó sigmoidectomía. En 11 pacientes se realizó cistectomía parcial y en 2 casos el manejo fue conservador con sonda vesical. En los 21 pacientes con patología maligna se realizaron 5 abordajes laparoscópicos y se convirtieron 3, con 16 casos abordados vía laparotómica. Se realizaron sigmoidectomía, hemicolectomía izquierda, resección anterior y exenteración pélvica, y abordaje urológico en todos los casos. Dieciséis pacientes (76%) tuvieron complicaciones, la mayoría menores (I-II según la clasificación de Clavien-Dindo) e intervenidos por abordaje laparotómico.
ConclusionesEl tratamiento de elección en las fístulas colovesicales es la cirugía con resección colónica y abordaje urológico según el caso y el diagnóstico etiológico. El abordaje laparoscópico puede ser factible en casos muy bien seleccionados y con una situación clínica favorable, teniendo en cuenta que el umbral de conversión debe ser bajo y la intervención ha de ser llevada a cabo por un equipo con experiencia.
Colovesical fistulae are a rare entity, whose precise incidence is unknown (estimated 1 in 3000 surgical hospital admissions),1 consisting of an abnormal communication between the colon (usually sigmoid) and the bladder. It is more frequent in men, and the most common etiology is benign due to diverticulitis, followed by malignant etiology due to colon adenocarcinoma.2,3 The incidence of fistulae in patients with diverticular disease is 2%, and 0.6% in patients with colon adenocarcinoma.4
Diagnosis may be delayed due to the misleading symptoms, which are usually urinary. The best imaging test to identify this clinical situation is a computed tomography scan (CT).2,5,6
The differential diagnosis between colovesical fistulae of benign or malignant etiology can be difficult because the symptoms and complementary test results are similar. In addition, it is sometimes difficult to obtain a biopsy to confirm malignancy. Although the literature does not specify what percentage of cases are surgical, authors agree that this is the ideal treatment in almost all cases. Laparotomy or laparoscopy can be used, which is associated with total or partial resection of the bladder in many cases.3,6,7
Our study aims to describe a case series of patients who underwent surgery for a benign or malignant colovesical fistula, and to assess the applicability of the laparoscopic approach in both groups.
MethodsWe carried out a descriptive study of 34 patients diagnosed with colovesical fistula who had been treated surgically at our hospital from January 2001 to March 2018. We included patients treated on an elective (28) or urgent (6) basis. Patients with benign or malignant colovesical fistula were grouped according to their diagnosis based on complementary tests, including abdominal CT scan, colonoscopy and cystoscopy.
We initially decided to perform a laparoscopic approach in patients diagnosed with benign or malignant colovesical fistula in whom imaging tests showed no suspected involvement of the trigone of the urinary bladder or the retroperitoneal plane. These were also elective surgeries in patients whose clinical conditions allowed for a laparoscopic approach.
Data were collected on age, sex, symptoms, diagnostic tests, preoperative risk, comorbidities, cause of colovesical fistula, type of approach, procedure performed, postoperative hospital stay, early and late complications, recurrence and mortality.
This study has been approved by the Ethics Committee of our hospital.
ResultsA total of 34 patients who had undergone surgery for colovesical fistula were included in the study: 13 cases (38%) associated with a benign cause (diverticulitis), and 21 cases (62%) with a malignant cause (adenocarcinoma of the colon).
Colovesical fistula had been suspected in 27 cases after abdominal CT scan, colonoscopy and cystoscopy, and then later confirmed in 34 by the pathology study of the surgical specimen.
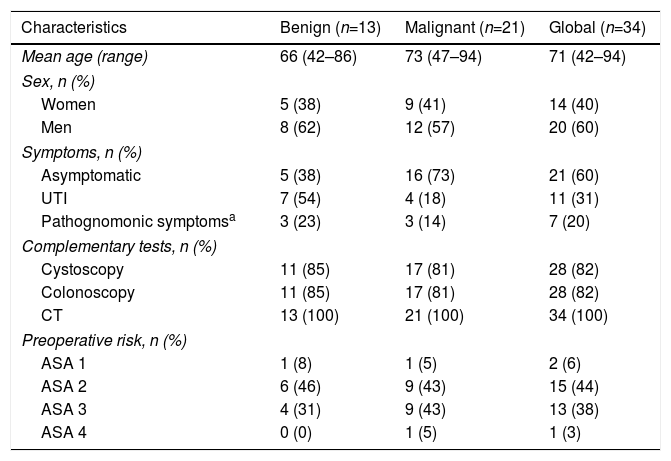
The mean age of the series was 71±13 years, and there was a predominance of men (60%) versus women (40%) (Table 1).
Characteristics of Patients With Colovesical Fistula due to Benign or Malignant Causes.
| Characteristics | Benign (n=13) | Malignant (n=21) | Global (n=34) |
|---|---|---|---|
| Mean age (range) | 66 (42–86) | 73 (47–94) | 71 (42–94) |
| Sex, n (%) | |||
| Women | 5 (38) | 9 (41) | 14 (40) |
| Men | 8 (62) | 12 (57) | 20 (60) |
| Symptoms, n (%) | |||
| Asymptomatic | 5 (38) | 16 (73) | 21 (60) |
| UTI | 7 (54) | 4 (18) | 11 (31) |
| Pathognomonic symptomsa | 3 (23) | 3 (14) | 7 (20) |
| Complementary tests, n (%) | |||
| Cystoscopy | 11 (85) | 17 (81) | 28 (82) |
| Colonoscopy | 11 (85) | 17 (81) | 28 (82) |
| CT | 13 (100) | 21 (100) | 34 (100) |
| Preoperative risk, n (%) | |||
| ASA 1 | 1 (8) | 1 (5) | 2 (6) |
| ASA 2 | 6 (46) | 9 (43) | 15 (44) |
| ASA 3 | 4 (31) | 9 (43) | 13 (38) |
| ASA 4 | 0 (0) | 1 (5) | 1 (3) |
ASA: American Society of Anesthesiologists; UTI: urinary tract infection; CT: computed tomography.
Most of the patients were classified as ASA 2 (44%) and ASA 3 (38%), although more than half did not present comorbidities.
In patients with a benign cause for colovesical fistula, the mean age was 66±12 years, and the majority were men (62%). The onset symptoms were urinary in more than half of the patients, while 38% (5) had no symptoms.
In patients with malignant colovesical fistula, the mean age was 73±10 years, and more than half were men. Most of the patients had no symptoms (73%), while anemia was the most common sign and the main reason for the study.
The diagnosis was made by abdominal CT scan, colonoscopy and cystoscopy. In 2 cases of fistula of benign cause and in 4 of malignant cause, colonoscopy and cystoscopy could not be performed since occlusion or perforation required urgent surgery.
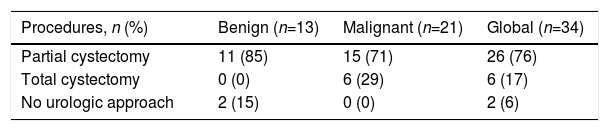
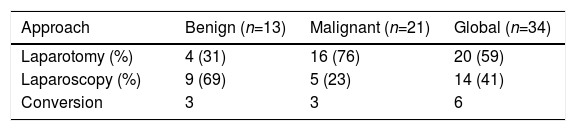
In cases with benign pathology, 4 procedures were performed via laparotomy and 9 by laparoscopy, 3 of which required conversion to laparotomy. Sigmoidectomy was performed in all cases, in 2 cases with end colostomy as they were emergency interventions and the clinical conditions of the patients did not allow for anastomosis to be performed.
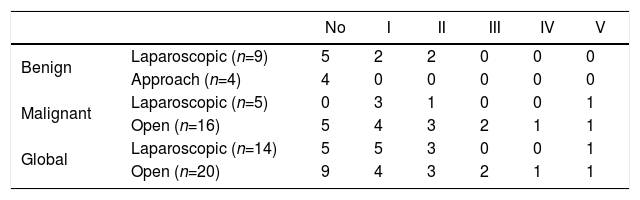
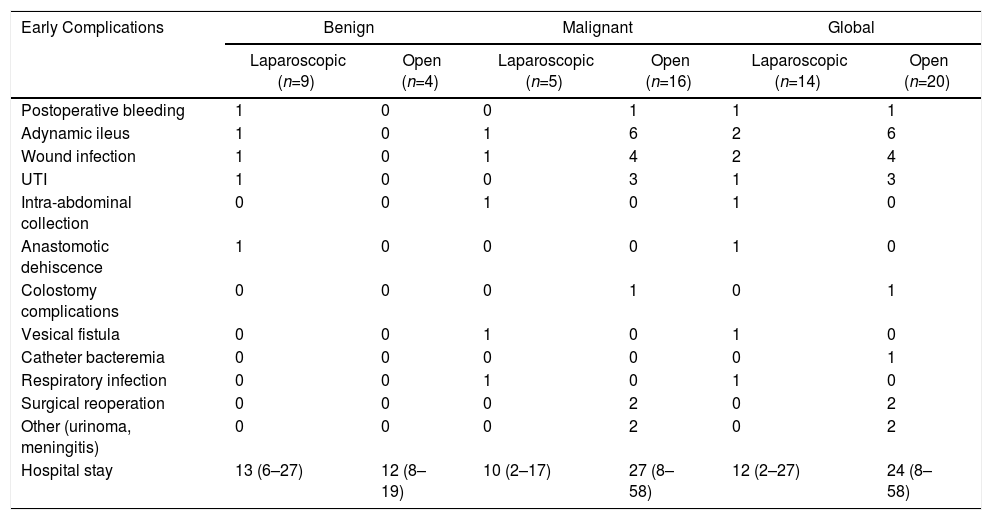
In 11 cases, a partial cystectomy was also performed: in 4 cases, it was completed by laparoscopy, and 3 cases required conversion to laparotomy. In 2 patients, it was not necessary to carry out a urological approach (Table 2), and conservative management was performed with a bladder catheter. Postoperative complications were not observed in 69% of the patients. Four cases had Clavien-Dindo I–II complications, all of which had been treated with laparoscopy (Table 3). The mean postoperative hospital stay was 13±7 days: 13±8 days in the patients treated laparoscopically, and 12±5 days in patients who underwent laparotomy (Table 4).
Results of Patients with Colovesical Fistula, of Benign or Malignant Cause, Treated with Laparoscopic or Open Surgery.
| Early Complications | Benign | Malignant | Global | |||
|---|---|---|---|---|---|---|
| Laparoscopic (n=9) | Open (n=4) | Laparoscopic (n=5) | Open (n=16) | Laparoscopic (n=14) | Open (n=20) | |
| Postoperative bleeding | 1 | 0 | 0 | 1 | 1 | 1 |
| Adynamic ileus | 1 | 0 | 1 | 6 | 2 | 6 |
| Wound infection | 1 | 0 | 1 | 4 | 2 | 4 |
| UTI | 1 | 0 | 0 | 3 | 1 | 3 |
| Intra-abdominal collection | 0 | 0 | 1 | 0 | 1 | 0 |
| Anastomotic dehiscence | 1 | 0 | 0 | 0 | 1 | 0 |
| Colostomy complications | 0 | 0 | 0 | 1 | 0 | 1 |
| Vesical fistula | 0 | 0 | 1 | 0 | 1 | 0 |
| Catheter bacteremia | 0 | 0 | 0 | 0 | 0 | 1 |
| Respiratory infection | 0 | 0 | 1 | 0 | 1 | 0 |
| Surgical reoperation | 0 | 0 | 0 | 2 | 0 | 2 |
| Other (urinoma, meningitis) | 0 | 0 | 0 | 2 | 0 | 2 |
| Hospital stay | 13 (6–27) | 12 (8–19) | 10 (2–17) | 27 (8–58) | 12 (2–27) | 24 (8–58) |
UTI: urinary tract infection.
In the 21 patients with malignant pathology, 5 procedures were performed by laparoscopy and 3 patients were converted to guarantee oncological criteria. Sixteen procedures were conducted by means of laparotomy. The procedures performed were 13 sigmoidectomies (6 with end colostomy), 4 open pelvic exenterations, one left hemicolectomy with end colostomy and 3 anterior resections (2 with end colostomy) (Tables 5 and 6). End colostomy was performed in 56% of the patients: pelvic exenterations and those who underwent emergency surgery and with a significant inflammatory component during surgery in whom anastomosis could not be performed safely.
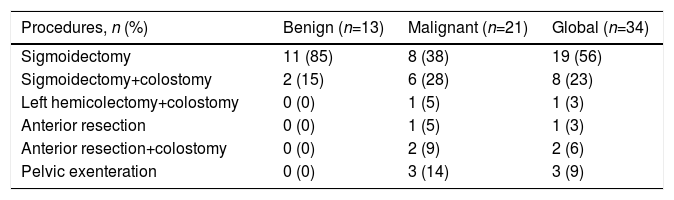
Surgical Procedures: Colon Resection.
| Procedures, n (%) | Benign (n=13) | Malignant (n=21) | Global (n=34) |
|---|---|---|---|
| Sigmoidectomy | 11 (85) | 8 (38) | 19 (56) |
| Sigmoidectomy+colostomy | 2 (15) | 6 (28) | 8 (23) |
| Left hemicolectomy+colostomy | 0 (0) | 1 (5) | 1 (3) |
| Anterior resection | 0 (0) | 1 (5) | 1 (3) |
| Anterior resection+colostomy | 0 (0) | 2 (9) | 2 (6) |
| Pelvic exenteration | 0 (0) | 3 (14) | 3 (9) |
In 21 cases, a urological approach was necessary: partial cystectomy was performed in 15 patients (2 cases were completed by laparoscopy), and total cystectomy with Bricker reconstruction was performed in 6 (Table 2).
Sixteen patients (76%) presented complications, and most were treated with laparotomy. Eleven patients (52%) presented minor complications (I–II) according to the Clavien-Dindo classification, and 5 (24%) presented major complications (III, IV and V) (Table 3).
The average postoperative hospital stay was 23±15 days, although the mean stay was shorter in patients who underwent laparoscopy at 10±5 days. In patients with laparotomy, the average stay was 27±15 days (Table 4).
DiscussionColovesical fistula is a very rare entity. At our hospital, out of the 3400 patients treated surgically for colon pathology in 17 years, only 35 cases have been observed.2
Despite the fact that in the literature diverticulitis is considered the most common cause of colovesical fistula (50%–70%), the most frequent cause in our series was adenocarcinoma of the colon (63%), which is reported in 20% in the literature. This is probably due to the characteristics of our population, with a mean age that was older than in other series.8
The diagnosis is based on urinary infection symptoms and pathognomonic signs, such as fecaluria and pneumaturia. The presence of air in the bladder on abdominal CT scan would confirm this diagnosis.3,6,9 In our series, most patients had no symptoms of urinary tract infection (11.32%) or pathognomonic signs of fistula (7 patients, 21%). Asymptomatic patients were identified in both groups (in fistulae of benign origin 5.38% and in fistulae of malignant origin 16.76%), whose CT study was motivated by laboratory findings. Because certain symptoms of patients with colovesical fistula are unclear, clinical suspicion is crucial, followed by complementary tests aimed at identifying the cause of the colovesical fistula.4,7 Abdominal CT scan is the imaging test of choice for diagnosis, since it provides better visualization of the anatomical structures and the degree of pelvic inflammation, helping to determine the best time for a surgical intervention.3,4,8 Colonoscopy is important to identify the cause, but in many cases this diagnosis is difficult due to the impossibility of completing a colonoscopy or obtaining a biopsy that confirms adenocarcinoma due to the important inflammatory signs that may accompany the colovesical fistula. In our series, the study could not be completed with colonoscopy and cystoscopy in patients who required urgent surgical intervention due to occlusion or perforation.5,6,8,10
A colovesical fistula requires a surgical approach for its treatment, and conservative management is relegated to patients at high risk for anesthesia. There is limited consensus in the literature on the management of bladder repair, and some authors, such as Bertelson et al.,2 advocate conservative management with a urinary catheter if the etiology of the fistula is benign and the defect is small.10,11 In some selected cases in which a benign origin is suspected, simple colon resection can be done without intervention on the bladder; however, in most cases, either due to suspected malignancy or the presence of inflammatory signs, partial or total bladder resection is required. For this reason, the participation of the urology team is necessary.4,6,7,9
Regarding the surgical approach to colorectal disease, laparoscopy has been established as the gold standard for the treatment of diverticular disease and colon cancer. In the context of the chronic inflammation that accompanies colovesical fistulae, the laparoscopic approach is not yet well established or recommended in the literature. In our study, we have only been able to complete a laparoscopic approach in 8 patients (24%), with a high conversion rate (3 patients [33%] in benign cases, and 3 patients [50%] in malignant cases). Thus, although this approach is complicated in cases of advanced adenocarcinomas and inflammatory changes after episodes of diverticulitis, with adequate patient selection the laparoscopic approach may be feasible.9,12,13 The most recently published series on colovesical fistula report laparoscopic approach rates between 30% and 100% and conversion rates from 10% to 30%, without differentiating the origin of the fistula.7,11,13–15 The most significant series are the study by Aydinli et al.,9 with 512 patients (473 with fistula of benign origin and 30% undergoing laparoscopy) and the study by Cirocchi et al.,11 with 202 cases of fistulae of benign origin (all of whom underwent laparoscopic surgery). Recently, Tomizawa et al.12 (2019) have published a retrospective descriptive study of 39 cases with colovesical fistula due to diverticulitis treated laparoscopically, without conversion to laparotomy as they were selected cases.
Our data are not comparable to these series due to their heterogeneity. However, in general terms, the percentage of patients who underwent laparoscopy in our series was lower and the conversion rate higher, probably due to cases of advanced neoplasm and diverticular disease with complex fistula and chronic inflammation.
In our series, the morbidity of patients undergoing laparoscopy is acceptable (8 cases with Clavien-Dindo I–II complications, 4 in each group) and the registered mortality is low, with 2 cases described (6%): one due to medical complications, and the other due to septic shock during the postoperative period because of multiple organ failure.
The main limitation of this paper is that it is a series of few cases with a 17-year follow-up, during which the laparoscopic approach was routinely implemented at our hospital.
Despite the fact that the existence of colovesical fistula is considered a risk factor for conversion by some authors, the laparoscopic approach may be applicable to maintain the advantages of minimally invasive surgery.11,16–21 The authors agree that this approach should be performed by trained surgeons; greater experience and improved laparoscopic technology will likely facilitate the applicability of the laparoscopic approach in this abnormality.11,12,14,15,17
In conclusion, surgical procedures for colovesical fistula can be difficult, as many patients present a significant inflammatory component. Several authors agree that the laparoscopic approach may be applicable in this pathology when performed by an experienced team and in the context of multidisciplinary treatment, providing a less invasive approach but also taking into account that the conversion rate can be high.
Conflict of InterestThe authors have no conflict of interest to declare.
Please cite this article as: de la Fuente Hernández N, Martínez Sánchez C, Solans Solerdelcoll M, Hernández Casanovas P, Bollo Rodríguez J, Gaya Sopena JM, et al. Fístula colovesical: aplicabilidad del abordaje laparoscópico y resultados según su etiología. Cir Esp. 2020;98:336–341.